Abstract
Adenosine acts as anti-inflammatory mediator on the immune system and has been described in regulatory T cell (Treg)–mediated suppression. In the absence of adenosine deaminase (ADA), adenosine and other purine metabolites accumulate, leading to severe immunodeficiency with recurrent infections (ADA-SCID). Particularly ADA-deficient patients with late-onset forms and after enzyme replacement therapy (PEG-ADA) are known to manifest immune dysregulation. Herein we provide evidence that alterations in the purine metabolism interfere with Treg function, thereby contributing to autoimmune manifestations in ADA deficiency. Tregs isolated from PEG-ADA–treated patients are reduced in number and show decreased suppressive activity, whereas they are corrected after gene therapy. Untreated murine ADA−/− Tregs show alterations in the plasma membrane CD39/CD73 ectonucleotidase machinery and limited suppressive activity via extracellular adenosine. PEG-ADA–treated mice developed multiple autoantibodies and hypothyroidism in contrast to mice treated with bone marrow transplantation or gene therapy. Tregs isolated from PEG-ADA–treated mice lacked suppressive activity, suggesting that this treatment interferes with Treg functionality. The alterations in the CD39/CD73 adenosinergic machinery and loss of function in ADA-deficient Tregs provide new insights into a predisposition to autoimmunity and the underlying mechanisms causing defective peripheral tolerance in ADA-SCID. Trials were registered at www.clinicaltrials.gov as NCT00598481/NCT00599781.
Introduction
CD4+CD25+FoxP3+ regulatory T cells (Tregs) actively suppress pathologic and physiologic immune responses to maintain peripheral immune self-tolerance and prevent autoimmunity.1,2 Several molecules and mechanisms have been shown to operate in Treg-mediated control of immune responses.3 In vitro functional studies have shown that Tregs suppress effector cells via the secretion of immunosuppressive cytokines, by cell contact-dependent Treg/antigen-presenting cells (APCs) or Treg/T-cell interactions, and functional modification or killing of APCs.4
Extracellular adenosine produced by Tregs has been described as one of the mechanisms mediating their suppressive activity. Concordant expression of the ectoenzymes CD39 and CD73 has been reported both for murine and human Tregs.5-7 The CD39 ectoenzyme produces AMP from ATP or ADP, which is subsequently converted into extracellular adenosine by the CD73 ectoenzyme.8 Treg function requires the coordinated expression of the adenosine 2A receptor (Adora2A) on activated T effector cells to enable adenosine-mediated immunosuppression.2 Moreover, human Tregs have been shown to express low levels of adenosine deaminase (ADA), the enzyme responsible for adenosine breakdown. In contrast, T effector cells are enriched in ADA but express low levels of CD39 and CD73.7 This molecular profile of human Treg (CD39+CD73+ADAlow) has functional significance, as it confers Tregs the capability to produce and sustain relatively high concentrations of extracellular adenosine.7
ADA catalyzes the irreversible deamination of adenosine and deoxyadenosine into inosine and deoxyinosine, respectively. Further conversion of these deaminated nucleosides leads to hypoxanthine, which can be either transformed irreversibly into uric acid or salvaged into mononucleosides.9 In the absence of ADA, adenosine and deoxyadenosine accumulate in plasma and cells, forming the metabolic basis underlying immune cell defects and severe combined immunodeficiency (ADA-SCID). Immunologic defects associated with this disease include impaired T-, B-, NK-cell development and function and complete absence of cellular and humoral immunity.9,10 In ADA-deficient patients, as in other forms of SCID, bone marrow transplantation (BMT) from an HLA-identical sibling donor is the treatment of choice, but available only for a minority of patients.11 The administration of enzyme replacement therapy with pegylated bovine ADA (PEG-ADA) results in clinical improvement with approximately 70% to 80% survival but often incomplete immunologic reconstitution. Recent trials represented the first demonstration of long-term clinical efficacy of hematopoietic stem cell gene therapy (GT) for ADA-SCID, underlining that GT has a favorable safety profile and is effective in restoring purine metabolism and immune function.12
Manifestations of immune dysregulation, autoimmunity, and allergic manifestations are key findings in milder forms of the disease but have also been reported in patients under PEG-ADA treatment.13-16 Little is known on their pathogenesis or to what extent some mechanisms of tolerance might be specifically affected by ADA deficiency.10 Because peripheral tolerance is primarily mediated by Tregs, which possess a unique biochemical signature among T cells in that they generate and sustain high adenosine concentrations, we hypothesized that the autoimmune manifestations associated with ADA deficiency might be the result of an altered purine metabolism interfering with normal Treg function. Herein we provide evidence for specific defects in the regulatory T-cell compartment of ADA-deficient mice and patients. Furthermore, we show that enzyme replacement treatment with PEG-ADA, but not GT or BMT, severely interferes with normal Treg function.
