Abstract
Abstract 4113
Despite the raise of major new drugs in the management of multiple myeloma (MM), it is still an incurable disease and allogeneic stem cell transplantation (alloSCT) is currently the sole potential curative therapy mediated by a graft-versus-myeloma (GVM) effect. For over ten years, reduced intensity conditioning regimens (RIC) in alloSCT has been developed to maintain the GVM effect and to decrease the high transplanted related mortality (TRM) associated with myeloablative conditioning (MAC) in myeloma patients. Yet, as numerous studies have assessed RIC alloSCT versus autologous SCT, only few data provides a comparison between RIC and MAC for MM in large series. Our study aims to compare RIC and MAC alloSCT for MM on a large retrospective French cohort.
We report a retrospective multicenter study based on the Société Française de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC) registry, evaluating the outcome of patients undergoing alloSCT for MM. Between 1995 and 2009, 811 patients allografted for MM were registered. Data concerning disease characteristics and the allograft procedure were screened using the French Promise® database; computerized discrepancy errors and data verification of every single file ensure data quality, important missing data were directly retrieved in each centre.
We assign the type of conditioning regimen for each patient according to the registry's data reported by the local physician and check this information according to the following rules. We consider as myeloablative (MAC) all regimens containing > 8 mg/kg oral busulfan, > 600 cGY TBI, ≥ 200 mg/kg cyclophosphamide or combinations as BEAM like regimens. All other chemotherapy combinations with or without TBI are defined as RIC regimens generally including fludarabine. Patients were excluded when major data or conditioning information were not available; 566 patients (70% of the entire cohort) were finally eligible for analysis, 478 RIC and 88 MAC.
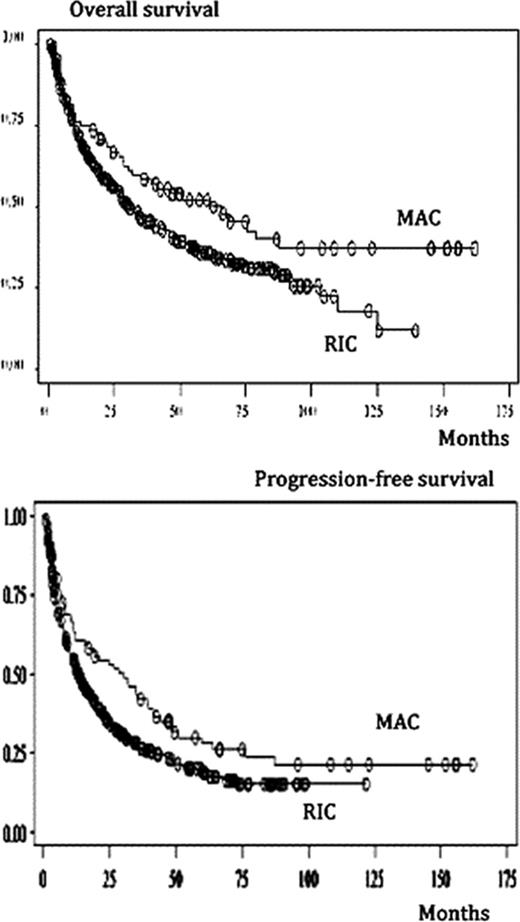
Chi-squared test and T-test were used for comparisons. Survival analyses (Overall survival, OS; progression-free survival, PFS) are made using the Kaplan-Meier curve and log rank test. Multivariate analysis is made using the Cox proportional hazards model.
The RIC and MAC populations were statistically different regarding age (respectively 53 versus 46 years, p<.0001), number of prior transplant (> 1 prior transplant in 94% RIC versus 77% MAC, p<.0001), time to transplantation (<12 months after diagnosis in 22% RIC versus 38% MAC, p=.001) and stem cell source (peripheral blood 84% RIC versus 52% MAC, p<.0001, and bone marrow 10% RIC versus 45% MAC, p<.0001).
The 2-year OS is 69.5% after RIC and 79.9% after MAC (p<.0001); 5-year OS is 49.7% after RIC and 60.2% after MAC (p<.0001, fig.1). The 2 year PFS is 49.3% and 70.1% and 5-year PFS is 29.6% and 40.8% after RIC and MAC respectively (p<.0001, fig.2).
Factors associated with better OS and PFS in multivariate analysis are the following in the whole cohort: < 12 months between diagnosis and alloSCT (p=.0078 and p=.0037, respectively); disease status at transplantation (at least partial response, p=.0409 and p=.0026); no or limited acute graft-versus-host disease (GvHD) (p<.0001 and p=.0094) and presence of chronic GvHD (p<.0001 and p<.0001). On multivariate analysis, the intensity of conditioning regimen (RIC vs MAC) do not appear statistically significant for OS (p = 0.64) and PFS (p = 0.17). For patients transplanted between 2006 and 2009, neither high risk-cytogenetic nor bortezomib use before transplantation seems to affect the outcome in multivariate analysis.
Conclusions: In the French practice, MAC regimens have had more limited indications due to their higher toxicity. This study suggests that the outcome after MAC-alloSCT is comparable to that after RIC-alloSCT with a trend to a better OS in the late follow-up (after 5 years) after MAC. The aspect of flattening in the survival curves suggests that the anti-tumoral action of the conditioning regimen remains essential on the anti-myeloma effect after alloSCT and that should be considered in the transplantation procedure.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.