In 2 patients with As2O3-refractory acute promyelocytic leukemia (APL), Goto et al identified missense mutations in the PML-region B2-box domain that neighbor the dicysteine motif recently found to be critical for PML-RARα degradation, a requirement for curative anti-APL effect.1
As2O3 has emerged as the most clinically effective agent in APL (reviewed in Chen et al2 ). Like the antecedent agent all-trans retinoic acid (ATRA) that targets PML-RARα, the underlying pathogenetic driver in APL, primary resistance to remission induction is extremely rare. Its superiority to ATRA is demonstrated by the capacity of As2O3 to produce sustained remissions and apparent disease cure even when administered as a single agent in the majority of cases. When relapse occurs after As2O3 treatment, second and additional remissions can usually be achieved, however, these secondary remissions become progressively less durable. This pattern of resistance development suggests a pharmaco-metabolic basis for the development of clinical resistance to As2O3.3 Similarly, clinical ATRA resistance was demonstrated to have a pharmaco-metablolic component, but when the dose-schedule was adjusted to avoid tachyphylaxis, the only established mechanism of clinical ATRA resistance is the acquisition of mutations in the RARα-region ligand binding domain (LBD) of PML-RARα.4 Now, Goto et al report the first molecular basis for clinical resistance to As2O3 in APL, missense mutations in the PML-region B2-box domain of PML-RARα.1
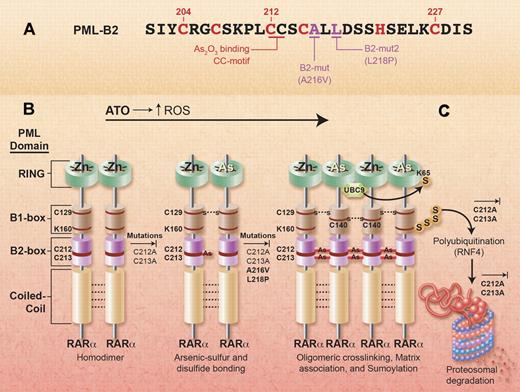
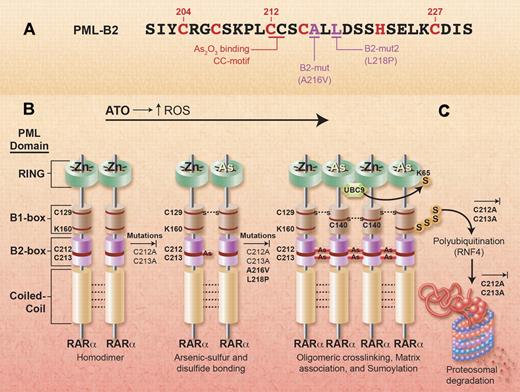
The findings of Goto et al indicate that clinically administered As2O3 was able to select APL cells with mutations in critical PML-RARα target sites, despite pharmacokinetic studies indicating that in Japanese patients the reactive trivalent form of arsenic only reaches low nanomolar concentrations in plasma.5 Thus, these findings provide critical support for the clinical relevance of a molecular model of As2O3 action developed in preclinical investigations conducted at much higher (≥ 1μM) As2O3 concentrations (reviewed in Chen et al2 ). As shown in the figure, PML-RARα exists as predominant homodimers in APL cells because of intermolecular noncovalent bonding of coiled-coil domains, the third component of the tripartite RBCC (Ring/B-box/Coiled Coil) domain at the PML-region amino-terminus. Exposure to As2O3 produces 2 primary effects that lead to covalent cross-linking of individual PML-RARα molecules. First, As2O3 produces an increase in reactive oxygen species (ROS), related both to the poisoning of ROS scavenger enzymes by enhancing disulfide bond formation in cysteine residues and to the generation of increased amounts of neutrophil-associated NADPH oxidase (reviewed in Sumi et al6 ). The increase in oxidative state also augments disulfide bond formation in many other redox-sensitive proteins, including intermolecular cross-linking of cysteine residues in PML-RARα homodimers.2,7 Second, As2O3-derived arsenic (As) atoms were recently shown to directly bind to PML-RARα, partly by replacing zinc atoms in the RING domain zinc fingers and partly by covalent bond formation with the sulfhydryl groups of the only dicysteine motif in PML, C212 and C213.2,7 The latter, which likely involves cross-linking via 2 As atoms, was shown to be crucial, because mutation of either C212 or C213 eliminated As binding and abrogated most downstream effects of As2O3 exposure, including nuclear matrix association, sumoylation, polyubiquitination, and proteosomal degradation of PML-RARα (see figure).7 Thus, the novel finding of mutations 3 and 5 amino acid positions removed from the crucial dicysteine motif in As2O3-resistant APL cells (A216V and L218P) strongly supports the hypothesis that the APL cellular resistance resulted from impairment of the defined sequence of events necessary for PML-RARα degradation, which, in turn, has been shown to be of central importance for the elimination of APL leukemia-initiating/propagating cells in preclinical models (reviewed in Chen et al2 ).
