Abstract
We have developed and previously reported on a therapeutic vaccination strategy for indolent B-cell lymphoma that combines local radiation to enhance tumor immunogenicity with the injection into the tumor of a TLR9 agonist. As a result, antitumor CD8+ T cells are induced, and systemic tumor regression was documented. Because the vaccination occurs in situ, there is no need to manufacture a vaccine product. We have now explored this strategy in a second disease: mycosis fungoides (MF). We treated 15 patients. Clinical responses were assessed at the distant, untreated sites as a measure of systemic antitumor activity. Five clinically meaningful responses were observed. The procedure was well tolerated and adverse effects consisted mostly of mild and transient injection site or flu-like symptoms. The immunized sites showed a significant reduction of CD25+, Foxp3+ T cells that could be either MF cells or tissue regulatory T cells and a similar reduction in S100+, CD1a+ dendritic cells. There was a trend toward greater reduction of CD25+ T cells and skin dendritic cells in clinical responders versus nonresponders. Our in situ vaccination strategy is feasible also in MF and the clinical responses that occurred in a subset of patients warrant further study with modifications to augment these therapeutic effects. This study is registered at www.clinicaltrials.gov as NCT00226993.
Introduction
Cutaneous T-cell lymphoma (CTCL) is a group of mature T-cell lymphomas with primary presentation in the skin.1 Mycosis fungoides (MF) is the most common subtype, with pleomorphic skin lesions including patches, plaques, tumor lesions, and erythroderma. The skin-tropic malignant cells are CD3+/CD4+/CLA+/CCR4+ with loss of CD7 and CD26.2,3 It is considered a malignancy of skin-homing or skin-resident CD4+ T cells; however, the specific molecular mechanisms of induction and progression are yet to be ascertained. As an indolent lymphoma with a chronic course, immunotherapeutic modality can play a significant role in long-term disease control in MF without exposing the patients to undesirable toxicities of traditional cytotoxic chemotherapies.
Primary immune-stimulatory or modulatory therapies currently used in MF or Sézary syndrome (SS) include interferons, retinoids, and extracorporeal photopheresis.4 Newer immunotherapeutic approaches under investigation in CTCL include monoclonal antibodies,5,6 transimmunization,7 and customized vaccines.8,9 Few different approaches to dendritic cell (DC)–based vaccination regimens have been studied in CTCL. Although encouraging clinical responses and immune effects were noted in each, all required significant ex vivo manipulation to generate a patient-specific vaccine product.8,9 In a phase I study, intratumoral injections of live attenuated measles virus induced clinical responses in CTCL and increased anti-measles antibody titer after therapy.10
Toll-like receptor (TLR) agonists represent a novel approach to stimulate an antitumor immune response by activating and bridging the innate and adaptive immunity.11 In a phase I study, a TLR9-activating CpG oligodeoxynucleotide (ODN) was administered subcutaneously at uninvolved skin sites in patients with MF or SS.12 Antitumor activity was noted, including some complete responses. The most common adverse events were injection-site reactions and flu-like symptoms that were anticipated and mostly mild.
In a murine B-cell lymphoma model, the combination of intratumoral injection of CpG ODN with systemic cytotoxic therapy effectively provided tumor antigens from dying tumor cells to antigen-presenting cells (APCs) and activated these APCs to present their engulfed antigens to T cells.13 This combination approach was required to induce tumor-reactive CD8+ T cells and to cure mice of an established and systemic lymphoma. We found similar results when CpG was combined with local radiation therapy (RT) in the same murine model. After this proof of concept in the murine model, a clinical trial was performed in patient with systemic B-cell lymphoma, primarily follicular and marginal zone lymphomas.14 Localized low-dose RT was administered together with intratumoral injection of CpG ODN to serve as an in situ vaccination maneuver. This procedure was well tolerated, and systemic clinical responses were observed in 4 of 15 patients (27%), including one who had a complete response. Given that MF tumor cells are also very radiosensitive, we elected to test a similar in situ vaccination strategy to determine whether it could induce the regression of distant, nonirradiated sites of skin lesions in patients with MF.
Methods
Study design and eligibility criteria
This was a single institution phase 1/2 study evaluating the safety, feasibility, and efficacy of in situ vaccination using intratumoral CpG injections combined with local low-dose RT. It was approved by the Institutional Review Board and the Scientific Review Committee at Stanford Cancer Center. Written informed consent was obtained from each patient before study enrollment, in accordance with the Declaration of Helsinki.
Adult patients (age, ≥ 18 years) with biopsy-confirmed MF of stage IA-IVA who failed at least 1 standard therapy were eligible. Patients with SS were excluded. Patients were required to have skin lesions appropriate for intratumoral injection of CpG and measurable disease in areas other than the injection site. An adequate washout from prior MF treatments was required, including 2 weeks from topical therapy; 4 weeks from phototherapy and radiation therapy; and 4 weeks from systemic therapies, including cytotoxic chemotherapy. A Karnofsky performance status of ≥ 70, adequate bone marrow, hepatic function, and renal function were required for participation. Patients were excluded if they had pre-existing autoimmune disease or a known history of serious or active infection.
