Abstract
Abstract 843
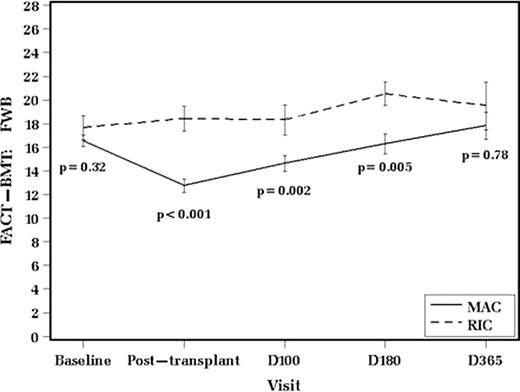
Allogeneic hematopoietic stem cell transplantation (Allo-HSCT) following reduced intensity conditioning (RIC) compared to myeloablative conditioning (MAC) results in less treatment related morbidity and mortality. RIC permits older and less healthy patients (pts) to undergo Allo-HSCT. Whether RIC is also associated with better quality of life (QOL) and psychosocial functioning (PF) among pts with myeloid malignancies has not been systematically analyzed. We prospectively collected QOL and PF outcomes in 192 consecutive pts with AML (n=130), MDS (n=52), or myeloproliferative neoplasms (n=10) who received MAC (n=154) or RIC (n=38) Allo-HSCT from 2004 to 2010. Psychometric data were assessed longitudinally (at baseline, post-transplant, day100, 180, and 365) by validated questionnaires (Functional Assessment of Cancer Therapy- Bone Marrow Transplant Scale [FACT-BMT], coping inventory [Brief COPE], and Profile of Mood States Short Form [POMS]). FACT-BMT consisted of individual and summary scores for physical (PWB), social (SWB), emotional (EWB), functional (FWB) well-being along with additional concerns (AC). Brief COPE has 14 components such as use of emotional and instrumental support, venting, positive reframing etc. POMS consisted of 6 components such as depression, vigor, anger etc. Secondary endpoints included overall survival (OS), relapse-free survival (RFS), incidence of acute (aGVHD) and chronic (cGVHD) graft vs. host disease. QOL and PF differences were compared between transplant types over time by repeated measures analysis of variance. Adjustment for baseline differences in QOL and PF was made in mixed linear model analysis. Kaplan-Meier and cumulative incidence methods were used for analyses of secondary endpoints. RIC and MAC patients were comparable (all p>0.1) for gender, race, hematopoietic cell transplantation comorbidity index, number of prior chemotherapies, donor relation, length of follow up. Differences between RIC and MAC groups (all p<0.001) were detected for median age at transplant (61 for RIC vs. 48 yrs for MAC), stem cell (SC) source (95% peripheral SC in RIC vs. 19% in MAC), TBI-containing preparative regimen (95% for RIC vs. 24% for MAC), CD34+ dose (5.2 for RIC vs. 2.2 ×106/kg for MAC), GVHD prophylaxis. RIC pts had shorter median time-to-neutrophil (11 vs. 15 days, p<0.001) and -platelet (12 vs. 21 days, p<0.001) recovery. There was no baseline QOL difference between RIC and MAC according to FACT-BMT. RIC pts had better baseline scores for anger, emotional support use, venting, and positive reframing (all p<0.05). As compared to MAC, pts with RIC had superior QOL scores post-transplant, i.e FWB (up to day 180, p<0.01), AC (up to day 100, p<0.05), and summary (up to day 100, p<0.05) despite the absence of baseline differences. FWB advantage of RIC remained significant up to half a year (p<0.05) in mixed linear model analysis adjusted for baseline differences. RIC pts had better depression (p<0.01) and anger (p<0.01) scores post-discharge after controlling for baseline differences. In adjusted analysis of COPE, RIC pts had better positive reframing (p=0.02) and use of instrumental support (p=0.02) during early post-transplant follow up. All QOL and PF metrics equalized between RIC and MAC by post-transplant day365 (all p>0.1). With a median follow up of 34 months, there were no differences between RIC and MAC in incidence of aGVHD or cGVHD, RFS, or OS (all p>0.3). In conclusion, our prospective study provides further evidence on overall comparable clinical, QOL and PF outcomes between RIC and MAC and it is the first to demonstrate significant early advantage of RIC in certain QOL and PF metrics up to 180 days post-transplant across all three psychometric instruments.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011