Abstract
Abstract 995
N-terminal fragment of BNP (NT-proBNP) and cardiac troponin –T (TnT) or I (TnI) form a useful staging system in AL amyloidosis and poor outcomes have been reported in stage III patients treated before routine use of novel agents. These patients are routinely excluded from clinical trials and prospective outcome data is limited but recent studies suggest that some such patients may have better outcomes. We report the outcomes of 347 patients with Mayo stage III AL amyloidosis seen at the amyloid centres in London (UK), Pavia (Italy), Heidelberg (Germany) and Athens (Greece). Organ involvement and responses are defined according to 2005 amyloidosis consensus criteria. Presenting features were [n (%)/median (range)]: cardiac, renal and liver involvement in 338 (97%), 216 (62%) and 77 (22%) respectively, NT-proBNP 9106 ng/L (379–216187); TnI – 0.18 ng/ml (0.1–12); TnT −0.09 ng/ml (0.04–8.2) and IVS 15 mm (7–24). Treatments given were: Bortezomib combinations - 23 (7%), MDex - 150 (43%), thalidomide combinations - 96 (28%), lenalidomide combinations - 13 (4%). 30 (8%) were deemed too ill for treatment or died prior to treatment initiation. Only 37% completed the planned treatment course. The haematological responses on an intention to treat basis were seen in (Overall response rate/complete response (CR)/partial response (PR))(n(%)): MDex – 63(42%)/24 (16%)/39 (26%); Thalidomide combinations 31(32%)/11(12%)/20(21%), bortezomib combinations 10(43%)/6 (23%)/4 (17%), lenalidomide combination 5(38%)/0(0%)/5(38%).
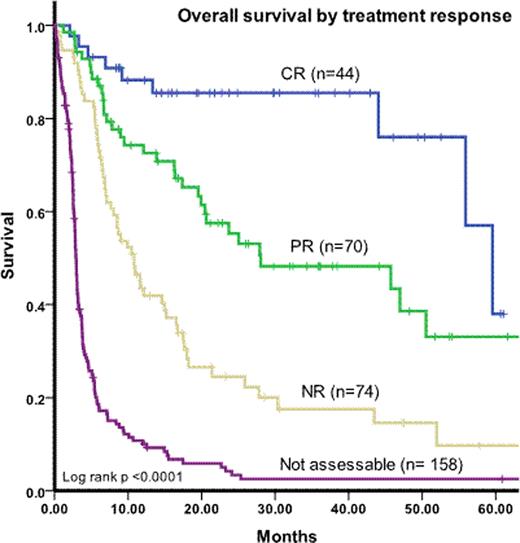
The median overall survival (OS) was 7.1 mos. The overall survival at 12 months from response evaluation was 74% for CR, 52% for PR and 18% for NR and from diagnosis was (median): CR – 59 mo, PR 28 mo, NR 10 mo and not assessable for response 2.9 mos. Stage III patients without echocardiographic evidence of cardiac involvement had excellent outcomes with 80% estimated 2 year OS. Using best fit cut-off, in multivariate model (including NT-proBNP., systolic blood pressure (SBP), ejection fraction, NYHA, ECOG, dFLC, LV wall thickness), NT-proBNP > 8000 ng/L (HR 2.3; p <0.0001) and SBP < 100 mm of Hg (HR 1.6; p<0.0001) were the only independent predictors of poor outcome. Using NT-proBNP >8000 ng/L and SPB <100 mm of Hg as high risk criteria, stage III patients can be further subdivided based on presence of none, one or two criteria with OS of 25 mo, 6 mo and 3 mo respectively. Using these criteria, on intent to treat basis, OS by CR/PR/NR was: no high risk factors – median not reached/69 mo/7 mo and one high risk factor - 59 mo/23 mo/4 mos respectively and too few patients for patients with two high risk factors making comparison unreliable.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.