Treatment schema
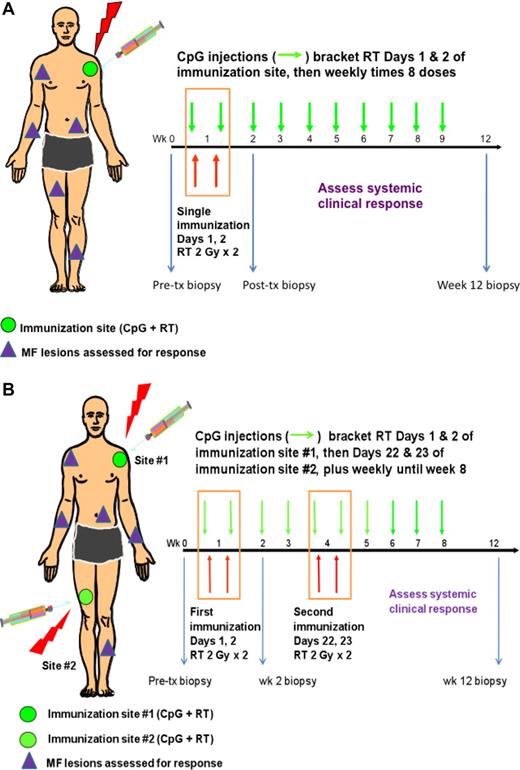
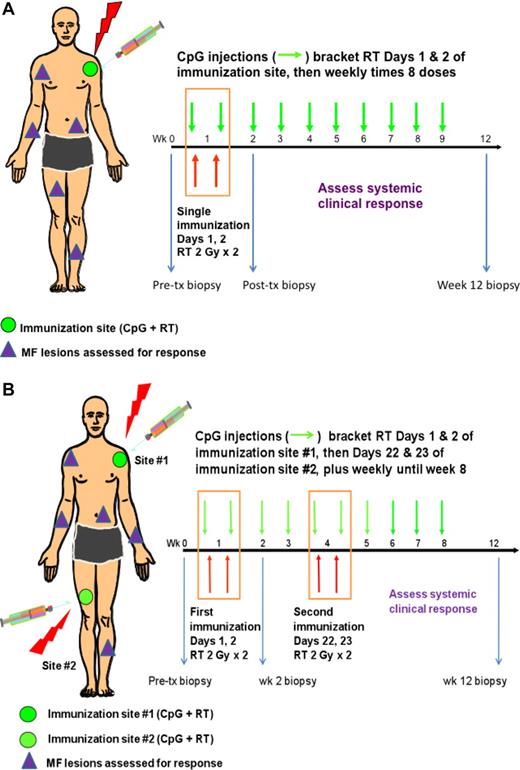
For the immunization procedure, a measurable MF skin lesion with adequate size and optimal thickness was selected (immunization site in Figure 1A-B). Systemic antitumor clinical response was assessed by measuring MF skin lesions that were not subjected to the immunization procedure. Each immunization consisted of irradiating a single MF skin lesion on days 1 and 2 (2 Gy each day) along with intratumoral injection of CpG-enriched TLR9 agonist (also referred to as CpG) PF-351267612 (Pfizer Inc) 6 mg within an hour before the day 1 and after the day 2 RT. This was followed by 8 weekly intratumoral injections of the same CpG compound. The planned duration of study was 12 weeks, after which time the primary evaluation of safety, efficacy, and immune response was performed. Clinical response was assessed weekly up to week 8 and then at week 12. After week 12, patients were followed monthly for 3 months and then every 2 months until disease progression or patient withdrawal. The first 6 patients were treated with a single immunization procedure (Figure 1A). After that we added an additional immunization for patients 7 to 15 (Figure 1B). For the second immunization procedure, a remote MF skin lesion was selected that was preferably linked to different lymph node (LN) drainage basin. The combined CpG and RT was then repeated at this second site at week 4 (Figure 1B).
Treatment schema. The single immunization procedure (A) consisted of irradiating a single MF skin lesion on days 1 and 2 (2 Gy each day) along with intratumoral injection of CpG within an hour before the day 1 and after the day 2 RT. CpG was then injected into the same site weekly for an additional 8 doses for a total of 10 doses. From patient 7 (B), a boost immunization was delivered at a distant MF lesion at week 4, and weekly CpG injections were performed at that site until completion of 10 doses. Systemic clinical response was assessed by mSWAT of nonimmunized MF lesions weekly until week 8 and then at week 12. Correlative skin samples were obtained from the immunization site at baseline and week 2.
Treatment schema. The single immunization procedure (A) consisted of irradiating a single MF skin lesion on days 1 and 2 (2 Gy each day) along with intratumoral injection of CpG within an hour before the day 1 and after the day 2 RT. CpG was then injected into the same site weekly for an additional 8 doses for a total of 10 doses. From patient 7 (B), a boost immunization was delivered at a distant MF lesion at week 4, and weekly CpG injections were performed at that site until completion of 10 doses. Systemic clinical response was assessed by mSWAT of nonimmunized MF lesions weekly until week 8 and then at week 12. Correlative skin samples were obtained from the immunization site at baseline and week 2.
Safety and efficacy assessments
Treatment toxicity was evaluated weekly for the first 9 weeks; at week 12; monthly for 3 months; and then every 2 months until end of study. Adverse events (AEs) were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events Version 3.0.
The primary efficacy end point was the evaluation of skin disease response as measured by modified severity-weighted assessment tool (mSWAT).15 Medical photography was obtained at each clinical assessment visit to support the mSWAT response data. A complete response (CR) was defined as complete resolution of all disease. A partial response (PR) was defined by a greater than or equal to 50% reduction in the mSWAT score compared with baseline. CR/PR required confirmation after 4 weeks. Progressive disease (PD) was defined as a greater than or equal to 25% increase in the mSWAT score from baseline. Patients who did not meet the criteria for CR, PR, or PD were considered to have stable disease (SD).
