Abstract
Beyond providing a scaffold for immune cells, recent studies indicate that lymph node stromal cells provide potent regulatory capacities that affect the quality of adaptive immune responses. In this study, we provide evidence that neonatal lymph node stromal cells (nnLNSCs) consistently promote the differentiation of macrophage dendritic cell progenitors as well as mature and immature dendritic cells into a distinct population of CX3CR1+ CD11b+F4/80+ regulatory macrophages (regMΦ). These cells possess remarkably low levels of T cell costimulatory molecules as well as MHC class II molecules. regMΦ do not interfere with early T-cell activation but, via nitric oxide secretion, efficiently suppress T-cell proliferation. Furthermore, CD4+ T cells proliferating in the presence of regMΦ gain immunosuppressive capacity and MΦ isolated from day 3 nnLNs are T-cell immunosuppressive. Adoptive transfer of antigen-loaded regMΦ induce a profound antigen-specific immune suppression in vivo. Together our data show that nnLNSCs skew the differentiation of dendritic cells and their progenitors toward regMΦ, thus revealing a novel mechanism for local immune regulation.
Introduction
Secondary lymphoid organs (SLOs) such as lymph nodes (LNs) develop during embryogenesis but continuously expand and reshape throughout the first weeks of life. After a series of highly coordinated reciprocal interactions between hematopoietic cells and mesenchymal stromal cells, SLOs gradually acquire their structural and functional maturation during the neonatal period.1 These interactions are primarily orchestrated by homeostatic chemokines, cytokines, and growth factors that attract hematopoietic cells to the sites of future lymphoid organ development and promote their survival and differentiation. In turn, lymphotoxin-expressing hematopoietic cells trigger the differentiation of stromal and endothelial cells that make up the scaffolding of SLOs.2 After final maturation, SLOs show a highly organized architecture composed of distinct cellular compartments and structures, at the heart of which are nonhematopoietic stromal cells.3-5 There is accumulating evidence that stromal cells play a key role in the functional organization of SLOs, such as organogenesis,6 migration of lymphocytes,7-9 naive T-cell homeostasis,10 and the progress of immune responses.11,12 We and others recently demonstrated that LN stromal cell–produced retinoic acid affects the expression of gut-homing adhesion molecules α4β7 integrin, as well as chemokine receptor CCR9.13,14
Dendritic cells (DCs) represent ubiquitous sentinels of the immune system possessing potent antigen presenting capacities. The maturation and activation status of DCs critically determines the response of T cells that they prime. Therefore, DCs are key players in initiating and shaping adaptive immune responses. They contribute to the functional differentiation of effector and regulatory T (Treg) cells, as well as the induction of central and peripheral tolerance.15,16
Given the importance of LN stromal cells for the function and organization of SLOs in adolescents and adults, we addressed in this study whether LN stromal cells of neonates (nnLNSCs) modulate immune responses. We evaluated the effect of stromal cells isolated from peripheral and mesenteric LNs of day 3 neonatal mice on the fate of macrophage DCs progenitors (MDPs),17 as well as on mature and immature DCs. Surprisingly, after coculture with nnLNSCs all of these cells underwent differentiation resulting in the formation of CX3CR1+ regulatory macrophages (regMΦ). Of note, these regMΦ exhibit a strong T-cell immunosuppressive activity in vitro and in vivo. Moreover, they efficiently induce antigen-specific tolerance in vivo. Thus our results demonstrate that nnLNSCs possess a strong, hitherto unrecognized T cell immune-regulating activity by changing the phenotype of DCs and their progenitors into a distinct population of regMΦ.
Methods
Day 3 neonatal mice LN CD45− stromal cell preparation
Day 3 neonatal mice axillary, brachial and mesenteric LNs were isolated, disrupted with a 26G needle (BD Biosciences) and then digested at 37°C for 40 minutes with 0.1 mg/mL Liberase Blendzyme2 (Roche) and 50 U/mL DNaseI (Roche). Digested LN cell suspensions were cultured in RPMI /10% fetal calf serum (FCS)/pen-strep/L-glutamine and expanded for a maximum of 9 passages. Adherent cells were detached from the culture plate by 0.05% trypsin/5mM EDTA (ethylenediaminetetraacetic acid) in phosphate-buffered saline (PBS), and then resuspended in PBS containing 5% FCS and 3mM EDTA. To purify CD45− stromal cells, 3 rounds of cell depletion were performed using anti-CD45 microbeads and autoMACS (Miltenyi Biotec). The purity of CD45− stromal cells was checked with flow cytometry and was always > 99%. All animal experiments were conducted in accordance with local or institutional guidelines and have been approved by the review board of Hannover Medical School and the local government.
Purification and culture of MDPs
BM cells from CX3CR1+/gfp mice were harvested by flushing femurs and tibias. Applying a cocktail of lineage-specific mAbss (CD3, NK1.1, Iab, CD11c, B220, TER-1, and Gr-1), anti–c-kit mAbs (CD117), and anti-CD11b mAbs, CX3CR1+CD11b−lin−c-Kit+ MDPs were sorted by flow cytometry. The purity of sorted population was always > 98%. After cell sorting, MDPs were subsequently cultured in 12-well plates at 1 × 104 cells/well in complete medium (RPMI/10% FCS/pen-strep/L-glutamine) supplemented with 30 ng/mL granulocyte macrophage-colony-stimulating factor (GM-CSF). In some experiments MDPs were cultured without GM-CSF but seeded on monolayers of nnLNSCs. As required, TNFα (30 ng/mL) or lipopolysaccharide (LPS; 1 μg/mL) was added for the final 48 hours of culture.
In vitro T-cell proliferation
Magnetic-activated cell sorting (MACS)–isolated OTII cells (2 × 105) were cocultured with 8000 ovalbumin (OVA)–maDCs or with the same number of OVA-loaded regMΦ (OVA-regMΦ) in 96 U-well plates. In some experiments 2 × 105 OTII cells were cocultured with 8000 OVA-maDCs together with 8000 or 40 000 regMΦ. In some other experiments 2 × 105 MACS-isolated CD45.2+CD4+ T cells (using the CD4+ T cells kit; Miltenyi Biotec) from C57BL/6 mice were stimulated with 2 μL anti-CD3/CD28 dynabeads in the presence or absence of different amounts of CD45.1+CD4+ T cells that were treated with anti-CD3/CD28 dynabeads in the presence of regMΦ.
Immune regulatory effects of regMΦ in vivo
Mice either received intraperitoneally 1 × 107 OTII cells alone or together with either OVA-maDCs (4.5 × 105), OVA-regMΦ (4.5 × 105), or OVA-maDCs (4.5 × 105) together with regMΦ (1.5 × 106). regMΦ were loaded with 0.2 mg/mL OVA for 24 hours at day 5 of coculture on nnLNSCs before being harvested for in vivo intraperitoneal injection. After 5 days, single-cell suspensions of mLNs and spleen were prepared and the number of OTII cells was determined (DAPI−CD45.1+CD4+TCR−Va2+ cells). In other experiments, mice were either left untreated or received intravenously either OVA-maDCs (3 × 105), or OVA-regMΦ (3 × 105; derived from MDPs) or OVA-maDCs (3 × 105) together with regMΦ (1 × 106). At day 7, mice were either immunized subcutaneously with 200 μg OVA or keyhole limpet hymocyanin (KLH) in complete Freund adjuvant (CFA). After another 7 days mice were bled and the amount of serum anti-OVA and anti-KLH antibodies was determined by ELISA. In another experimental modification mice were either left untreated or received intravenously either OVA-maDCs (3 × 105), or OVA-regMΦ (3 × 105; derived from MDPs) or OVA-maDCs (3 × 105) together with regMΦ (1 × 106). At day 7 mice were killed and CD4+ T cells were isolated by MACS. These T cells were intravenously transferred (5 × 106/mouse in a volume of 150 μL PBS) to new recipients that received 1 day later subcutaneously OVA or KLH. At day 15, mice were bled and the amount of anti-OVA and anti-KLH IgG1 and IgG2a was determined.
Statistics
Statistical analysis was performed with GraphPad Prism, 4.0 using unpaired 2-tailed Student t test. Error bars represent SEM or SD as indicated. Statistical differences for the mean values are indicated as *P < .05, **P < .001, and ***P < .0001.
Additional information
The following are provided in supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article): mice, reagents; antibodies used for flow cytometry; immunohistology; generation of BM-derived dendritic cells (BMDCs) and OVA-loaded BMDCs; uptake of Cy5-labeled OVA (OVA-Cy5); cytospins; saining of cells with CFSE (carboxyfluorescein diacetate succinimidyl ester); determination of cytokine production by cytometric bead array; NO detection; and RT-PCR and [3H]thymidine incorporation assay.
