In this issue of Blood, Ridges et al report the first successful use of a medium throughput zebrafish screen to identify novel compounds effective against human leukemia.1
The zebrafish, historically a robust developmental patterning model, has in recent years begun to show its strength as a useful disease model, particularly for cancer.2 One of the great promises of this model is its potential for use in drug discovery.3 For example, whole transgenic embryos carrying oncogenes and fluorescent reporters can be arrayed in 96-well plates and used to screen small molecule libraries for novel compounds that reduce tumor load. Unlike cell-based screens, whole-animal screens can yield valuable additional information such as pharmacokinetic and organ-toxicity data, but up to now no antileukemia lead compound has been successfully identified by medium throughput screening. These new results augur the general use of zebrafish as a platform for cancer drug discovery.
Zebrafish and humans show striking similarity in hematopoietic development, and zebrafish have cognates of all human adult blood lineages, including T and B lymphocytes.4 For these reasons, it is conceivable that drugs that show hematopoietic effects in zebrafish might have similar effects on human cells. Indeed, a pharmacologic screen for drugs that could cause alterations in hematopoietic stem cell (HSC) numbers during embryonic specification revealed that prostaglandins can expand HSC populations,5 and protocols based on this observation are now in clinical trials for use in expanding human HSCs for transplantation therapy (http://clinicaltrials.gov/ct2/show/results/NCT00890500).
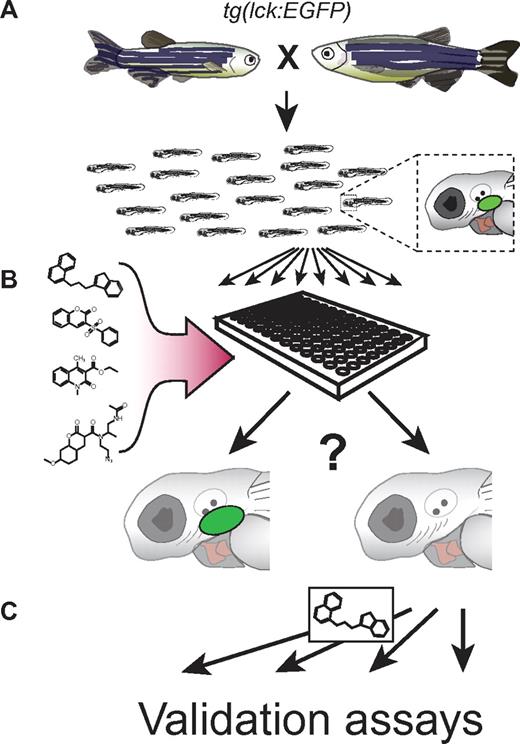
In their groundbreaking work, Ridges and colleagues reasoned that because T-acute lymphoblastic leukemia (T-ALL) generally involve immature blasts, looking for compounds that prevent T-cell maturation during embryonic development in zebrafish might identify compounds that would have similar effects on the immature blasts found in T-ALL. They took advantage of a transgenic zebrafish line (lck:EGFP) carrying an EGFP transgene under the control of the T cell–specific lck promoter and treated embryos with library compounds to determine whether any had the capacity to block T-cell development, readily visualized by fluorescence in lck:EGFP fish (figure panel A). Their survey of 25 000 small molecules (figure panel B) revealed that a compound with previously unappreciated biologic activity, 1H-indole-3-carbaldehyde 8-quinolinylhydrazone, which they termed Lenaldekar (LDK), is able to specifically ablate immature T cells.
Zebrafish screen for potential T-ALL therapeutics. (A) Adults carrying a transgene that fluorescently labels T cells (lck:EGFP) are mated. Resulting embryos have fluorescent T cells in the thymus (green oval in magnified embryo schematic). Immature T cells in embryos are posited to be similar to malignant lymphoblasts. (B) Five-day-old embryos are arrayed into 96-well plates and incubated with different compounds from a small molecule library. Forty-eight hours later, embryos are observed to determine general health, and examined for normal (left embryo) or decreased (right embryo) T-cell numbers, visible as reduced fluorescence. (C) Effective compounds are further verified and tested in follow-up assays.
Zebrafish screen for potential T-ALL therapeutics. (A) Adults carrying a transgene that fluorescently labels T cells (lck:EGFP) are mated. Resulting embryos have fluorescent T cells in the thymus (green oval in magnified embryo schematic). Immature T cells in embryos are posited to be similar to malignant lymphoblasts. (B) Five-day-old embryos are arrayed into 96-well plates and incubated with different compounds from a small molecule library. Forty-eight hours later, embryos are observed to determine general health, and examined for normal (left embryo) or decreased (right embryo) T-cell numbers, visible as reduced fluorescence. (C) Effective compounds are further verified and tested in follow-up assays.
In follow-up studies, Ridges et al verified LDK antileukemic activity in a variety of settings (figure panel C). LDK showed activity against a zebrafish T-ALL model carrying a human cMYC oncogene under the control of the rag2 promoter, with 15% of treated fish displaying stable tumor load and 85% showing significant decreases. Remarkably, while all untreated animals had succumbed to their cancer by 40 days, the LDK-treated group remained in long-term remission months after the 14-day treatment course had ended. Likewise, 4-week LDK treatment yielded 4-fold lower tumor loads in mice xenografted with a human T-ALL cell line. Finally, LDK showed activity not only against multiple T-ALL cell lines and primary tumors in vitro, but also against diverse additional leukemias, including T315I mutated, BCR-ABL positive, therapy-refractory B-ALL and CML samples. Thus, LDK shows promise for a variety of hematologic malignancies.
Ideally, anticancer therapeutics should specifically target unwanted proliferative cells, with few off-target effects. LDK activity appears to be highly specific. In cell culture, LDK, compared with an AKT inhibitor, showed equivalent toxicity toward malignant lymphoblasts. But unlike the AKT drug, LDK was not nearly as lethal toward mature T cells in peripheral blood at the lymphoblast-lethal dose. LDK appears to work in 2 ways: by inhibition of the PI3K/AKT/mTOR pathway and by cell-cycle delay in G2/M. Interestingly, cell-cycle effects appeared to be relatively specific for lymphoblasts, because cell-cycle defects were not observed in LDK-treated zebrafish embryos during development, before the emergence of lymphoblasts. Moreover, because the original screen was performed in whole animals, LDK was preselected for its lack of general toxicity. This tolerability was confirmed in mammals where injection or oral administration produced reasonably long-lasting serum levels of drug, but had no obvious organ toxicity in a variety of assays. Thus LDK appears to be a highly effective antileukemic agent, with few off-target effects.
The data presented by Ridges and colleagues demonstrate that zebrafish are an exceptional cancer and drug discovery model. Previously it has been shown that zebrafish get cancer,2 that human oncogenes cause malignancy in zebrafish,2 that novel oncogenes can be discovered by mutagenesis,6 and that known human cancer therapeutics can be effective in fish.7 High throughput means of transplanting, injecting, and screening embryos are rapidly developing.3,8 Here, Ridges et al show that novel human anticancer therapeutics can be discovered de novo using small molecule screening in zebrafish.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■