Immunohistochemistry
Sections (4 μm in thickness) of formalin-fixed, paraffin-embedded biopsies were placed on glass slides, baked for 1 hour at 60°C, deparaffinized in xylene, and hydrated in a series of graded alcohols. Commercially available antibodies were used to assess the expression of following markers using standard dilutions and antigen retrieval and chromogen development methods: CD3 (polyclonal; R&D Systems), CD4 (IF6; Novocastra), CD5 (4C7; Novocastra), CD8 (C8/144B; Dako North America), CD20 (L26; Dako North America), CD25 (4C9; Novocastra), CD30 (Ber-H2; Dako North America), CD56 (123C3; Zymed Laboratories), CD123 (BD Biosciences Pharmingen), CD163 (10D6; Novocastra), C4d (polyclonal; Cell Marque), TIA-1 (2G9; Immunotech), CD1a (010; Dako North America), S100 (polyclonal; Dako North America), FoxP3 (236A/E7; eBioscience), and active caspase-3 (polyclonal; R&D Systems).
A semiquantitative scoring system was developed and assessed by D.G. (hematopathologist) and F.R.A. (dermatopathologist). The definition of histologic grade of the H&E review was as follows: epidermal infiltrate 1 to 3 based on amount of epidermotropic tumor cells, dermal infiltrate density scored 1 to 3, with 1 being few cells to 3 defined as confluent infiltrate. Large cell transformation (LCT) was defined as > 25% if tumor cells were large cell by morphology.16 Immunohistochemistry (IHC) was graded on a scale of 1 to 4, with the following definitions: 1, < 5% immunoreactive; 2, 5% to 24%; 3, 25% to 74%; and 4, ≥ 75%. CD4, CD5, CD8, CD25, CD30, CD56, TIA-1, and FoxP3 expression was scored as percentage positive of the CD3+ population, whereas activated caspase-3, C4d, CD1a, CD3, CD20, CD123, CD163, and S100 were scored as percentage positive of the dermal mononuclear infiltrate. Quantitative scoring (enumeration) of CD3+ lymphocytes within the epidermis and CD1a+, CD25+, CD123+, FoxP3+, and S100+ cells within the superficial dermis was performed under oil immersion at ×1000 by D.G.; the 2 densest areas were identified at scanning power, and the average density of 2 high-power fields (hpf) is reported.
Immunofluorescence
Frozen sections (4 μm in thickness) were mounted on poly-l-lysine–coated slides. The tissue was fixed in precooled acetone at −20°C for 10 minutes; air-dried; washed in PBS, pH 7.4; immunostained; and then coverslipped with VECTASHIELD mounting medium containing 4′,6-diamidino-2-phenylindole nuclear counterstain (Vector Laboratories). Direct immunofluorescence was performed by incubating with (1) FITC–conjugated polyclonal rabbit anti–human C3c antibody (Dako North America), (2) FITC-conjugated F(ab′)2 polyclonal rabbit anti–human IgG antibody (Dako North America), or (3) FITC-conjugated F(ab′)2 polyclonal rabbit anti–human IgM antibody (Dako North America) at 1:20 for 45 minutes at room temperature in the dark. Bullous pemphigoid tissue was used as a positive control. Indirect immunofluorescence was performed by incubating with matched patient serum at 1:80 in antibody diluent (Dako North America) at room temperature for 45 minutes, rinsed, and then incubated with FITC-conjugated F(ab′)2 polyclonal rabbit anti-human IgG (Dako North America) at 1:20 for 45 minutes at room temperature in the dark. Pemphigus vulgaris serum was used as a positive control. Slides were stored at 4°C, and images were captured with Eclipse E200 fluorescent microscope with a PLAN APO 40×/0.95 objective lens and DXM1200C digital camera with ACT-1C Version l.02 software (Nikon).
Serum antibody binding assay
Serum antibody binding was performed on CD4+ T cells isolated from MF skin biopsy, blood taken from patients more than 6 months after any CpG treatment, or both. Fresh tissue was placed in 1× EDTA-free Protease Inhibitor Cocktail (Roche Diagnostics), prepared in complete media (RPMI-1640 + 10% FCS) per the manufacturer's directions. Cells were teased out via mechanical manipulation aided by a 30- to 45-minute incubation with collagenase (Liberase Thermolysin Medium Research Grade; Roche Diagnostics) at a final concentration of 15 μg/mL at 37°C. The enzyme activity was quenched with a 10-fold volume of cold complete media, and the cells were counted and stained for CD4, CD8, and CD3 expression using directly conjugated antibodies (BD Biosciences).
Serum binding was assessed by incubating the cells at 4°C with serum drawn before, after, and during CpG treatment at a final dilution of 1:3. Antibody binding was detected using a goat anti–human IgG phycoerythrin (PE; Southern Biotechnology Associates). Cells were run on an FACSCalibur (BD Biosciences) and analyzed using an online-based software provided by Cytobank Inc 2010 (http://www.cytobank.org).
Assessment of TLR9 sensitivity
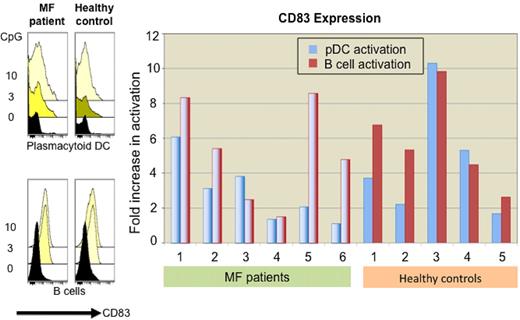
Leukocytes were isolated from heparinized peripheral blood from patients or healthy controls by Ficoll gradient and were then cultured in complete media at 37°C, 5% CO2 for 18 hours with 0, 3, or 10 μg/mL CpG ODN PF-3512676. Afterward, cells were washed and stained with the following antibody panel (BD Biosciences): CD3, CD14, CD16, CD56 (lin)–FITC, CD83-PE, CD123-PE-Cy7, HLA-DR-allophycocyanin, and CD19-AMCyan. Sensitivity was analyzed by an LSR-II flow cytometer (BD Biosciences). Overlaid histograms illustrate CD83 expression on either plasmacytoid dendritic cells (pDCs) by gating on lin−, CD123+ live cells or on B cells by gating on lin−, CD19+ live cells. Statistics presented are median fluorescence intensity within that gate.