Results
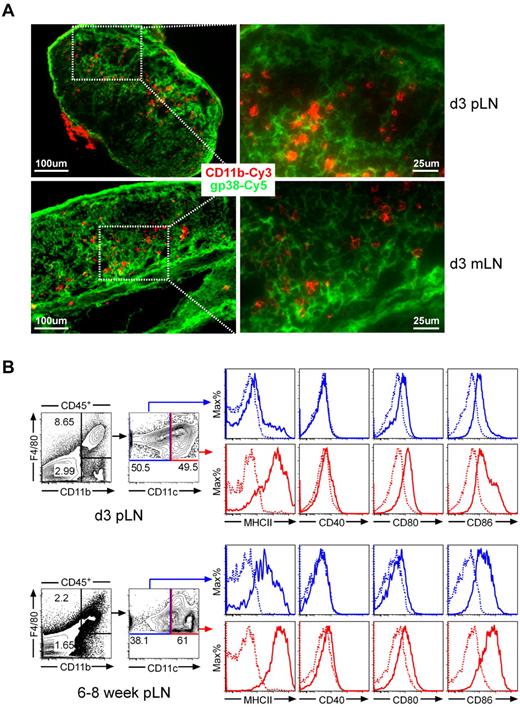
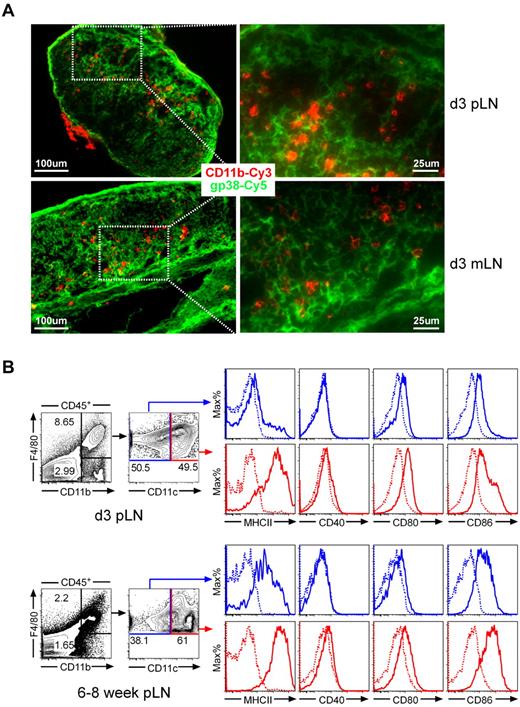
High frequency of F4/80+CD11b+MHCIIlow cells in neonatal LNs
Applying a variety of mAbs in immunohistology of day 3 LNs, we observed that CD11b+ cells to be localized in close proximity to gp38+ stromal cells (Figure 1A), suggesting that nnLNSCs might affect the differentiation of myeloid cells. Further flow cytometric analysis of skin-draining peripheral as well as mesenteric LN revealed a higher frequency of CD11b+ myeloid cells in neonatal (nn) LNs (approximately 9%-12%) compared with adult LNs (approximately 3%-5%). Of note, our analysis also revealed that the percentage of CD45− stromal cells was much higher in neonatal (8%-35%) than in adult (0.6%-1.2%) LNs. Further detailed analysis showed that more than 70% of CD11b+ cells in nnLNs express F4/80+, whereas only approximately 50% of CD11b+ cells in adults expressed this marker. In both adults and neonates this population can be subdivided into CD11chigh and CD11clow cells. Most interestingly, the MHCII expression levels of the CD11b+F4/80+CD11clow population in nn LNs were considerably lower than in adult LNs, whereas mice from both age groups expressed this molecule at comparable levels in the CD11chigh subpopulation. In both adults and neonates the CD11clow subpopulation showed slightly reduced levels CD40, CD80, and CD86 compared with the CD11chigh population. Notably, in nnLNs the CD86 expression of both CD11b+F4/80+ CD11clow and CD11b+F4/80+CD11chigh cells were considerably lower than in adult LNs (Figure 1B). Together these data reveal difference regarding the expression of MHCII and costimulatory molecules of myeloid cell subpopulations in neonates and adults.
CD11b+ myeloid cells localize in close proximity with gp38+ stromal cells in neonatal LNs, which contain abundant CD11b+F4/80+MHCIIlow cells. (A) Expression of CD11b and gp38 in neonatal LNs. Cryosections of day 3-old C57BL/6 mice were stained with antibodies as indicated. Shown are sections representative for 5 animals analyzed. (B) Flow cytometric analysis of CD45+CD11b+ myeloid cells compartment in neonatal peripheral LNs. DAPI−CD45+ cells were grouped into CD11b+F4/80+ (top box) and CD11b+F4/80− (bottom box) subpopulations. The CD11b+F4/80+ subpopulation was further subdivided into CD11clow (blue box) and CD11chigh (red box). Solid lines, mAbs as indicated; dotted lines, isotype. Data are representative of 3 independent experiments.
CD11b+ myeloid cells localize in close proximity with gp38+ stromal cells in neonatal LNs, which contain abundant CD11b+F4/80+MHCIIlow cells. (A) Expression of CD11b and gp38 in neonatal LNs. Cryosections of day 3-old C57BL/6 mice were stained with antibodies as indicated. Shown are sections representative for 5 animals analyzed. (B) Flow cytometric analysis of CD45+CD11b+ myeloid cells compartment in neonatal peripheral LNs. DAPI−CD45+ cells were grouped into CD11b+F4/80+ (top box) and CD11b+F4/80− (bottom box) subpopulations. The CD11b+F4/80+ subpopulation was further subdivided into CD11clow (blue box) and CD11chigh (red box). Solid lines, mAbs as indicated; dotted lines, isotype. Data are representative of 3 independent experiments.
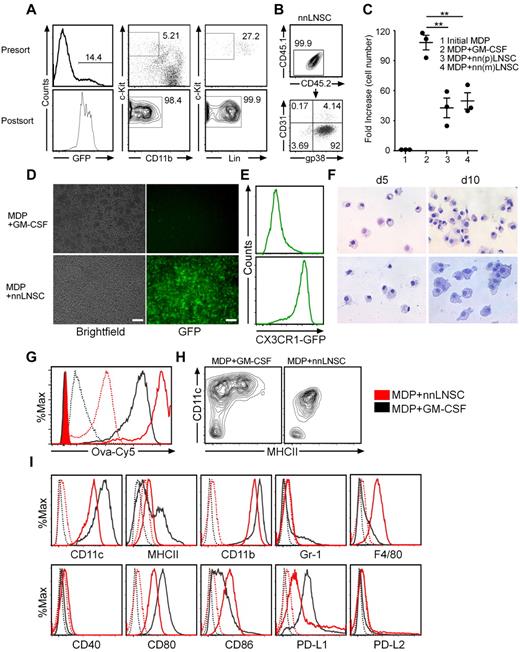
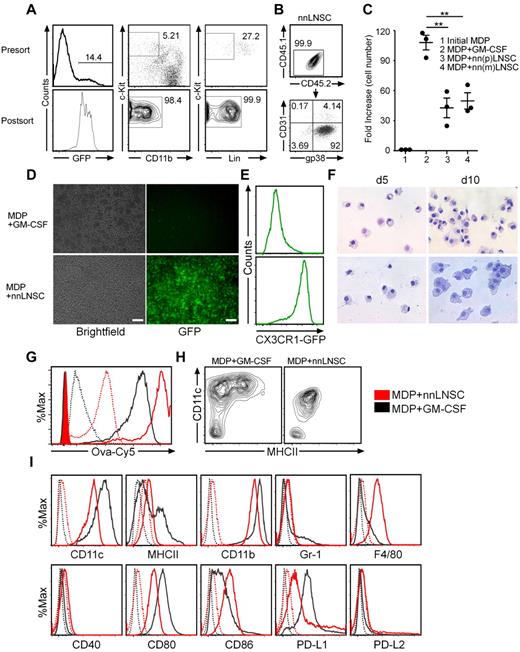
nnLNSCs drive MDPs into a distinct macrophage phenotype
To test the hypothesis that the nnLNSCs might have an effect on the differentiation of myeloid progenitors potentially leading to reduced expression of MHCII and costimulatory molecules on myeloid subpopulations, MDPs from the bone marrow (BM) of CX3CR1+/gfp mice (C57/B6 background), defined as GFP+lin−c-Kit+ cells, were sorted by flow cytometry to 99% purity (Figure 2A). These cells were either cultured in the presence of GM-CSF or seeded on purified nnLNSCs from C57/B6 mice without exogenous cytokines. To this end, CD45− nnLNSCs were isolated from day 3 peripheral or mesenteric LNs and after 3 rounds of MACS-depletion the purity of the CD45.2− stromal cells was > 99%. Further analysis of the phenotype of stromal cells using anti-gp38 (podoplanin) and anti-CD31 mAbs revealed that more than 90% of CD45− stromal cells are gp38+CD31− nnLNSCs (Figure 2B). We could not observe any differences regarding the phenotype and function of nnLNSCs prepared from peripheral and mesenteric LNs. Thus, unless otherwise stated nnLNSCs used in this study were derived from pLNs.
nnLNSCs drive MDPs into a distinct macrophage population. (A) MDPs were isolated from BM cells of CX3CR1+/gfp C57BL/6 mice by FACS. Numbers adjacent to gated areas indicate the percentage of cells before and after sorting. (B) Flow cytometry analysis of nnLNSCs purified by MACS. CD45.2 versus CD45.1 and gp38 versus CD31 expression of nnLNSCs after MACS-purification. (C) MDPs were cultured under the conditions indicated. After 5 days of culture the number of CD45+ cells has been determined. Fold changes are shown (mean ± SEM of 3 wells from 1 representative of 3 independent experiments). (D-I) MDPs cultured with 30 ng/mL GM-CSF only or on a monolayer of nnLNSCs for 10 days. MDPs (104) were seeded/well in 12-well plates and incubated. (D) At day 5, images were captured with bright-field or fluorescent microscope. Scale bar represents 100 μm. (E) At day 5, GFP-expression was monitored by flow cytometry (indicative for CX3CR1 expression), cells were gated on the DAPI−CD45+ population. (F) Cytospin of CD45+ cells sorted by MACS and stained with May-Grünwald-Giemsa after 5 or 10 days of coculture. Images were captured with bright-field microscope, original magnification 40×. (G) At day 5, the phagocytic ability of MDPs cultured with GM-CSF and MDPs educated by nnLNSCs was assessed by flow cytometry after OVA-Cy5 phagocytosis. Black, MDPs cultured with GM-CSF; red, MDPs educated with nnLNSCs (incubation at 37°C, solid line; incubation at 4°C, dotted line; without OVA-Cy5 control, shaded areas). (H-I) Analysis of CD45+ cells after 5 days of culture using antibodies as indicated. Data are representative of at least 3 independent experiments.