Methods
ADA−/− mice
ADA-deficient mice have been described previously.17 Breeding pairs for FVB;129-Adatm1MW-TgN(PLADA)4118Rkmb were purchased from Jackson ImmunoResearch Laboratories. Procedures were performed according to protocols approved by the Committee for Animal Care and Use of San Raffaele Scientific Institute (IACUC 406). Treatment procedures were performed as described.18 See also supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Patients
The patient's population includes ADA-SCID children and adult cases (Table 1). Patients treated with GT were enrolled in GT protocols (www.clinicaltrials.gov; NCT00598481/NCT00599781) approved by the HSR Ethical Committee and by the competent authority (Italian Istituto Superiore di Sanità). GT treatment was performed as described.12 None of the patients was under immunomodulatory therapy at the time of analysis. The protocol for research studies on biologic material from patients with primary immunodeficiency (TIGET02), including ADA-SCID, is approved by the HSR Institutional Ethical Committee. Biologic specimens from HDs (adult/children) were collected and used on informed consent for research purpose in agreement with the rules defined by approved protocols TIGET01 and TIGET PERIBLOOD.
Immunohistochemical studies
FoxP3 and CD3 stainings on thymi of ADA+/+ and ADA−/− mice were performed as described.19 See also supplemental Methods. Thyroids from treated ADA−/− and control mice were collected at death and stained with cleaved caspase-3 (AbD Serotec) antibody. The slides were developed using HRP-conjugated secondary antibody and were counterstained with hematoxylin. Positive nuclei were scored by means of Aperio image Analysis Nuclear algorithm (Aperio Technologies).
Gene expression analyses
RNA was purified from whole frozen thymus using EUROzol (Euroclone). RT-PCR into cDNA and real-time PCR reactions using Assay-on-Demand gene expression arrays (Applied Biosystems) were carried out as described previously.20 Arrays used included the following: FoxP3 (Mm00475156_m1), CD4 (Mm00442754_m1), and HPRT (Mm00446968_m1) as internal housekeeping control.
FACS analyses
FACS stainings were performed as described previously.20 A complete list of antibodies can be found in supplemental Methods.
ADA enzymatic activity
ATP hydrolysis assay
Experiments measuring ATP conversion by Tregs were performed as described.7 ATP consumption and AMP and adenosine generation were measured by high-performance capillary electrophoresis as described in “ADA enzymatic activity.” See also supplemental Methods.
In vitro suppression assays
In vitro suppression assays with murine and human Tregs are detailed in supplemental Methods.
Immunoglobulin isotyping
Serum IgG1, IgG2a, IgG2b, IgG3, IgA, IgE, and IgM levels were analyzed by multiplex assay kit (Beadlyte Mouse Immunoglobulin Isotyping Kit; Upstate Biotechnology) as described.22
Anti-ADA and anti-platelet ELISA
The 96-well polystyrene plates were coated with 0.1 μg/mL of bovine ADA (Calbiochem). Alternatively, 10 μg/mL of proteic extract from platelets isolated with Tyrode buffer was used as coated antigen. Titrated sera were added, and positivity was revealed by staining with secondary goat anti–mouse IgG-AP antibody (Southern Biotechnology). See also supplemental Methods.
Anti–TSH ELISA
ELISA kit for mouse thyroid-stimulating hormone (TSH) was purchased from USCNLIFE and performed on serum samples according to the manufacturer's instructions.
Indirect immunofluorescence for organ-specific autoantibodies
Immunohisotchemical studies
FoxP3 and CD3 stainings on thymi of ADA+/+ and ADA−/− mice were performed as described.19 See also supplemental Methods. Thyroids from treated ADA−/− and control mice were collected at death and stained with cleaved caspase-3 (AbD Serotec) antibody. The slides were developed using HRP-conjugated secondary antibody and were counterstained with hematoxlin.
Microscope image acquisition
Immunohistochemical images to thymi were acquired by an Olympus DP70 camera mounted on an Olympus BX60 microscope (Olympus) using a dry 10× objective and AnalySIS imaging software (Soft Imaging System GmbH).
Immunohistochemical images of thyroids were acquired by an AxioCam MRc5 camera mounted on Zeiss Axioplan-2 microscope (Carl Zeiss Microimaging) using dry 5× or 40× objectives and AxioVision imaging software (Carl Zeiss Microimaging). Cleaved caspase-3–positive nuclei were scored by means of Aperio image Analysis Nulear algorithm (Aperio Technologies).
Statistical analyses
All group results are expressed as mean ± SD if not stated otherwise. Student t test was used for comparisons between groups. For group values that did not follow a Gaussian distribution, Mann-Whitney U test (2-tailed) was used. A P value < .05 was considered significant.