Statistical analysis
All enrolled patients were included in the assessment of the primary end point of this study. Duration of response (DOR) was determined from date of initial response to PD. Several patients withdrew from study follow-up to initiate localized MF skin therapy without meeting PD; these patients were censored at time of termination of follow-up. Time to response (TTR), DOR, and time to progression were analyzed by Kaplan-Meier method.
The significance of differences in baseline versus postimmunization parameters of local tissue for paired values were assessed by Wilcoxon signed rank test, and comparisons between responders versus nonresponders were done using nonparametric Wilcoxon methods. Statistical analyses were conducted using SAS Version 9.2 (SAS Institute).
Results
Patient characteristics
In total, 15 patients were enrolled in the study (Table 1). The median age of the entire study cohort was 57 years (range, 18-71 years); 12 of 15 patients were male. Five patients had clinical stage IB and 10 had IIB disease. Three of 10 patients with stage IIB had LCT and 2 had folliculotropic MF (FMF), each a known unfavorable prognostic feature. None of the IB patients had LCT, although 1 had FMF. The median number of all prior therapies (skin-directed and systemic) was 5 (range, 2-9) and that of prior systemic therapies was 1 (range, 0-6).
In situ vaccination therapy is feasible and safe
Overall, our in situ vaccination using intratumoral CpG combined with RT was very well tolerated, with AEs mostly of only grade 1 or 2 (Table 2). The most common treatment-related AE was injection site reaction (15 of 15) consisting of local erythema, pain, and induration/swelling. All patients reported at least 1 adverse event of flu-like symptoms (eg, fever, chills, headache, fatigue, myalgia, arthralgia). Two patients developed regional lymphadenopathy postimmunization therapy. All of these AEs were reversible and manageable. The only patient with grade 3 AE was patient 13, who experienced severe injection site reaction with focal skin necrosis. The patient was withdrawn from the study as specified by the protocol, and the reaction resolved in 3 to 4 weeks without any further complications. No clinical signs of autoimmune disorder were observed during or after therapy.
Systemic antitumor clinical responses are observed
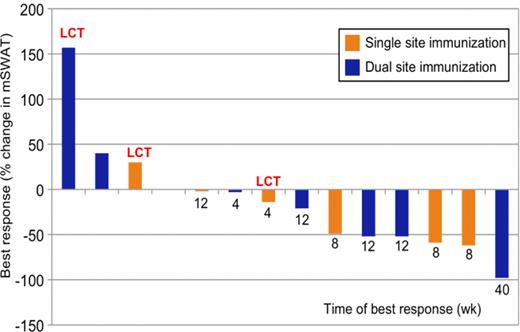
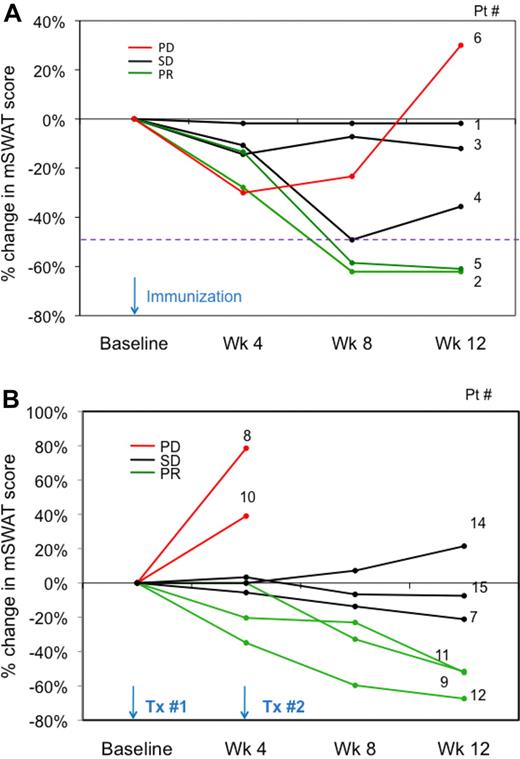
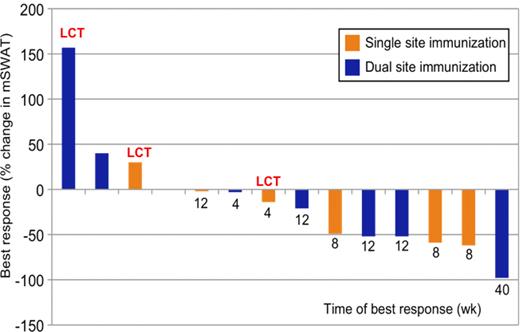
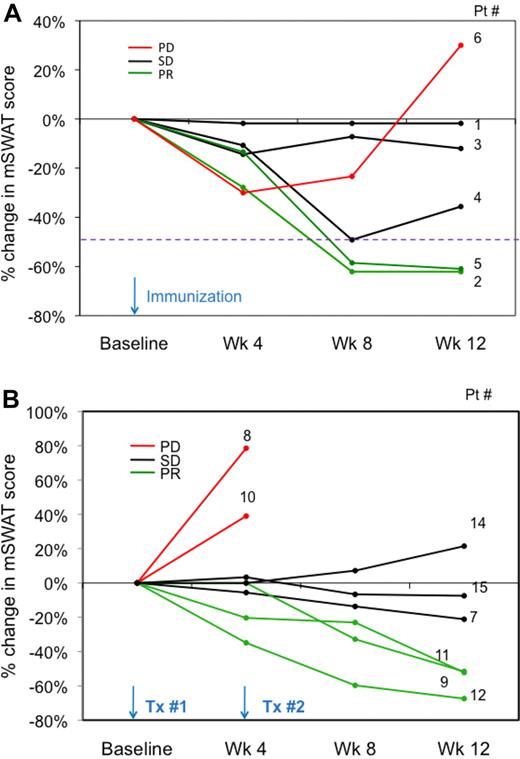
Two of 6 patients who received single immunization procedure achieved a clinically meaningful response, with PR as the best response (Figure 2). An additional patient (4) had a near PR. As the mSWAT scores reached a plateau at week 4 to 5 in the nonresponding patients (Figure 3A), a second (boost) immunization procedure was then introduced at week 4 to enhance the immune response (Figure 1B). Three patients who received the boost immunization demonstrated an objective response, with PR being the best response (Figure 3B). Representative photographs of responding patients with the single and dual immunization are provided in Figure 4A and B. Of the 15 patients enrolled, only 14 were included in the efficacy analysis; patient 13, who was forced to terminate prematurely for grade 3 injection site AE, was excluded. The overall response rate of evaluable cohort (n = 14) was 35.7% (33.3%, single immunization; 37.5%, dual immunization). The median TTR was 7.9 weeks (range, 7.1-12.0 weeks), and the median DOR was 7.0 weeks (range, 6.0-37.0 weeks). Six patients had documented PD; of these patients, 3 experienced PD at or before week 12 and had either LCT or FMF. Two patients failed to receive their second immunization because they documented PD before their scheduled boost immunization. The median time to progression for the study cohort was 20.3 weeks (range, 2.4-44.1 weeks).