nnLNSCs drive MDPs into a distinct macrophage population. (A) MDPs were isolated from BM cells of CX3CR1+/gfp C57BL/6 mice by FACS. Numbers adjacent to gated areas indicate the percentage of cells before and after sorting. (B) Flow cytometry analysis of nnLNSCs purified by MACS. CD45.2 versus CD45.1 and gp38 versus CD31 expression of nnLNSCs after MACS-purification. (C) MDPs were cultured under the conditions indicated. After 5 days of culture the number of CD45+ cells has been determined. Fold changes are shown (mean ± SEM of 3 wells from 1 representative of 3 independent experiments). (D-I) MDPs cultured with 30 ng/mL GM-CSF only or on a monolayer of nnLNSCs for 10 days. MDPs (104) were seeded/well in 12-well plates and incubated. (D) At day 5, images were captured with bright-field or fluorescent microscope. Scale bar represents 100 μm. (E) At day 5, GFP-expression was monitored by flow cytometry (indicative for CX3CR1 expression), cells were gated on the DAPI−CD45+ population. (F) Cytospin of CD45+ cells sorted by MACS and stained with May-Grünwald-Giemsa after 5 or 10 days of coculture. Images were captured with bright-field microscope, original magnification 40×. (G) At day 5, the phagocytic ability of MDPs cultured with GM-CSF and MDPs educated by nnLNSCs was assessed by flow cytometry after OVA-Cy5 phagocytosis. Black, MDPs cultured with GM-CSF; red, MDPs educated with nnLNSCs (incubation at 37°C, solid line; incubation at 4°C, dotted line; without OVA-Cy5 control, shaded areas). (H-I) Analysis of CD45+ cells after 5 days of culture using antibodies as indicated. Data are representative of at least 3 independent experiments.
After 5 days, MDPs cultured in the presence of GM-CSF had expanded 115-fold (± 3), whereas MDPs culture on nnLNSCs expanded 24.95 ± 19.05-fold (pLNs) and 53.00 ± 13.00-fold (mLNs; Figure 2C). MDPs cultured for 5 days in the presence of GM-CSF expressed only a low frequency and small amount of CX3CR1 and showed typical features of DCs. In contrast, MDPs cultured in the presence of nnLNSCs showed a high level expression of CX3CR1 (Figure 2D-E) and a macrophage-like phenotype characterized by a considerable increase in size and the presence of numerous vacuoles. These findings were even more pronounced after 10 days of coculture (Figure 2F). Compared with DCs, the macrophage-like cells ingested more OVA-Cy5 at 37°C and bound more OVA-Cy5 at 4°C to their cell surface (Figure 2G). Furthermore, the macrophage-like cells showed reduced expression of CD11c, MHC class II, and CD80 but high levels of F4/80 compared with the DCs differentiated in the presence of GM-CSF. Some of the macrophage-like cells also had higher expression of PD-L1, but most of them did neither express PD-L2 nor Gr1, a finding that distinguishes these cells from myeloid-derived suppressor cells (MDSCs), which express Gr1 (Figure 2H-I).18 Thus, MDPs differentiated on nnLNSCs proliferate vigorously and develop into a characteristic macrophage-like population (CX3CR1+CD11clowMHCIIlow/−CD40low/−CD80lowCD86lowF4/80+).
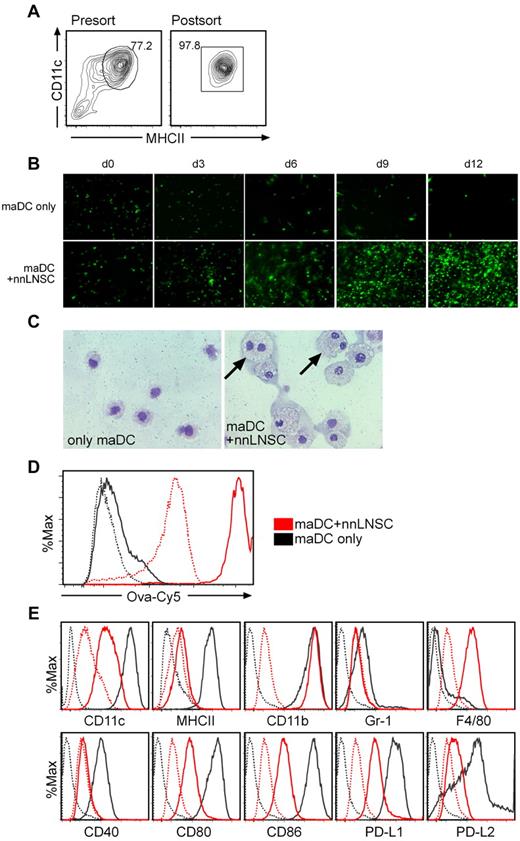
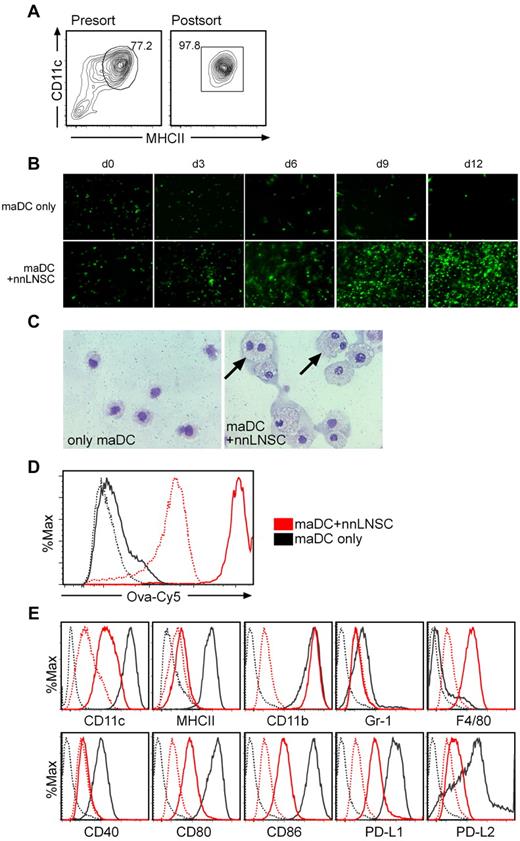
nnLNSCs drive mature dendritic cells into a distinct macrophage phenotype
Because nnLNSCs were able to differentiate MDPs into macrophages, we tested the hypothesis that the stromal cells might have a similar effect on the fate of LPS-matured (ma) DCs (Figure 3A). Seeding these maDCs from EGFP transgenic mice onto CD45− stromal cell monolayers, we found that maDCs attached to the stromal cells and after several days of coculture started to proliferate vigorously (Figure 3B). maDCs cultured on nnLNSCs showed long-term survival and continued to proliferate for more than 2 months (data not shown). To further investigate the morphology of maDCs educated by stromal cells, we sorted the CD45+ cells by MACS 7 days after coculture and analyzed them on May-Grünwald-Giemsa–stained cytospins. These cells showed a typical macrophage morphology with numerous vacuoles and in some cases possessed 2 nuclei (Figure 3C arrows). When testing their phagocytic activity by incubating cells at 4°C or 37°C with Cy5-labeled ovalbumin (OVA-Cy5), we found that the maDCs educated by nnLNSCs regained a strong capacity to take up foreign material compared with the starting maDCs population (Figure 3D). The purity of the FACS-sorted mature CD45.1+CD11chighMHCIIhigh DCs was approx 98%. Flow cytometry of these cells cultured for 10 days in the presence of nnLNSCs revealed reduced expression of CD11c, MHCII, CD40, CD80 and CD86, but up-regulated expression of F4/80 compared with the starting maDCs population. In addition, the cells were negative for Gr-1 (Figure 3E). We also performed the same experiments with immature BMDCs (imDCs) and found similar effects as described here for maDCs (supplemental Figure 1). Furthermore, when imDCs were FACS-sorted into MHCIIhigh and MHCIIlow cells both fractions adapted a rather similar macrophage-like phenotype (supplemental Figure 2). Collectively, these data support the hypothesis that nnLNSCs can drive DCs, independent of their developmental stage into CX3CR1+CD11clowMHCIIlow/−CD40low/−CD80lowCD86lowF4/80+ macrophages. It should be mentioned that we could not observe any difference between nnLNSCs derived from pLNs and mLNs regarding their capacity and potency to program MDPs or reprogram DCs (Figures 2–3, supplemental Figures 1-2). Because the macrophage-like cells derived from coculture with nnLNSCs were highly immunosuppressive in vivo and in vitro (see next paragraphs), we from now on will refer to these cells as regulatory macrophages (regMΦ).
nnLNSCs induce maDCs into a similar macrophage population. (A) maDCs expressing high levels of MHCII and CD11c from either EGFP-C57BL/6 or CD45.1 C57BL/6 mice were sorted by FACS. Representative plots show the expression levels of MHCII and CD11c presort and postsort. (B) nnLNSCs promote maDCs proliferation. Continued proliferation of maDCs after being seeded onto nnLNSCs. EGFP-maDCs cultured alone or on monolayers of nnLNSCs. At the time points indicated images were captured with a fluorescent microscope, original magnification 20×. (C-E) Characteristics of maDCs educated by nnLNSCs. (C) Cytospins of CD45+ cells sorted by MACS from maDCs alone, or maDCs cultured on nnLNSCs for 10 days were stained with May-Grünwald-Giemsa, original magnification 40×. Black arrows indicate proliferating cells with double nuclei. (D) Phagocytic ability of maDCs and maDCs educated by nnLNSCs for 10 days assessed by flow cytometry by uptake of OVA-Cy5. Black lines, maDCs; red lines, maDCs educated by nnLNSCs (solid lines, incubation temperature: 37°C; dotted line, 4°C). (E) CD45.1+ maDCs (black lines) or maDCs educated by nnLNSCs for 10 days (red lines) were stained with antibodies indicated. Dotted lines, corresponding isotype controls. (D-E) Histograms are gated on CD45.1+ cells. Representative data from at least 3 independent experiments are shown.
