Abstract
Abstract 4490
Allogeneic hematopoietic stem cell transplantation (allo-SCT) may rescue patients with acute myeloid and lymphoblastic leukemia (AML/ALL) even in high risk disease. Little has been investigated about prognostic impact of pre- and post-transplant residual disease (RD) status, hematogones (HG) level and natural killer (NK) cells level in the adult patients with acute leukemia.
We retrospectively studied 45 consecutive adult patients, including 31 AML and 14 ALL, receiving allo-SCT at National Taiwan University Hospital. Based on disease status at transplant, 18 patients were in standard risk; 16 in intermediate risk; and 11 in high risk disease. 28 patients underwent myeloablative conditioning and 17 received reduced-intensity SCT. Bone marrow samples were obtained both before conditioning therapy (pre-SCT) and at hemogram recovery after transplantation (post-SCT). RD, HG level and NK cells level were evaluated by multidimensional flow cytometry. Leukemia-free survival (LFS) was estimated by using Kaplan-Meier method.
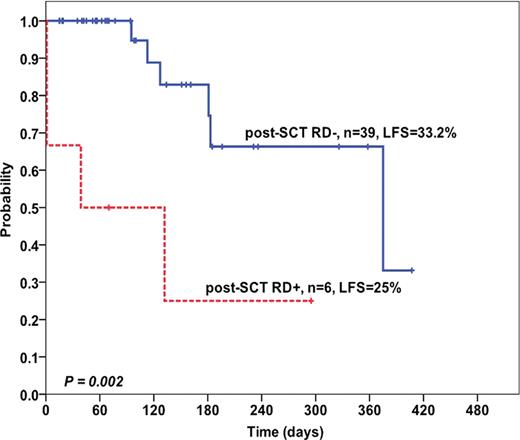
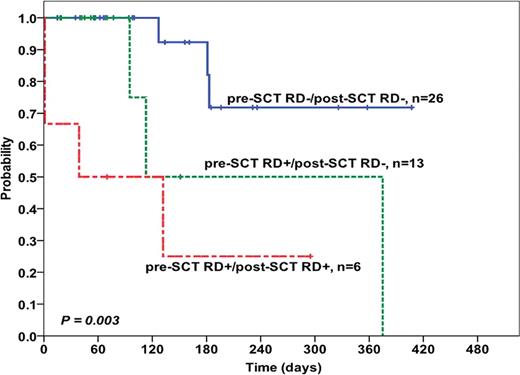
Pre-SCT RD-negative (RD-) was shown in 26 patients and RD-positive (RD+) in 19 patients; whereas post-SCT RD- was found in 39 patients and RD+ in 6 patients. Level of pre-SCT RD status ranges from 0–90% and level of post-SCT RD status ranges from 0–3%. Estimated one-year LFS were 71.8% in pre-SCT RD- compared to 0% in pre-SCT RD+ group (P=0.008, Fig. 1). In post-SCT flow cytometric analysis, one-year LFS were 33.2% in post-SCT RD- versus 25.0% in post-SCT RD+ group (P=0.002, Fig. 2). After combining pre- and post-SCT RD status, three groups of patients were identified; pre-SCT RD−/post-SCT RD- (n=26), pre-SCT RD+/post-SCT RD- (n=13), and pre-SCT RD+/post-SCT RD+ (n=6). The classification further stratify the patients into different groups with distinct outcome (P=0.003, Fig. 3). We also found the median HG 0.2% (range 0–12%) and 0.1% (range 0–2.1%) and median NK cells 1.8% (range 0.2–20%) and 1.8% (0.02–15.5%) pre-SCT and post-SCT, respectively. The patients with higher NK cells, either pre-SCT or post-SCT, had longer LFS (P<0.001 and 0.004, continuous variables, respectively).
Leukemia-free survival according to pre-SCT RD status
Leukemia-free survival according to post-SCT RD status
Leukemia-free survival according to stratification of pre-SCT & post-SCT RD status
Leukemia-free survival according to stratification of pre-SCT & post-SCT RD status
Our data suggest both pre- and post-SCT RD status and NK cells level could predict the transplant outcome. Further large-scale studies may be needed to confirm this point.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.