Waterfall plot showing percent change in skin mSWAT score at time of best clinical response. All values are shown as the percentage of change in the mSWAT score compared with the baseline assessment calculated at screening.
Waterfall plot showing percent change in skin mSWAT score at time of best clinical response. All values are shown as the percentage of change in the mSWAT score compared with the baseline assessment calculated at screening.
Percentage of change in mSWAT score from baseline (skin tumor burden). (A) Single immunization schedule, patients 1 to 6. (B) Dual immunization schedule, patients 7 to 15.
Percentage of change in mSWAT score from baseline (skin tumor burden). (A) Single immunization schedule, patients 1 to 6. (B) Dual immunization schedule, patients 7 to 15.
Systemic antitumor clinical response observed with single or dual immunization schedule. (A) Patient 2 (64-year-old man, stage IIB) was treated with the single immunization procedure. Systemic evaluation site was the left calf, and the immunization site was the left thigh. PR was noted at week 8, with DOR of 12 weeks. Patient met progression criteria per mSWAT score at week 20 and withdrew from the trial to start topical steroid therapy. (B) Patient 9 (71-year-old man, stage IB) received dual immunization treatment. Systemic evaluation sites were the lower legs, and lesions on each thigh served as the immunization sites. PR was noted at week 12, with DOR of 6 weeks. Patient withdrew from trial at week 18 to initiate topical nitrogen mustard to small areas of recurrent skin disease.
Systemic antitumor clinical response observed with single or dual immunization schedule. (A) Patient 2 (64-year-old man, stage IIB) was treated with the single immunization procedure. Systemic evaluation site was the left calf, and the immunization site was the left thigh. PR was noted at week 8, with DOR of 12 weeks. Patient met progression criteria per mSWAT score at week 20 and withdrew from the trial to start topical steroid therapy. (B) Patient 9 (71-year-old man, stage IB) received dual immunization treatment. Systemic evaluation sites were the lower legs, and lesions on each thigh served as the immunization sites. PR was noted at week 12, with DOR of 6 weeks. Patient withdrew from trial at week 18 to initiate topical nitrogen mustard to small areas of recurrent skin disease.
We assessed for clinical parameters predictive of systemic antitumor response. LCT histology may be a negative predictor of response (P = .08) because none achieved objective clinical response. Of the 3 patients with FMF, the stage IB patient responded, but the 2 stage IIB patients did not respond. There were no statistically significant differences in age, gender, clinical stage, baseline tumor burden (measured mSWAT), number or type of prior therapies, or adverse event profile (including regional lymphadenopathy) between the clinical responders versus nonresponders.
MF skin tissue infiltrate is rich in CD25+, FoxP3+ T cells and APCs preimmunization
The majority of cases showed moderate to marked epidermotropism, with a prominent dermal infiltrate. CD3+ and CD4+ T cells composed the majority of the infiltrate; 2 markers associated with regulatory T cells (Tregs), CD25 and FoxP3, were expressed in more than 25% of the epidermal and dermal CD3+ T-cell infiltrate in most cases. By contrast, CD8+ T cells comprised less than 25% of the CD3+ dermal infiltrate in most cases and CD20+ B-cells were generally infrequent (< 5%). The percentage of T cells expressing the cytotoxic marker TIA-1 varied widely, but no significant CD56+ component was present in any sample. APCs expressing S100 or CD1a were richly represented in the skin infiltrate, more than 5% in most cases (median, 31.5/hpf and 25.0/hpf, respectively); CD123+ pDCs were less frequent, estimated at less than 5% in most cases (median, 3.0/hpf).