nnLNSCs induce maDCs into a similar macrophage population. (A) maDCs expressing high levels of MHCII and CD11c from either EGFP-C57BL/6 or CD45.1 C57BL/6 mice were sorted by FACS. Representative plots show the expression levels of MHCII and CD11c presort and postsort. (B) nnLNSCs promote maDCs proliferation. Continued proliferation of maDCs after being seeded onto nnLNSCs. EGFP-maDCs cultured alone or on monolayers of nnLNSCs. At the time points indicated images were captured with a fluorescent microscope, original magnification 20×. (C-E) Characteristics of maDCs educated by nnLNSCs. (C) Cytospins of CD45+ cells sorted by MACS from maDCs alone, or maDCs cultured on nnLNSCs for 10 days were stained with May-Grünwald-Giemsa, original magnification 40×. Black arrows indicate proliferating cells with double nuclei. (D) Phagocytic ability of maDCs and maDCs educated by nnLNSCs for 10 days assessed by flow cytometry by uptake of OVA-Cy5. Black lines, maDCs; red lines, maDCs educated by nnLNSCs (solid lines, incubation temperature: 37°C; dotted line, 4°C). (E) CD45.1+ maDCs (black lines) or maDCs educated by nnLNSCs for 10 days (red lines) were stained with antibodies indicated. Dotted lines, corresponding isotype controls. (D-E) Histograms are gated on CD45.1+ cells. Representative data from at least 3 independent experiments are shown.
regMΦ are T-cell immunosuppressive in vitro
To address whether the regMΦ affect T cell immune responses, we evaluated their antigen-presenting and T-cell immunosuppressive ability in vitro. To this aim, we made use of CD4+ T cells that carry a transgenic TCR specific for an OVA-encoded peptide (OTII cells) as responder cells to regMΦ or maDCs loaded with OVA (OVA-maDCs). After 3 days of coculture, viable OTII cells were collected and analyzed by flow cytometry. OTII cells cultured alone underwent apoptosis to a substantial degree (Figure 4A, data not shown). Although OTII cells stimulated with OVA-maDCs showed a strong proliferative response (Figure 4A-B), OVA-loaded regMΦ (OVA-regMΦ) failed to induce proliferation of the reporter cells (Figure 4A-B). Interestingly, when adding regMΦ to OVA-maDCs/OTII culture we observed a strong suppressive effect of the regMΦ on OTII cell proliferation (Figure 4A-B). As little as 8000 regMΦ were already extremely efficient in suppressing the proliferation of 2 × 105 OTII cells (Figure 4A-B). Next, we tested nnLNs for the presence of natural occurring counterparts of regMΦ. Gating on CD45+CD11b+F4/80+ cells isolated from day 3 nnLNs we found that approximately 60% to 80% of them expressed CX3CR1 (supplemental Figure 3A). To test whether these cells also show T-cell immunosuppressive activity in vitro we sorted CD45+CD11b+F4/80+ cells from day 3 nnLNs to purities > 95% (data now shown). To get sufficient numbers of macrophages these cells were cocultured for 4 days on nnLNSCs before macrophages were resorted and used in T-cell immunosuppression assay. Our results demonstrate that MΦ isolated from nnLNs strongly inhibit T-cell proliferation (supplemental Figure 3B).
MDPs educated by nnLNSCs (regMΦ) are poorly immunogenic but T-cell immunosuppressive in vitro. (A) regMΦ control T-cell proliferation. Cells were incubated as indicated at 37°C for 3 days before the total numbers of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined (mean ± SD of pooled data from 2 independent experiments). (B) Same as panel A; CSFE dilution of OTII cells labeled with the dye prior incubation (circles with numbers indicate conditions depicted in panel A). (C-D) regMΦ do not dampen early activation of OTII cells. Expression of the activation-related markers (C) CD25 and (D) CD69 on OTII cells after 24 hours incubation under experimental conditions shown in panel A were assessed by flow cytometry. Numbers adjacent to gated areas indicate percentage of gated cells. DAPI−CD45.1+CD4+Vα2+ T cells are shown. Data are representative of at least 3 independent experiments. (E-F) The influence of regMΦ on IFNγ and IL-2 levels in the coculture supernatants. After 3 days coculture, IFNγ and IL-2 present in the supernatant were analyzed by cytometric bead array. (G) nnLNSCs are not directly T-cell immunosuppressive. gp38+CD45− and gp38−CD45− nnLNSCs were sorted from peripheral or meseneric LNs by flow cytometry and 8 × 103 stromal cells were seeded per well. One day later, 2 × 105 MACS-isolated CD4+ T cells were added and stimulated with anti-CD3/CD28 dynabeads. After 3 days of culture [3H]-thymidine was added. The incorporation of [3H]-thymidine for 15 hours is shown. (E-G) Values represent mean ± SEM of 3 wells from 1 representative of 2 independent experiments.
MDPs educated by nnLNSCs (regMΦ) are poorly immunogenic but T-cell immunosuppressive in vitro. (A) regMΦ control T-cell proliferation. Cells were incubated as indicated at 37°C for 3 days before the total numbers of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined (mean ± SD of pooled data from 2 independent experiments). (B) Same as panel A; CSFE dilution of OTII cells labeled with the dye prior incubation (circles with numbers indicate conditions depicted in panel A). (C-D) regMΦ do not dampen early activation of OTII cells. Expression of the activation-related markers (C) CD25 and (D) CD69 on OTII cells after 24 hours incubation under experimental conditions shown in panel A were assessed by flow cytometry. Numbers adjacent to gated areas indicate percentage of gated cells. DAPI−CD45.1+CD4+Vα2+ T cells are shown. Data are representative of at least 3 independent experiments. (E-F) The influence of regMΦ on IFNγ and IL-2 levels in the coculture supernatants. After 3 days coculture, IFNγ and IL-2 present in the supernatant were analyzed by cytometric bead array. (G) nnLNSCs are not directly T-cell immunosuppressive. gp38+CD45− and gp38−CD45− nnLNSCs were sorted from peripheral or meseneric LNs by flow cytometry and 8 × 103 stromal cells were seeded per well. One day later, 2 × 105 MACS-isolated CD4+ T cells were added and stimulated with anti-CD3/CD28 dynabeads. After 3 days of culture [3H]-thymidine was added. The incorporation of [3H]-thymidine for 15 hours is shown. (E-G) Values represent mean ± SEM of 3 wells from 1 representative of 2 independent experiments.
Characterization of the T-cell immunosuppressive function mediated by regMΦ
To define the mechanism underlying the T-cell immunosuppression imposed by regMΦ we analyzed the expression of the early activation marker CD25 and CD69 after 24 hours of coculture. Although less than 10% of the OTII cells stimulated by OVA-regMΦ showed weak expression of CD25 and CD69, more than 70% of OTII cells activated with OVA-maDCs showed high expression of both activation markers. Of interest, the addition of regMΦ to OVA-maDCs/OTII coculture did not interfere with cell activation because both markers were also highly expressed on T cells (Figure 4C-D). These findings indicate that although regMΦ are T-cell immunosuppressive, they do not interfere with the early steps of T-cell activation.
Because secretion of IFNγ as well as IL-2 are characteristic features of activated T cells, we tested whether the presence of regMΦ can interfere with the production of these cytokines. As described above, OTII cells were activated with OVA-maDCs in the absence or presence of regMΦ or with OVA-regMΦ alone. As expected, OVA-maDCs triggered expression of IFNγ and IL-2, whereas regMΦ failed to induce the production of significant amount of both cytokines (Figure 4E-F). After stimulation with OVA-maDCs in the presence of regMΦ less IFNγ was detected compared with stimulation with OVA-maDCs alone (Figure 4E). In contrast, we failed to observe a similar effect regarding IL-2 secretion (Figure 4F). Of interest, the presence of regMΦ did not affect the percentage of IFNγ+ OTII cells in OTII/OVA-maDCs coculture (supplemental Figure 4). Because the proliferation of OTII cells is dramatically inhibited by the presence of regMΦ, IFNγ levels in the supernatants were significantly down-regulated (Figure 4E). These data indicate that impaired T-cell proliferation was obviously not caused by lack of IL-2. It has been recently described that fibroblastic reticular cells (FRCs) isolated from adult mouse LNs can dampen the proliferation of activated T cells via NOS2.19-21 However, neither CD45−gp38+ nor CD45−gp38− nnLNSCs showed any T-cell immunosuppressive activity in the assays used here (Figure 4G).