Results
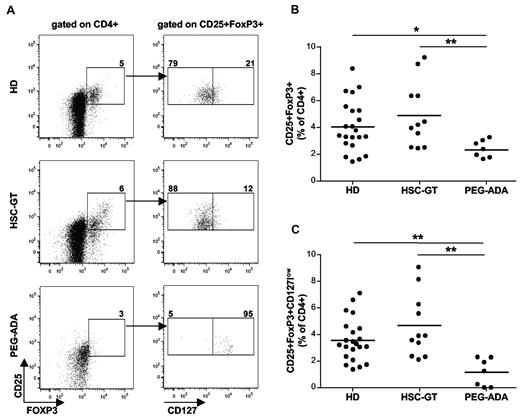
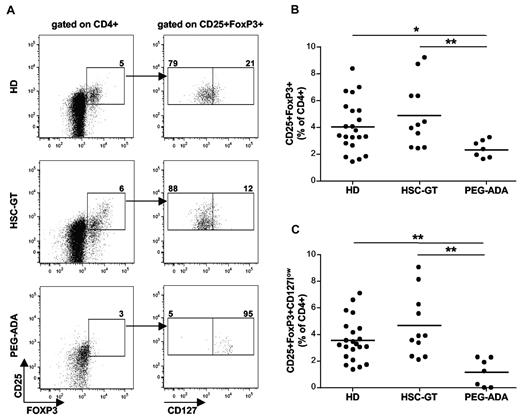
Treg compartment of ADA-SCID patients after PEG-ADA and GT
Although immune dysregulation and autoimmune manifestations are frequent findings in ADA-deficient patients with milder forms or in patients under PEG-ADA, mechanisms causing the loss of peripheral tolerance and onset of autoimmunity have remained elusive. We therefore studied the Treg compartment in our cohort of patients, including 7 PEG-ADA–treated and 11 retroviral GT-treated patients (Table 1). Figure 1A shows the gating strategy used to assess the percentage of Tregs in both groups of ADA-SCID patients and healthy pediatric donors (HD). When defined as CD25+FOXP3+ Tregs, their mean percentage in the CD4+ gate was similar between GT-treated patients and pediatric HD analyzed in parallel (Figure 1B). However, we observed a significantly lower Treg frequency in PEG-ADA–treated patients compared with GT-treated patients or HDs. When additionally considering the low or absent expression of CD127 to exclude activated effector cells from the analysis,24 PEG-ADA–treated patients showed an even lower percentage of CD25+FOXP3+CD127low Tregs compared with GT-treated patients and HD (Figure 1C).
Phenotype of Tregs in ADA-SCID patients after different treatments. (A) Representative FACS staining and gating strategy of Tregs in a pediatric HD, GT, and PEG-ADA–treated patient. Total PBMCs were stained for CD4, CD25, CD127, and FOXP3. Gates were established on the basis of isotype-identical monoclonal antibody controls. Treg frequencies are indicated. (B) Percentage of CD25+FOXP3+ Tregs in the CD4+ gate of 22 HD, 11 GT, and 7 PEG-ADA–treated patients. Horizontal bars indicate mean values. *P < .05. **P < .005. (C) Percentage of Tregs identified by the low or absent expression of CD127 in the CD25+FOXP3+ gate. Horizontal bars indicate mean values. **P < .005.
Phenotype of Tregs in ADA-SCID patients after different treatments. (A) Representative FACS staining and gating strategy of Tregs in a pediatric HD, GT, and PEG-ADA–treated patient. Total PBMCs were stained for CD4, CD25, CD127, and FOXP3. Gates were established on the basis of isotype-identical monoclonal antibody controls. Treg frequencies are indicated. (B) Percentage of CD25+FOXP3+ Tregs in the CD4+ gate of 22 HD, 11 GT, and 7 PEG-ADA–treated patients. Horizontal bars indicate mean values. *P < .05. **P < .005. (C) Percentage of Tregs identified by the low or absent expression of CD127 in the CD25+FOXP3+ gate. Horizontal bars indicate mean values. **P < .005.
Alterations in ectonucleosidase expression in Tregs from PEG-ADA–treated patients
As shown in representative histogram analyses in supplemental Figure 1A, we also evaluated the expression of CD39 and CD73 in Tregs of our patient cohort. The percentage of CD39 and CD73 expressing Tregs in the CD4+CD25+FOXP3+ population was not significantly different between all groups (data not shown). But Tregs from PEG-ADA–treated patients showed an increased MFI for both markers (Student t test: CD39, P = .05; CD73, P = .02), although there were no significant differences in MFI expression levels between the GT-treated group and HD (supplemental Figure 1B-C). Linear correlation analysis indicated that the higher expression of CD39 corresponds with a higher expression of CD73 in PEG-ADA–treated patients (R2 = 0.99; Pearson: Pr = 0.995), which was not observed in cells obtained from healthy controls. To assess whether increased CD39 and CD73 expression in PEG-ADA–treated patients influences the turnover of adenine nucleotides and adenosine levels, we measured ATP, AMP, and adenosine in the plasma of these patients compared with HD. As shown in supplemental Figure 1D, GT-treated patients showed adenine nucleotide levels similar to HD, whereas PEG-ADA patients showed reduced levels of ATP and AMP. This observation is consistent with the observed higher expression of CD39, hence increased ectonucleotidase activity. Moreover, we observed an increased concentration of adenosine in the plasma of PEG-ADA–treated patients. This finding is in agreement with the increased CD73 expression but also suggests a lower level of adenosine detoxification by PEG-ADA with respect to GT.