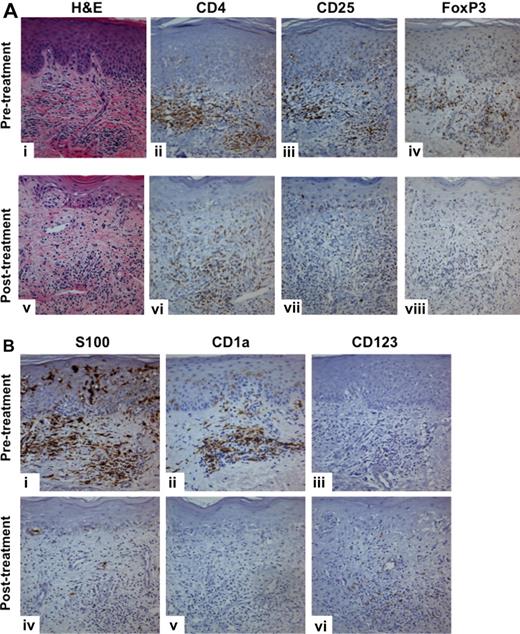
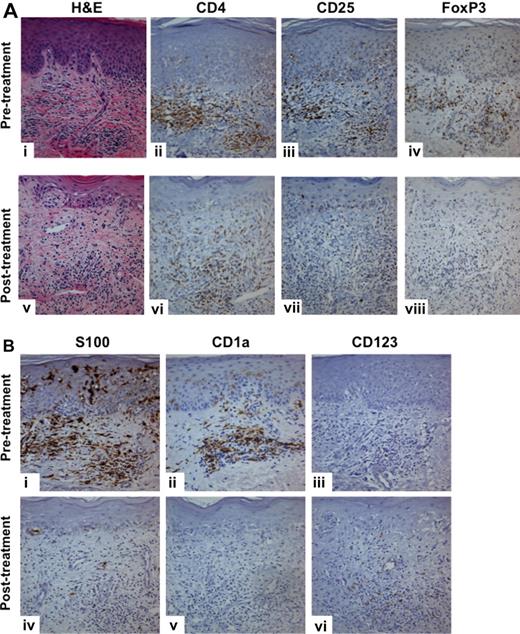
Significant decreases in CD25+, FoxP3+ T cells and APCs occurred, whereas CD123+ pDCs increased at the immunized site
We examined pre- and posttreatment paired biopsies of the immunized site available from 11 patients. Treg markers CD25 and FoxP3 both showed a more than 50% median decrease (Figure 5A), a decrease that was significant by both qualitative (P = .0078 for both) and quantitative (P = .0049 and P = .0020, respectively) measures. APC markers S100 and CD1a likewise decreased significantly, by a median of 84% for S100 (P = .031, grading; P = .01, enumeration) and 96% for CD1a (P = .016, grading; P = .001, enumeration; Figure 5B). By contrast, we noted an increase in CD123+ probable pDCs, by a median of 115%. Because of the lower overall numbers of CD123+ cells, this difference was not captured by the 4-point grading system but was significant by enumeration (P = .003). No statistically significant differences were present in any of the other histologic or IHC parameters studied.
Significant decreases in CD25+, FoxP3+ T cells and APCs, whereas CD123+ pDCs show increases at the immunized site. (A) A significant decrease in the CD25, FoxP3–expressing T-cell infiltrate was noted when comparing skin biopsies taken from the immunization site before and after treatment (week 2). (B) S100+ and CD1a+ DC numbers also decreased at these time points, whereas CD123+ pDC numbers increased. Images were acquired using a model BX51 microscope with a 100×/1.25 NA Plan oil objective lens and Microfire digital camera with PictureFrame Version 2.3 software (Olympus). Digitized images were processed using Photoshop 7 image processing and manipulation software (Adobe Systems).
Significant decreases in CD25+, FoxP3+ T cells and APCs, whereas CD123+ pDCs show increases at the immunized site. (A) A significant decrease in the CD25, FoxP3–expressing T-cell infiltrate was noted when comparing skin biopsies taken from the immunization site before and after treatment (week 2). (B) S100+ and CD1a+ DC numbers also decreased at these time points, whereas CD123+ pDC numbers increased. Images were acquired using a model BX51 microscope with a 100×/1.25 NA Plan oil objective lens and Microfire digital camera with PictureFrame Version 2.3 software (Olympus). Digitized images were processed using Photoshop 7 image processing and manipulation software (Adobe Systems).
To separately identify the tissue effects of low-dose local RT from those of the combination of CpG + RT, we obtained skin biopsies of MF lesion before and after local RT in patients who were not enrolled in the study. Four paired biopsies at pretreatment and at week 2 after low-dose RT (2 Gy × 2) were obtained. Both markers of DCs showed a trend toward a decrease after RT (median S100+, 22.8/hpf vs 5.0/hpf; median CD1a+, 18.5/hpf vs 5.5/hpf). In contrast, there was no trend toward a decrease in CD25+ (46.3/hpf vs 41.3/hpf) or FoxP3+ (54.5/hpf vs 58.5/hpf) T cells, nor was there a trend toward an increase in CD123+ cells (36.3/hpf vs 23.3/hpf).
We assessed for histologic or IHC parameters at the immunized site that might have been associated with systemic clinical response. Our semiquantitative analysis suggested a trend toward greater reduction of CD25+ T cells (mean for responder, 1.6 ± 0.9 vs nonresponder, 0.7 ± 0.5; P = .03) and skin DCs (s100; mean for responder, 1.0 ± 0.7 vs nonresponder, 0.3 ± 0.5; P = .2) at the immunized site in clinical responders versus nonresponders.