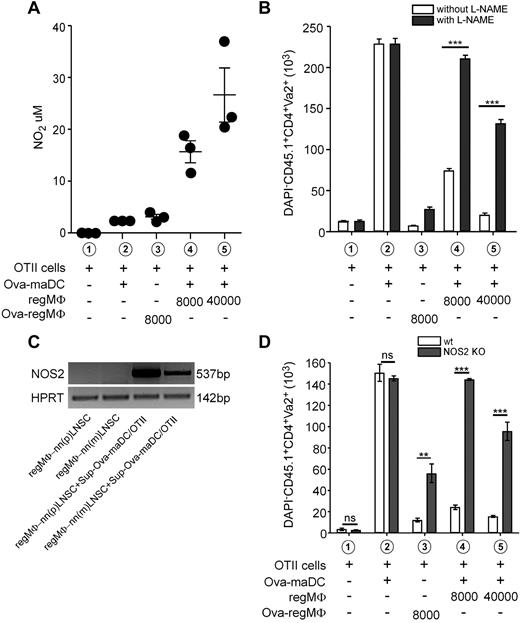
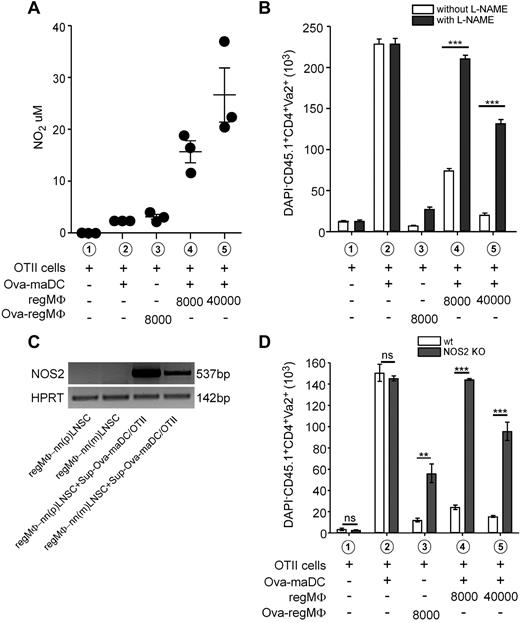
T-cell immunosuppression of regMΦ is mediated by nitric oxide and inducible nitric oxide synthase
Nitric oxide (NO) is known to act as a potent T-cell suppressant.22 We thus tested the hypothesis that NO is involved in mediating the immunosuppressive activity of regMΦ. As shown in Figure 5A, neither OTII cells alone nor OTII cells stimulated by OVA-maDCs produced significant amounts of NO. In contrast, the addition of regMΦ dose dependently induced high amounts of NO. Furthermore, NO was also detectable in coculture supernatants of CD4+ T cells stimulated by anti-CD3/CD28 dynabeads in the presence of regMΦ that were either generated from MDPs or immature DCs (supplemental Figure 5). To confirm a potential role of NO in regMΦ-mediated immunosuppression, we tested the effects of Nω nitro-L-arginine methyl ester (L-NAME), a inhibitor of nitric oxide synthases (NOS), in our system. Although the addition of 1mM L-NAME could completely overcome the suppressive effect of 8000 regMΦ present in the system, this concentration of the inhibitor also resulted in an approximately 66% recovery of the suppressive effect exerted by 40 000 regMΦ (Figure 5B). Of the 3 NOS known,22 we tested whether inducible NOS (NOS2) is present in resting or activated regMΦ. Although regMΦ grown in cell culture medium did not express NOS2, the addition of supernatants (50%, vol/vol) from OVA-maDCs/OTII cocultures induced within 48 hours a strong expression of NOS2 in regMΦ (Figure 5C). The supernatant added contained high amount of proinflammatory cytokines such as IFNγ and TNFα (data not shown), suggesting that the suppressive effect of regMΦ on T cells is mediated by NOS2, which in turn is induced by cytokines produced by activated T cells. To directly address the immunosuppressive activity of NOS2 derived from regMΦ we generated regMΦ by coculturing nnLNSCs for 7 days with immature BMDCs derived from wild-type (WT) or NOS2−/− mice. Flow cytometric analysis did not reveal any differences between WT and NOS2-deficient cells (data not shown). However, when using DCs-derived regMΦ in in vitro T-cell immunosuppression assay by coculturing these cells together with OTII cells and OVA-maDCs, we observed that, compared with WT regMΦ NOS2−/− regMΦ were considerably less efficient in suppressing T-cell proliferation (Figure 5D).
NO-mediated T-cell immunosuppression by regMΦ. (A) Dose-dependent effect of regMΦ on NO production. OTII cells were stimulated for 48 hours at the conditions indicated. Before the concentration of NO in the medium was determined (mean ± SEM of 3 wells from a representative of 2 independent experiments). (B) Addition of L-NAME restored T-cell proliferation. The total number of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined after 3 days of coculture conditions indicated (open bars, without; closed bars, with 1mM L-NAME; mean ± SEM of 3 wells from a representative of 2 independent experiments). (C) Supernatant from OTII cells that were activated by OVA-maDCs can induce NOS2 specific transcripts in regMΦ. Supernatants were harvested from OTII cells activated for 3 days by OVA-maDCs. One-half of culture medium of 105 regMΦ (MDPs cultured on nnLNSCs for 5 days was exchanged by the supernatant of OVA-maDCs activated OTII cells. After further 48 hours, total RNA was prepared and mRNA specific for NOS2 and HPRT mRNA determined by RT-PCR. Data are representative of at least 3 independent experiments. (D) regMΦ generated from NOS2−/− immature DCs were inefficient in suppressing T-cell proliferation. BM cells from WT BL6 mice and NOS2−/− mice (BL6 background) were cultured with GM-CSF to generated BMDCs. On day 7, immature DCs were harvested and put into coculture with nnLNSCs. After another 7 days, WT (open bars) or NOS2-deficient (closed bars) regMΦ were used in in vitro T-cell immunosuppression assay. The total number of DAPI−CD45.1+CD4+ Va2+OTII cells was determined after 3 days of cocultures at the conditions indicated (mean ± SEM of 3 wells from 1 representative of 2 independent experiments).
NO-mediated T-cell immunosuppression by regMΦ. (A) Dose-dependent effect of regMΦ on NO production. OTII cells were stimulated for 48 hours at the conditions indicated. Before the concentration of NO in the medium was determined (mean ± SEM of 3 wells from a representative of 2 independent experiments). (B) Addition of L-NAME restored T-cell proliferation. The total number of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined after 3 days of coculture conditions indicated (open bars, without; closed bars, with 1mM L-NAME; mean ± SEM of 3 wells from a representative of 2 independent experiments). (C) Supernatant from OTII cells that were activated by OVA-maDCs can induce NOS2 specific transcripts in regMΦ. Supernatants were harvested from OTII cells activated for 3 days by OVA-maDCs. One-half of culture medium of 105 regMΦ (MDPs cultured on nnLNSCs for 5 days was exchanged by the supernatant of OVA-maDCs activated OTII cells. After further 48 hours, total RNA was prepared and mRNA specific for NOS2 and HPRT mRNA determined by RT-PCR. Data are representative of at least 3 independent experiments. (D) regMΦ generated from NOS2−/− immature DCs were inefficient in suppressing T-cell proliferation. BM cells from WT BL6 mice and NOS2−/− mice (BL6 background) were cultured with GM-CSF to generated BMDCs. On day 7, immature DCs were harvested and put into coculture with nnLNSCs. After another 7 days, WT (open bars) or NOS2-deficient (closed bars) regMΦ were used in in vitro T-cell immunosuppression assay. The total number of DAPI−CD45.1+CD4+ Va2+OTII cells was determined after 3 days of cocultures at the conditions indicated (mean ± SEM of 3 wells from 1 representative of 2 independent experiments).
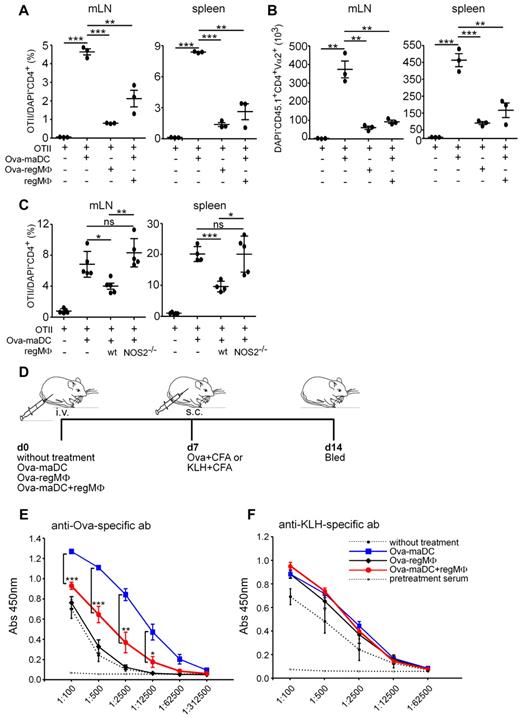
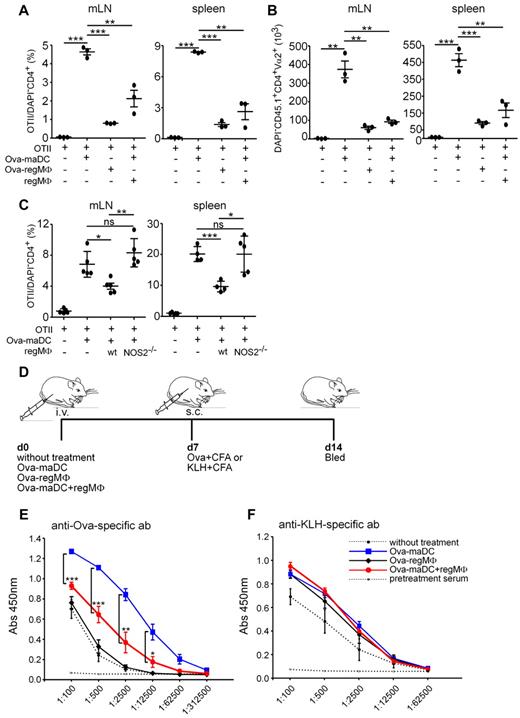
regMΦ show T-cell immunosuppression in vivo
Given the strong T-cell immunosuppression achieved by regMΦ in vitro we next asked whether they can also perform T-cell immunosuppression in vivo. We therefore adoptively transferred OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ i.p. into naive C57BL/6 mice that also received OTII cells. Five days after transfer, mice were killed and the number of OTII cells was determined in mLNs and spleen. Whereas OVA-regMΦ induced T-cell proliferation moderately, OVA-maDCs were highly efficient in inducing T-cell proliferation. Interestingly, the coapplication of regMΦ together with OVA-maDCs could almost completely prevent the OVA-maDC–mediated expansion of OTII cells (Figure 6A-B). To test whether NO derived from regMΦ plays a role in this process we applied WT and NOS2−/− regMΦ derived from immature DCs (Figure 5D) and found that NOS2−/− regMΦ failed to suppress T-cell proliferation in vivo (Figure 6C). Together, these data show that regMΦ are highly efficient in reducing T-cell proliferation in vivo and indicate that NOS2 plays a critical role in regMΦ-mediated T-cell immunosuppression in vivo.
