Abstract
Abstract 4118
Despite the advent of novel agents, outcomes of T cell Lymphoma (TCL) with conventional chemotherapy are poor. We have previously reported (Rodriguez J, JCO 2001) encouraging results with autologous stem cell transplantation (ASCT). Others have advocated allogeneic transplants (Allo-SCT). Herein, we report our long-term experience in 196 TCL patients (pts) who had either ASCT (n=119) or Allo-SCT (n=77).
This is a retrospective analysis of TCL pts treated with SCT at our institution between 1986 and 2009. We adopted WHO 2008 classification for TCL and divided pts accordingly into Nodal TCL (N-TCL), extra nodal TCL (EN-TCL), and T cell lymphoblastic Lymphoma (T-LBL). Sixty one pts (31%) had peripheral t-cell not otherwise specified (PTCL), 50 (26%) had anaplastic large cell (ALCL), 19 (10%) angioimmunoblatic (AITL), 34 (17%) EN-TCL, and 32 (16%) had T-LBL. ASCT and Allo-SCT pts were balanced for Ann-Arbor stage, gender distribution and time from initial diagnosis. However, Allo-SCT pts were younger (median age 41 vs. 49 yrs, respectively, (p=0.002), more heavily pretreated (p=0.01), were more likely to have extranodal (p<0.001) or bone marrow involvement (p=0.001), and refractory disease (p=0.01) at the time of transplant.
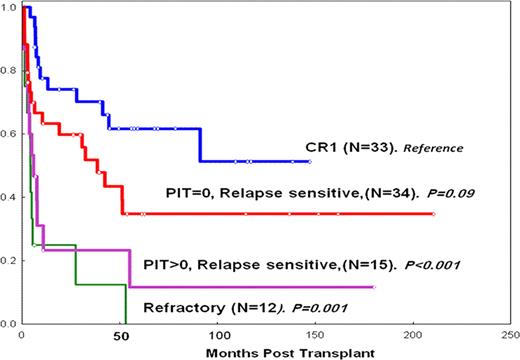
Most pts (82%)received BEAM-like conditioning. With a median follow-up of 39 months (range, 3–208), the OS and PFS rates were 39% and 30%, respectively. Risk factors for OS and PFS were evaluated among the largest histologic subgroups, i.e., PTCL, ALCL and AITL: among those 94 pts who received ASCT, having a transplant > CR1 (p=0.001), Prognostic Index for TCL(PIT) >0 (p=0.009), IPI>1 (p=0.03), refractory disease (p=0.001) were associated with worse OS and PFS (Figure 1). The 3-year OS and PFS for CR1 pts (n+33) were 90% and 70%, respectively. A subset of pts (n= 11) within the CR1 group received induction chemotherapy with Hyper-CVAD before ASCT. The 3-year OS and PFS rates for these pts were both 100%. We were not able to detect any difference in outcomes between the different histologies studied, including ALK(+) and ALK (−) ALCL. B. [Allo-SCT] Most pts (75%) received myeloablative conditioning. There was a trend for better outcomes for transplants > year 2000. With a median follow-up of 65 months (range, 5–235), the OS and PFS rates were 43% and 30%, respectively. OS and PFS rates for EN-TCL(n=18) were 49% and 36%, respectively. Among the N-TCL (n=33) group, unlike ASCT, most pts (87%) were >CR1. The 3-year OS and PFS rates for these pts were 38% and 23%, respectively. Both IPI and PIT >0 were determinants for worse PFS, whereas IPI >0 and marrow involvement were predictors for worse OS. No plateau however was observed in these pts, unlike those with T-LBL, where a clear plateau of 40 % was observed.
Autologous SCT for N-TCL: PFS Based on Disease Status and PIT at transplant
This is the largest single institution analysis to investigate the role of SCT for TCL. Our review demonstrates that ASCT can induce long-term remissions in CR1 pts with N-TCL. Prospective studies comparing ASCT in this setting to other conventional treatments are warranted. Although allo-SCT was found to be effective in T-LBL, its role in other forms of TCL is yet to be determined. Innovative strategies remain needed for pts with relapsed disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.