Antitumor humoral response
We and others have reported that meaningful humoral antitumor immune responses can be generated in patients treated with vaccination strategies. We assessed for anti-lymphoma antibody response by evaluating MF skin tissue for bound antibody and the sera after immunization. Biopsy specimens taken before and after immunization were analyzed by direct immunofluorescence for IgG, IgM, and C3 for 7 patients with available frozen tissue and by IHC for C4d in 13 patients with available paired paraffin-embedded specimens. IgG, IgM, C3, or C4d deposition were not increased in these post versus preimmunization specimens. We further assessed for anti-lymphoma antibodies present in post versus preimmunization serum using indirect immunofluorescence. In 11 patients with available sera and baseline frozen lymphoma biopsy specimen, we were not able to detect anti-lymphoma IgG reactivity.
Anti-lymphoma humoral response was further assessed by flow cytometric analysis using tumor cells isolated from fresh biopsies in 8 patients. We found no serum antibody that could bind to CD4+ or CD3+/CD8− T cells, which includes the tumor population.
Peripheral blood pDCs and B cells are responsive to activation by CpG
The possibility existed that pDCs in patients with lymphoma may be dysfunctional and not be responsive to CpG. To explore this, we isolated pDCs from the peripheral blood in MF patients and healthy controls and studied their responsiveness to CpG. Data from 6 MF and 5 healthy subjects were available (Figure 6). The TLR9 sensitivity was assessed by increases in CD83 expression after exposure in vitro to TLR9 agonist (0 vs 3 vs 10 μg/mL CpG). The responsiveness of to CpG ODN was similar in MF compared with healthy controls in both pDCs and B cells; the median fold-activation of pDC in MF versus healthy controls was 2.60 versus 3.71 (P = .440), whereas that of B cells was 5.10 versus 5.34 (P = .75). Overall, the B cells were more sensitive to TLR9 agonist than pDCs, both in MF and healthy controls.
Dose-responsive activation of peripheral blood pDCs and B-cells by CpG. These are dose-response histograms showing activation of pDCs and B cells (measured by expression of CD83) with incremental amounts of CpG. In this study, leukocytes were isolated from heparinized peripheral blood from patients or healthy controls by Ficoll gradient and cultured in complete media at 37°C, 5% CO2 for 18 hours with 0, 3, or 10 μg/mL CpG ODN PF-3512676. Afterward, cells were washed and stained with the following antibody panel: CD3, CD14, CD16, CD56 (lin)–FITC, CD83-PE, CD123-PE-Cy7, HLA-DR-allophycocyanin, and CD19-AMCyan. Then, the sensitivity was assessed on an LSR-II flow cytometer. The responsiveness of TLR9 to CpG was similar in MF compared with healthy controls in both pDCs and B cells.
Dose-responsive activation of peripheral blood pDCs and B-cells by CpG. These are dose-response histograms showing activation of pDCs and B cells (measured by expression of CD83) with incremental amounts of CpG. In this study, leukocytes were isolated from heparinized peripheral blood from patients or healthy controls by Ficoll gradient and cultured in complete media at 37°C, 5% CO2 for 18 hours with 0, 3, or 10 μg/mL CpG ODN PF-3512676. Afterward, cells were washed and stained with the following antibody panel: CD3, CD14, CD16, CD56 (lin)–FITC, CD83-PE, CD123-PE-Cy7, HLA-DR-allophycocyanin, and CD19-AMCyan. Then, the sensitivity was assessed on an LSR-II flow cytometer. The responsiveness of TLR9 to CpG was similar in MF compared with healthy controls in both pDCs and B cells.
Discussion
We have demonstrated that an in situ vaccination strategy using low-dose local RT bracketed with intratumoral injection of CpG is feasible and safe in patients with MF. The most common toxicities were expected from past experience, including injection site reactions and flu-like symptoms.12 Objective systemic clinical responses were noted in one third of enrolled patients. These responses were observed in patients who had been refractory to a median of 5 prior treatments. These results in patients with MF complement our earlier report in systemic B-cell lymphoma14 in which we demonstrated tumor regressions with a similar in situ vaccination maneuver, using involved LNs for the immunization procedure. In CTCL, we took advantage of the easily accessible, multiple skin lesions for additional immunization procedure and tissue studies.
The prior vaccination studies in CTCL have been based on the use of DCs that involved significant ex vivo maneuvering to produce a customized vaccine product. Maier et al studied vaccination of CTCL patients using intranodal injection of autologous tumor lysate–pulsed DCs.8 Five of their 10 patients had objective clinical responses, including 1 patient with durable CR. In another phase 1/2 study,9 7 patients with SS were treated with patient-specific DCs co-incubated with autologous tumor cells, matured using T-helper 1–polarizing cocktail. Patients were immunized using high-resolution ultrasound-guided intranodal injections. One patient had an objective PR, 3 had SD, and 3 experienced PD.
Our in situ approach embraces the concept of tumor antigen–pulsed DC strategy; however, it does not involve the production of a customized vaccine product, and it is augmented by the potent immune-stimulatory effects of CpG ODN. Prior studies with RT have shown that tissue DCs are not killed by radiation but induced to migrate to the regional LNs.17,18 It has been shown that irradiation alone can render the tumor cells more immunogenic19 and that RT may be a useful tool to combine with immunotherapy.20,21 Furthermore, the TLR9-mediated activation of tissue DCs by CpG ODN can enhance cross-priming of tumor antigens and can lead to improved systemic antitumor responses.11 Moreover, because the RT is applied only to a local site, our clinical trial design allowed measurement of systemic immune and clinical effects at untreated sites of disease.
We believe but cannot prove from this trial that the systemic clinical responses were the result of our in situ vaccination rather than an effect from CpG monotherapy. In our previous trial of CpG monotherapy given at uninvolved skin sites, we did not observe clinically meaningful responses at the 6-mg dose used in the current trial.12 The response rate of 36% that we observed is similar to that reported with other biologic agents (eg, interferons, retinoids) that are used as standard therapies in MF. However, the response durations in our trial were short, with a median of only 7 weeks. A second immunization boost did not meaningfully improve the systemic antitumor response.