regMΦ show T-cell immunosuppression and induce antigen-specific immune tolerance in vivo. (A-B) regMΦ are T-cell immunosuppressive in vivo. OTII cells (1 × 107) were intraperitoneally transferred into recipients together without or with OVA-maDCs, OVA-regMΦ or OVA-maDCs together with regMΦ. After 5 days the percentage (A) of DAPI−CD45.1+CD4+Vα2+ viable OTII in DAPI−CD4+ cells and the absolute number (B) of DAPI−CD45.1+CD4+Vα2+ viable OTII cells in mLNs and spleen were determined (dots represent individual mice analyzed in 1 experiment; similar results were obtained in a second experiment). (C) NOS2 deficient regMΦ are incapable in T-cell immunosuppression in vivo. OTII cells (1 × 107) were intraperitoneally transferred into recipients together with or without OVA-maDCs, together with WT or NOS2−/− regMΦ. After 5 days the percentage of DAPI−CD45.1+CD4+Vα2+ OTII in DAPI−CD4+ cells was determined (dots represent individual mice analyzed in 2 independent experiments). (D-F) regMΦ induce antigen-specific immune tolerance in vivo. OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ were injected intravenously in to syngeneic C57BL/6 mice. Seven days later, mice were immunized subcutaneously with OVA or KLH in CFA. Serum IgG1 levels against OVA (E) or KLH (F) were measured by ELISA. Serum was diluted serially as indicated (mean ± SEM, 3 mice per group). Similar data were obtained in a second experiment.
regMΦ show T-cell immunosuppression and induce antigen-specific immune tolerance in vivo. (A-B) regMΦ are T-cell immunosuppressive in vivo. OTII cells (1 × 107) were intraperitoneally transferred into recipients together without or with OVA-maDCs, OVA-regMΦ or OVA-maDCs together with regMΦ. After 5 days the percentage (A) of DAPI−CD45.1+CD4+Vα2+ viable OTII in DAPI−CD4+ cells and the absolute number (B) of DAPI−CD45.1+CD4+Vα2+ viable OTII cells in mLNs and spleen were determined (dots represent individual mice analyzed in 1 experiment; similar results were obtained in a second experiment). (C) NOS2 deficient regMΦ are incapable in T-cell immunosuppression in vivo. OTII cells (1 × 107) were intraperitoneally transferred into recipients together with or without OVA-maDCs, together with WT or NOS2−/− regMΦ. After 5 days the percentage of DAPI−CD45.1+CD4+Vα2+ OTII in DAPI−CD4+ cells was determined (dots represent individual mice analyzed in 2 independent experiments). (D-F) regMΦ induce antigen-specific immune tolerance in vivo. OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ were injected intravenously in to syngeneic C57BL/6 mice. Seven days later, mice were immunized subcutaneously with OVA or KLH in CFA. Serum IgG1 levels against OVA (E) or KLH (F) were measured by ELISA. Serum was diluted serially as indicated (mean ± SEM, 3 mice per group). Similar data were obtained in a second experiment.
Next, we investigated whether regMΦ can suppress an antigen-specific, T cell dependent humoral immune response in vivo using an immunization regime depicted in Figure 6D. Mice received intravenously either OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ, or left untreated. At day 7 one-half of the mice from each group were immunized subcutaneously with OVA or with KLH. After another 7 days serum IgG1 and IgG2a levels against OVA or KLH were measured by ELISA (Figure 6E, data not shown). Interestingly, mice that received OVA-maDCs together with regMΦ showed significantly lower serum IgG1 and IgG2a levels against OVA than mice that received OVA-maDCs only. Compared with mice that were initially either left untreated or received OVA-regMΦ, the coapplication of regMΦ together with OVA-maDCs led to an approximately 90% reduction in specific anti-OVA IgG1 (Figure 6D). In contrast, the coapplication of regMΦ had no significant effect on the production of anti-KLH antibodies (Figure 6F), suggesting that regMΦ are able to suppress T-cell responses in an antigen-specific manner.
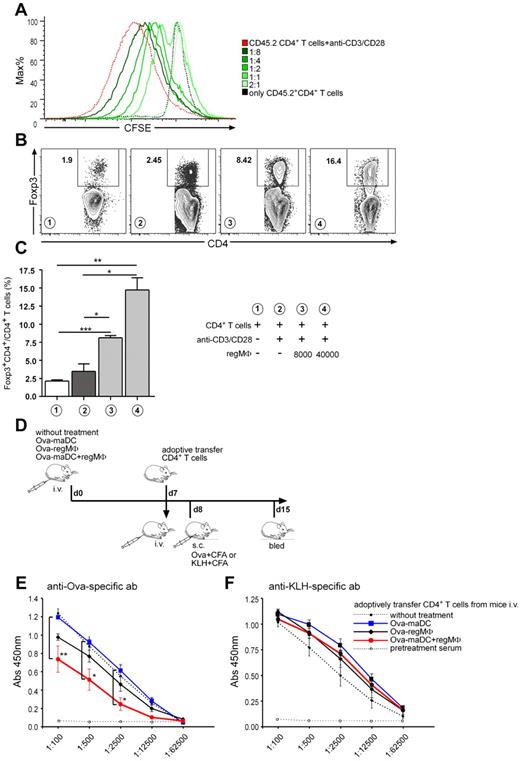
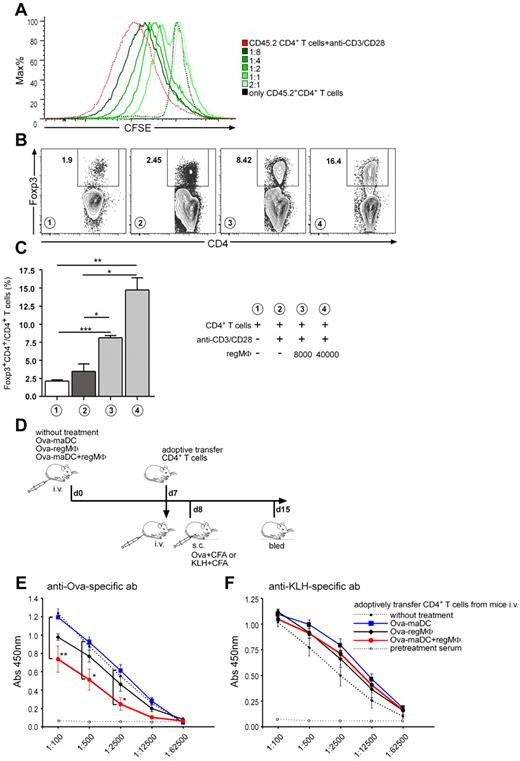
regMΦ can exert immune tolerance by expanding Tregs in vitro
To test the hypothesis whether the presence of regMΦ influence the ensuing response of T cells through Tregs induction or expansion, we stimulated CD4+ T cells isolated from CD45.1 mice with anti-CD3/CD28 dynabeads in the presence or absence of regMΦ. After 5 days of coculture CD4+ cells were MACS-sorted and mixed with increasing amounts of CFSE-labeled CD45.2+CD4+ T cells that were stimulated by anti-CD3/CD28 dynabeads. As depicted in Figure 7A, CD45.1+CD4+ T cells expanded in the presence of regMΦ showed a dose-dependent suppression of T-cell proliferation. Of note, at a ratio of 2:1 (CD45.1+CD4+T educated by regMΦ:CD45.2+CFSE+CD4+) proliferation of the reporter T cells was entirely blocked, and even at ratios of 1:8 some suppression was still detectable. The percentage of Foxp3+CD4+ cells after anti-CD3/CD28 dynabead stimulation in the presence or absence of regMΦ was further analyzed. Although only 3.48 ± 1% Foxp3+ cells were found in the anti-CD3/CD28-only cultures, the presence of regMΦ dose-dependently increased this fraction up to 14.8 ± 1.7% (Figure 7B-C). Moreover, this increase was strongly reversed by anti-TGFβ antibody treatment (supplemental Figure 6). By further applying eGFP−CD4+ T cells sorted from Foxp3eGFP reporter mice23 as responders to anti-CD3/CD28 dynabead stimulation, we found that the presence of regMΦ can only support the expansion of existing Tregs rather than Treg induction from naive T cells in vitro based on the observation that we could not observe induction of eGFP+ Tregs from eGFP−CD4+ T cells (data not shown).
CD4+ T cells proliferating in presence of regMΦ are T-cell immunosuppressive in vitro and in vivo. (A) CD4+ T cells proliferating in the presence of regMΦ gain T-cell immunosuppressive capacity. CD45.1+CD4+ T cells (2 × 105) were stimulated with anti-CD3/CD28 dynabeads in the presence of 4 × 104 regMΦ. Five days later, CD4+ T cells were again sorted by MACS to obtain CD45.1+CD4+ T cells. Together with anti-CD3/CD28 dynabeads these cells were cocultured with MACS-purified, CFSE-labeled, CD45.2+CD4+ T cells at the ratios indicated. Five days later, proliferation of CD45.2+CD4+ T cells was analyzed by flow cytometry. Cells were gated on the DAPI−CD45.2+CD4+ population. Data are representative of at least 3 independent experiments. (B) Expression of Foxp3 by CD4+ T cells cultivated in the presence of regMΦ. CD4+ T cells (2 × 105 C57BL/6) were stimulated with anti-CD3/CD28 dynabeads in the presence of 8000 or 4 × 104 regMΦ as indicated. Five days later, cells were stained intracellularly with anti-Foxp3 mAb. Gates were set on CD4+ cells. Numbers adjacent to gated areas indicate the percentage of Foxp3+CD4+ Treg. Number in circles indicate experimental conditions described in panel C. (C) Statistical analysis of (B; mean ± SEM, n = 3). Similar results were obtained in another 2 experiments. (D-E) CD4+ T cells from mice immunized with OVA-maDCs in the presence regMΦ transmit antigen-specific immune suppression in vivo. (D) Experimental setup of in vivo immune tolerance induction. At day 0 syngeneic C57BL/6 mice intravenously received, OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ. At day 7, CD4+ T cells were isolated from LNs and spleen of different groups and 5 × 106 cells/mouse were adoptively transferred into another cohort of naive C57BL/6 recipients. At day 8 these mice were immunized with OVA or KLH in CFA, and at day 15 mice were bled. Serum IgG1 levels against OVA (E) or KLH (F) were measured by ELISA. Serum was diluted serially as indicated (values represent mean ± SEM; 3 mice per group were analyzed). Similar data were obtained in a second experiment.