Mutations in As2O3-refractory APL support clinical relevance of experimental model of As2O3 action. (A) B2-Box missense mutation sites from Figure 1D in the article by Goto et al that begins on page 1600. (B-C) Relationship of As2O3 resistance-associated mutations (A216V and L218P) to preclinical model for As2O3-mediated PML-RARα degradation: all steps blocked by experimental site-specific mutation of the critical arsenic-binding/cross-linking dicysteine motif (C212A or C213A; Jeanne et al7 ); matrix association and sumoylation demonstrated to be blocked by A216V and L218P. Adapted from Jeanne et al7 with copyright permission from Elsevier. Professional illustration by Alice Y. Chen.
Mutations in As2O3-refractory APL support clinical relevance of experimental model of As2O3 action. (A) B2-Box missense mutation sites from Figure 1D in the article by Goto et al that begins on page 1600. (B-C) Relationship of As2O3 resistance-associated mutations (A216V and L218P) to preclinical model for As2O3-mediated PML-RARα degradation: all steps blocked by experimental site-specific mutation of the critical arsenic-binding/cross-linking dicysteine motif (C212A or C213A; Jeanne et al7 ); matrix association and sumoylation demonstrated to be blocked by A216V and L218P. Adapted from Jeanne et al7 with copyright permission from Elsevier. Professional illustration by Alice Y. Chen.
Considered in detail, the experiments performed by Goto et al demonstrate that the A216V and L218P mutations prevent matrix association and consequent sumoylation of the mutant PML-RARα (see figure).1 Further experiments are required to assess the presumed effects on As2O3 binding and proteosomal degradation. The latter seems almost certain, because polyubiquitination by the E3 ligase RNF4 required for proteosomal degradation is sumoylation-dependent. However, inhibition of As2O3 binding by a configurational mutation effect seems less certain, because the exact mechanism by which ATO binding activates sumoylation has not been determined, although this involves enhanced recruitment of the E2 sumo conjugase UBC9.2,7 2 other questions posed by details of the Goto et al report merit further investigation: (1) How does the apparently cytoplasm-restricted S-form PML-RARα in patient 1 (A216V) relate to the above model entirely developed with nuclear L-form PML-RARα? (2) What is the basis of the dissociated clonal relationships of the B2-box and LBD mutations in patient 1? In this long-term As2O3-treated patient, could this represent a genotoxic effect related to the clastogenic activity of As2O3, which can produce large deletions and chromosome rearrangements?8
The reported presence of B2-box mutations in the only 2 patients refractory to As2O3 induction among 15 patients studied, despite marked differences in clinical circumstances,1 renders such mutations suspect in any APL patient who progresses on active As2O3 therapy. However, the incidence and broader clinical importance of the mutations remains to be determined. One patient (1; A216V) had been repeatedly treated with As2O3 over 7 years with diminishing success, and the mutation was not detected until the last few months associated with increased refractoriness. Thus, the resistance to As2O3 in this case was likely complex, and, although the mutation was apparently required for sufficient loss of response for disease expansion on As2O3, such late-arising mutations might only develop in a fraction of extensively treated, As2O3-resistant patients. In contrast, the second patient (6; L218P) had not received As2O3 treatment before its instigation for a second clinical relapse. Although incompletely documented, the scenario presented in this case plausibly indicates that As2O3 treatment can select a minor pre-existing APL subclone harboring the mutation leading to disease expansion and relapse.1 However, the incidence of such mutations may be low even in the small fraction of As2O3-naive multiple-relapse cases who are subsequently treated with and fail As2O3 treatment: Gurrieri et al previously reported the absence of PML-region PML-RARα mutations using single-strand conformational polymorphism analysis of DNAs from 8 multiple-relapse APL patients, including relapse after As2O3 therapy (see Table 1 in Zhou et al9 ).10 Clearly, more extensive screening for these mutations is needed to determine the incidence of these mutations under different clinical circumstances.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■