In our parallel study using the similar in situ vaccination strategy in patients with low-grade B-cell lymphoma,14 tumor-reactive immune responses were induced. In that study, some patients showed continued disease regression. Not all clinically responding patients demonstrated tumor-reactive CD8 T cells, but there was a correlation between the ability of tumor cells to induce autologous T cells to express a Treg phenotype and clinical responses. We were unable to perform similar assays in our MF study because of the technical difficulty of obtaining sufficient tumor cells from small sample sizes of skin biopsies.
The lack of clinical responses in the transformed subset of MF patients is consistent with previous failures of systemic biologic therapies such as interferons, retinoids, or targeted therapies in these patients.4 Factors predictive of response in other immunization therapies, such as patient age, baseline tumor burden, or number and type of prior therapies, were not significant in our study.
Because skin is more accessible to sampling than LNs, we had the opportunity of performing a more rigorous local tissue assessment in this CTCL project compared with our B-cell lymphoma study. MF cells in the skin have been shown to express a Treg phenotype including CD4/CD25 and FoxP322 as was demonstrated by the prominent epidermal CD4+ atypical T cells in our patients. Our tissue studies of the immunized site demonstrated significant reduction in CD25- and FoxP3-expressing CD4+ T cells with treatment. Loss of these CD25/FoxP3+ T cells may reflect a depletion of MF cell, infiltrating Tregs, or both with our immunization therapy. Skin specimens from other patients who underwent local irradiation without CpG did not reveal a similar reduction in CD25- or FoxP3-expressing CD4+ T cells, indicating that these changes were not from RT alone. By our semiquantitative assessment, the reduction in CD25-expressing T cells was more dramatic in the patients who attained objective clinical responses compared with those who had SD or PD (P = .03). Although, this trend was not supported by the more quantitative, hpf enumeration assessment, it may be clinically meaningful and worthy of further evaluation. Furthermore, the loss of Tregs may reflect a decrease in local immune-suppressed microenvironment and hence increase in immune reactivity.
The loss of DC density reflected by a decrease in CD1a+ and S100+ cells after CpG + RT immunization may be a result of local RT or CpG alone or the combined effect. Prior reports support that irradiation alone can induce immunologic responses, including facilitating DC migration to regional LNs.17,18,20 Nonspecific inflammation also has been shown to deplete tissue DCs; thus, this finding also can be secondary to inflammation caused by the intratumoral CpG alone. Our tissue data with low-dose local irradiation suggest that RT alone can decrease DC numbers, although perhaps not as dramatically as in combination with CpG treatment. Interestingly, there was a trend toward a greater reduction in DCs after immunization in the clinical responders versus nonresponders. This may imply that in the clinical responders, a more efficient cross-presentation and priming of tumor antigen occurred at the immunized site followed by migration of DCs to the regional LNs, resulting in an improved systemic immune and clinical response. Thus, a greater reduction of DC or Treg markers at the immunized site may serve as potential tissue surrogate markers of clinical response.
We were able to demonstrate that the pDCs from MF patients can be activated by the type B CpG ODN used in our vaccination strategy. This observation is vital given the reports of DC defects in cancer23,24 that can cripple strategies that rely on DC activation. The TLR9 sensitivity was greater in B cells than in pDCs, as expected with B-class CpG ODN and may indicate that B-cell lymphomas are better targets for this in situ vaccination strategy.14 The increase in CD123+ pDC population at the immunized site reflects possible recruitment of these CpG-sensitive pDCs from the peripheral blood into the local tissue, thus serving as substrate for continued immune activation with additional CpG injections.
In this initial clinical study, CpG-based in situ vaccination was feasible in patients with MF with acceptable toxicities. Given the clinical responses in subset of patients, it may warrant further investigation with modification to optimize the immunologic and therapeutic response. Strategies to enhance T-effector capacity or use of agents with greater ability to target myeloid DCs can be considered. Furthermore, the data showing depletion of tissue Tregs after immunization in MF coupled with our data of inferior outcome in Treg-inducing B-cell tumors14 prompt us to consider strategies to augment depletion of Tregs, such as anti-CTLA4 antibodies25 or denileukin diftitox26 in combination with our in situ vaccination therapy. If successful, our in situ immunization maneuver offers convenience and practicality compared with methods that require the production and delivery of a customized vaccine product.
An Inside Blood analysis of this article appears at the front of this issue.
Presented in part in oral format at the 52nd Annual Meeting of the American Society of Hematology, Orlando, FL, December 6, 2010.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by National Institutes of Health grant P01-CA34233 (Y.H.K., R.L., R.J.T., and D.K.C.).
National Institutes of Health
Authorship
Contribution: Y.H.K. designed and performed research, analyzed data, and wrote the paper; Y.H.K., R.L., R.T.H., and W.A. designed the study; D.G., C.H., J.B., D.K.C., W.A., A.M., F.A., R.H.A., S.S., and D.N. performed research and collected and analyzed data; R.T.H. oversaw the radiation therapy aspect of the trial; Y.H.K., D.G., and C.H. designed the figures; D.G., L.X., R.J.T., and B.L. performed the statistical analysis; and R.L., D.G., J.B., and Y.H.K. performed critical review of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Youn H. Kim, Multidisciplinary Cutaneous Lymphoma Program, 900 Blake Wilbur Dr, Rm 1010, Stanford, CA 94305; e-mail: younkim@stanford.edu.
References
Author notes
D.G. and C.H. contributed equally to this study.