CD4+ T cells proliferating in presence of regMΦ are T-cell immunosuppressive in vitro and in vivo. (A) CD4+ T cells proliferating in the presence of regMΦ gain T-cell immunosuppressive capacity. CD45.1+CD4+ T cells (2 × 105) were stimulated with anti-CD3/CD28 dynabeads in the presence of 4 × 104 regMΦ. Five days later, CD4+ T cells were again sorted by MACS to obtain CD45.1+CD4+ T cells. Together with anti-CD3/CD28 dynabeads these cells were cocultured with MACS-purified, CFSE-labeled, CD45.2+CD4+ T cells at the ratios indicated. Five days later, proliferation of CD45.2+CD4+ T cells was analyzed by flow cytometry. Cells were gated on the DAPI−CD45.2+CD4+ population. Data are representative of at least 3 independent experiments. (B) Expression of Foxp3 by CD4+ T cells cultivated in the presence of regMΦ. CD4+ T cells (2 × 105 C57BL/6) were stimulated with anti-CD3/CD28 dynabeads in the presence of 8000 or 4 × 104 regMΦ as indicated. Five days later, cells were stained intracellularly with anti-Foxp3 mAb. Gates were set on CD4+ cells. Numbers adjacent to gated areas indicate the percentage of Foxp3+CD4+ Treg. Number in circles indicate experimental conditions described in panel C. (C) Statistical analysis of (B; mean ± SEM, n = 3). Similar results were obtained in another 2 experiments. (D-E) CD4+ T cells from mice immunized with OVA-maDCs in the presence regMΦ transmit antigen-specific immune suppression in vivo. (D) Experimental setup of in vivo immune tolerance induction. At day 0 syngeneic C57BL/6 mice intravenously received, OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ. At day 7, CD4+ T cells were isolated from LNs and spleen of different groups and 5 × 106 cells/mouse were adoptively transferred into another cohort of naive C57BL/6 recipients. At day 8 these mice were immunized with OVA or KLH in CFA, and at day 15 mice were bled. Serum IgG1 levels against OVA (E) or KLH (F) were measured by ELISA. Serum was diluted serially as indicated (values represent mean ± SEM; 3 mice per group were analyzed). Similar data were obtained in a second experiment.
To test the hypothesis that the observed reduction of the T-cell dependent B-cell response observed in Figure 6D might be mediated at least in part by Treg, we adopted the protocol accordingly (Figure 7D). As described for Figure 6C, mice were either left untreated, or received either mature OVA-maDCs, OVA-regMΦ, or OVA-maDCs together with regMΦ. After 7 days these animals were killed, CD4+ T cells from LNs and spleen were isolated by MACS and intravenously transferred into B6 recipients. The next day one-half of the mice of each group of the recipients was immunized with OVA, whereas the other one-half was immunized with KLH. Another 7 days later, mice were bled (Figure 7D) and serum IgG1 and IgG2a levels against OVA or KLH were measured by ELISA. Mice that received CD4+ T cells isolated from donors treated with OVA-maDCs together with regMΦ showed specifically decreased serum IgG1 and IgG2a level against OVA compared with those that received CD4+ cells from OVA-maDCs-treated donors (Figure 7E, data not shown). As described for Figure 6E, we failed to observe any effect on the formation of anti-KLH–specific antibodies (Figure 7F). Although the underlying mechanisms that allow antigen-specific immune-suppression are unclear, we suppose that expansion of Tregs and/or the induction of T-cell anergy by regMΦ participates in this process. This assumption is based on our in vivo results showing strongly reduced antigen-specific T-cell proliferation after regMΦ are present (Figure 6A-B). However, we cannot rule out that regMΦ might also have an direct effect on B cells.
Discussion
In this study, we tested the hypothesis that LN stromal cells contribute to immune tolerance in mice indirectly by manipulating cells of the macrophage/DCs lineage. Compared with adults, we found a significantly higher frequency of CD11b+F4/80+ CD11clowMHCIIlow myeloid cells in neonatal peripheral and mesenteric LNs, and abundant gp38+ stromal cells localizing in close proximity to CD11b+ myeloid cells. Based on this observations we tested whether gp38+ stromal cells have an effect on the fate of myeloid cells. Interestingly, 60% to 80% of the macrophages isolated from pLNs or mLNs of day 3 neonatal CX3CR1+/gfp mice expressed CX3CR1 (supplemental Figure 3A) and performed a strong T-cell immunosuppression (supplemental Figure 3B). Using in vitro coculture systems, we found that CX3CR1+lin−c-kit+ MDPs from CX3CR1−/gfp mice in coculture with nnLNSCs gave rise the characteristic CX3CR1+CD11b+MHCIIlow/−CD11clowF4/80+Gr1− macrophage population. Such cells were large in size, showed numerous vacuoles and phenotypically displayed decreased expression of CD11c, faint or no expression of MHCII, persistently high expression of CD11b and CX3CR1. They showed intermediate expression of F4/80, but lacked detectable expression of Gr1. Importantly, MDPs cultured with nnLNSCs not only vividly proliferated and showed a macrophage morphology but also regained the ability to efficiently take up foreign material.
Of interest, nnLNSCs also had a profound effect on the reprogramming of both immature and LPS-matured BM-derived DCs, as well as BM derived macrophages (supplemental Figure 7). In coculture with nnLNSCs all these cells remarkably switched their phenotype and (re-) gained novel functions as described above for regMΦ derived from MDPs with strongly reduced expression of MHCII and costimulatory molecules. From these observations we conclude that even at different starting points of differentiation, nnLNSCs drive the differentiation of DCs and their progenitors toward a distinct population of CX3CR1+CD11b+MHCIIlow/−CD11clowF4/80+Gr1− regMΦ.
The regMΦ described in this study are different from regulatory DCs obtained from coculture of mature BMDCs with day 7 spleen stromal cells24 and regulatory DCs derived from the coculture of day 7 spleen stromal cells with hematopoietic stem cells.25 The regulatory DCs derived from mature BM-DCs lack expression of F4/80 and CX3CR1 and show higher expression of CD80 and CD40 than the regMΦ described here.24 Moreover, the regulatory DCs reported by Tang et al express CD40 at a stable and much higher level than regMΦ.25 Along the same line, Svensson et al reported the generation of CD11clowCD45RBhi regulatory DCs using coculture of lin−c-kit+ progenitors with adult spleen stromal cells.26 In contrast to CD11clow CD45RBhi regulatory DCs, regMΦ do not express CD45RB (data not shown). Furthermore, neither LPS nor TNFα treatment of regMΦ results in the up-regulation of CD11c, MHCII, CD86, or CD40 (data not shown), effects that have been described for the CD11clowCD45RBhi regulatory DCs.26 It also should be mentioned that the cells described as regulatory DCs kept their DCs morphology very much in contrast to the regMΦ reported here. regMΦ are also different from MDSCs, which are primarily found in tumors and known to express Gr1.18
Mesenchymal stem cells (MSCs) were also shown to affect DC differentiation and function.27-32 Of interest, it has been reported that human mesenchymal stem cells as well as fibroblast or epithelial cell lines push the differentiation of monocytes or hematopoietic stem cells toward macrophages. These cells also showed decreased expression of CD11c, MHCII, as well as costimulatory molecules and gained a macrophage-like morphology,33,34 suggesting that nnLNSCs influence the fate of DCs through similar mechanisms. However, by applying anti–IL-6 antibody we did not find any significant influence of this cytokine on the phenotype of regMΦ (data now shown), which is in contrast to the above reports.33,34 We found that nnLNSCs can secret several cytokines spontaneously including IL-6, VEGF, M-CSF, or G-CSF (data not shown). GM-CSF is also detectable in the supernatant of nnLNSCs (data not shown). Because the phenotype of regMΦ is rather distinct from BM derived DCs and macrophages, we suppose that neither GM-CSF nor M-CSF secreted by nnLNSCs alone is sufficient for the generation and expansion of regMΦ. By applying a transwell coculture system, we investigated whether soluble factors secreted by nnLNSCs or/and cell-cell contact are necessary or sufficient for the induction of regMΦ. Compared with the direct coculture MDPs did not proliferate as efficiently when they were separated from nnLNSCs by transwell filters. Furthermore, these macrophages lost the T-cell immunosuppressive ability although the phenotype of both populations was strikingly similar (data not shown). These findings indicate cell-cell contact between nnLNSCs and MDPs is indispensable for the differentiation of MDPs into fully functional regMΦ.
Armed with different mechanisms, such as NO and arginase I-production,24,25,35 induction of Treg36 or IL-10–producing T regulatory type 1 (Tr1) cells,26 the capacity to inhibit T-cell proliferation is the hallmark of all the regulatory DCs reported. Therefore, we investigated the impact of nnLNSCs-induced regMΦ on T-cell proliferation. In line with their low or negative expression of MHCII and low expression of costimulatory molecules, these cells cannot serve as efficient antigen-presenting cells per se. However, they showed a strikingly strong T-cell immune suppression as third-party cells by inhibiting the proliferation of Ag-specific CD4+ T cells on culture with antigen-loaded maDCs. In doing so, they did not dampen early activation of T cells or their IFNγ and IL-2 secretion. Interestingly, the T-cell immunosuppression of regMΦ was mediated to a large part by NO because most of the in vitro effects of regMΦ on T-cell proliferation could be blocked by L-NAME which is a functional NOS inhibitor. Moreover, NOS2-expression can be induced by proinflammatory cytokines released from activated T cells. Both in vitro and in vivo, NOS2-deficient regMΦ, generated from immature DCs, are incapable to suppress T-cell proliferation. It should be noted that WT regMΦ generated from immature DCs were less efficient in suppressing T-cell proliferation than those derived from MDPs (compare Figure 6A with 6C) indicating that “reprogrammed” regMΦ might be less immunosuppressive than those directly derived from MDPs. It is currently also not clear yet how and to what degree regMΦ-mediated T-cell immunosuppression is antigen-specific. On one hand these cells could inhibit anti-CD3/CD28-induced CD4+ T-cell proliferation showing that T-cell immunosuppression of regMΦ can be mediated in the absence of antigen. On the other hand however, regMΦ showed antigen-specific immunosuppression on T-cell dependent B-cell responses (Figures 6E-F, and 7E-F). Thus further studies are needed to reveal the role of specific antigen in regMΦ-mediated T-cell immunosuppression.
In contrast to regulatory DCs generated by day 7 spleen stromal cells,24,25 regMΦ increased the percentage of Foxp3+CD4+ T cells in in vitro cultures. The CD4+ T cells proliferating in the presence of regMΦ possessed profound inhibitory effects in vitro. TGFβ and IL-10 are the 2 critical factors for generating Foxp3+ regulatory T cells37-40 and T regulatory type 1 (Tr1) cells,41,42 respectively. In support of the expansion of Treg, we found that regMΦ can produce TGFβ and anti-TGFβ antibody treatment reduced the percentage of Treg cells after CD4+ T-cell activation (supplemental Figure 6). However, our preliminary results suggest that the presence of regMΦ does not favor the de novo induction of Tregs from naive T cells in vivo and that regMΦ were still fully functional in mice with depleted Tregs (data not shown). Together these observations indicate that release of NO rather than induction/expansion of Tregs reflects the major mode of action of these cells in vivo. Along the same line, we could differentiate regMΦ from MDPs from the BM of IL-10−/− mice that were phenotypically indistinguishable from those from WT mice and also showed full T-cell immunosuppressive function (data now shown). A recent report from our laboratory showed that CX3CR1 signaling is also necessary to expand Foxp3+ Treg in the intestine.43 However, in our in vitro system IL-10 deficiency does not affect the frequency of Foxp3+CD4+ Treg.
Although nnLNSCs were highly efficient in differentiating DCs and MDPs toward regMΦ this property could also be observed after we used LNSCs from 6- to 8-week-old mice (supplemental Figure 8). In contrast to the in situ situation in the neonatal LNs stromal cells of adult LNs were not in cell cycle in situ as revealed by BrdU-incorporation assays (data not shown). However, these adult LNSCs started to proliferate once cultured in Petri dishes, suggesting that they also might potentially regain functional properties of proliferating stromal cells that are present in situ in neonatal LNs. This hypothesis is also supported by our finding that we found in the neonatal but not in the adult LNs cells showing the phenotype of regMΦ (Figure 1B, data not shown).
Together, our findings contribute to a better understanding of how regMΦ are generated and widen the knowledge of the “spectrum” of macrophage populations44 present in higher vertebrates. This may help to provide new insights on the induction of antigen-specific immune tolerance helping to create novel cell-based therapeutic approaches for the treatment of allergic and autoimmune diseases.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Christina Reimer and Matthias Ballmaier for cell sorting, Ulrike Schleicher and Christian Bogdan, University of Erlangen-Nuremberg, for generously providing bone marrow from Nos2−/− mice, and Günter Bernhardt for valuable suggestions and critically reading this paper.
This work was supported by Deutsche Forschungsgemeinschafts grant SFB738-B5 to R.F.
Authorship
Contribution: X.Y.Z. designed and performed research, analyzed data, and wrote the paper; S.F.Y., K.H., and K.Y. performed experiments; and R.F. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Reinhold Förster, Institute of Immunology, Hannover Medical School, Carl-Neuberg Strasse 1, D-30625, Hannover, Germany; e-mail: foerster.reinhold@mh-hannover.de.

![Figure 4. MDPs educated by nnLNSCs (regMΦ) are poorly immunogenic but T-cell immunosuppressive in vitro. (A) regMΦ control T-cell proliferation. Cells were incubated as indicated at 37°C for 3 days before the total numbers of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined (mean ± SD of pooled data from 2 independent experiments). (B) Same as panel A; CSFE dilution of OTII cells labeled with the dye prior incubation (circles with numbers indicate conditions depicted in panel A). (C-D) regMΦ do not dampen early activation of OTII cells. Expression of the activation-related markers (C) CD25 and (D) CD69 on OTII cells after 24 hours incubation under experimental conditions shown in panel A were assessed by flow cytometry. Numbers adjacent to gated areas indicate percentage of gated cells. DAPI−CD45.1+CD4+Vα2+ T cells are shown. Data are representative of at least 3 independent experiments. (E-F) The influence of regMΦ on IFNγ and IL-2 levels in the coculture supernatants. After 3 days coculture, IFNγ and IL-2 present in the supernatant were analyzed by cytometric bead array. (G) nnLNSCs are not directly T-cell immunosuppressive. gp38+CD45− and gp38−CD45− nnLNSCs were sorted from peripheral or meseneric LNs by flow cytometry and 8 × 103 stromal cells were seeded per well. One day later, 2 × 105 MACS-isolated CD4+ T cells were added and stimulated with anti-CD3/CD28 dynabeads. After 3 days of culture [3H]-thymidine was added. The incorporation of [3H]-thymidine for 15 hours is shown. (E-G) Values represent mean ± SEM of 3 wells from 1 representative of 2 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/17/10.1182_blood-2011-06-359315/4/m_zh89991289770004.jpeg?Expires=1766076219&Signature=n7CEla8d2FdvogrD1H5dhmQ6mRZWT59z1K~YT1MHNPOPQGcJVteAXcFHCF2FRNXicgRkHOo4ibvbLYvvi9tScH9fcXfnZmpnstIwOmTJjWIsN0FsQet3f~IClF2I5NsdTIBuFK3gDw55S14nVxSOqXg5szEbRvBYMYbDCJu2v0xZ7ryAQnWg0wiJCJD6z91gFjGFUzyuCEdf6vcJ-XNlBvtvqOZogLkhZZ4Z5zRkN1dUR8uT-QjMFXPPqqcFEN~OScfDb8xfO9t0vtj3m~VW~gnvs-F7dy~2c-TnKavQdOym~~kugaFQSKn9C1jOF4SZ~oIoDmWghQ6jZYqPj7nCuA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 4. MDPs educated by nnLNSCs (regMΦ) are poorly immunogenic but T-cell immunosuppressive in vitro. (A) regMΦ control T-cell proliferation. Cells were incubated as indicated at 37°C for 3 days before the total numbers of DAPI−CD45.1+CD4+Vα2+ OTII cells was determined (mean ± SD of pooled data from 2 independent experiments). (B) Same as panel A; CSFE dilution of OTII cells labeled with the dye prior incubation (circles with numbers indicate conditions depicted in panel A). (C-D) regMΦ do not dampen early activation of OTII cells. Expression of the activation-related markers (C) CD25 and (D) CD69 on OTII cells after 24 hours incubation under experimental conditions shown in panel A were assessed by flow cytometry. Numbers adjacent to gated areas indicate percentage of gated cells. DAPI−CD45.1+CD4+Vα2+ T cells are shown. Data are representative of at least 3 independent experiments. (E-F) The influence of regMΦ on IFNγ and IL-2 levels in the coculture supernatants. After 3 days coculture, IFNγ and IL-2 present in the supernatant were analyzed by cytometric bead array. (G) nnLNSCs are not directly T-cell immunosuppressive. gp38+CD45− and gp38−CD45− nnLNSCs were sorted from peripheral or meseneric LNs by flow cytometry and 8 × 103 stromal cells were seeded per well. One day later, 2 × 105 MACS-isolated CD4+ T cells were added and stimulated with anti-CD3/CD28 dynabeads. After 3 days of culture [3H]-thymidine was added. The incorporation of [3H]-thymidine for 15 hours is shown. (E-G) Values represent mean ± SEM of 3 wells from 1 representative of 2 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/119/17/10.1182_blood-2011-06-359315/4/m_zh89991289770004.jpeg?Expires=1766076220&Signature=yNyOIHJgBuoxVGgdfQjY2y7crJGh8AsQZaSXL-Hh8o3eR7uP0GIBazRj43OAlgT5gXLxiQIH1SgMTOS3g0tcAsulXjycsD2Zoj077EEJKGCxO8h5TiLbZAs7lPqpcWMXUpxv9MbLISFaF9NHEAY31XJalKbnb5vN~ttjUaZzcWp7BBq8YbNk7B5JYCpaufwVrpWBQOMOUmr80iUgnB7bsliCdQkohlBICxUYzFGzAA5OMaS-NLVhKfzftHo0Ekguk-C9cqcNdeOjIaCdlPGNsK8JiBgREttoakonSfo8uTEP~3Jp9GwZ3dzFZRnStnXPpnuOSjXSVKBIAw9MntRAQQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)