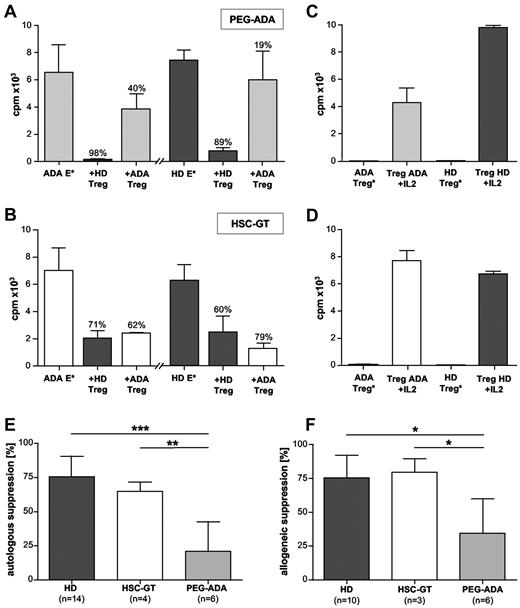
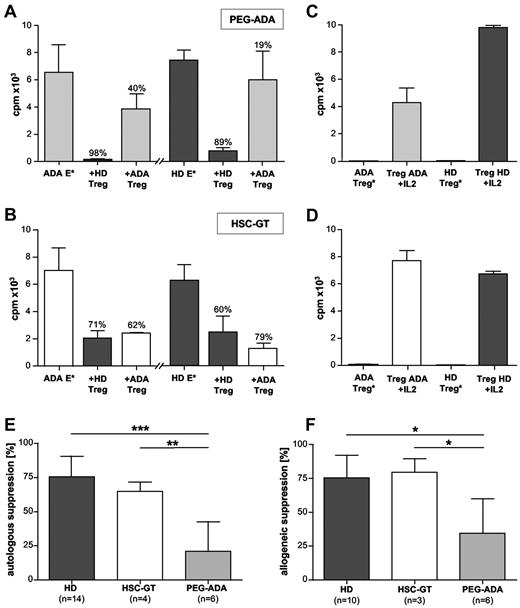
Low Treg function in ADA-SCID patients after PEG-ADA treatment but not GT
To assess Treg functionality in suppression assays, CD4+ enriched cells were FACS sorted for CD25 and CD127 expression to separate Tregs from responder T cells. Compared with HD, Treg functionality was evaluated for PEG-ADA or GT-treated patients in autologous and, when sufficient cell numbers were available, also in allogeneic settings. Figure 2A-B shows representative suppression assays of a PEG-ADA and GT-treated patient, respectively, both compared with HDs. Figure 2C and D shows Treg anergy and its reversion in the presence of IL-2. Although gene-corrected and control Tregs strongly suppressed the proliferation of cocultured autologous responder T cells, Tregs from the PEG-ADA–treated patient were unable to suppress (Figure 2A-B).
Treg function in ADA-SCID patients after different treatments. (A) Representative autologous and allogeneic suppression assays for a PEG-ADA–treated patient compared with an HD. E* indicates effector cells stimulated with allogeneic accessory cells (APCs) and soluble anti-CD3. Percentages of suppression are indicated. Data are intraexperimental mean ± SD. (B) Representative autologous and allogeneic suppression assays for a GT-treated patient compared with an HD. Percentages of suppression are indicated. (C-D) Stimulated Tregs (Treg*) of the same PEG-ADA-treated (C) and GT-treated (D) patients with their respective HDs and reversion of Treg anergy by IL-2. (E-F) Summarized percentages for autologous (E) and allogeneic (F) suppression assays in PEG-ADA– and GT-treated patients compared with healthy controls. Data are interexperimental mean ± SD. ***P < .0005 (Mann-Whitney test). **P < .005 (Mann-Whitney test). *P < .05 (Mann-Whitney test).
Treg function in ADA-SCID patients after different treatments. (A) Representative autologous and allogeneic suppression assays for a PEG-ADA–treated patient compared with an HD. E* indicates effector cells stimulated with allogeneic accessory cells (APCs) and soluble anti-CD3. Percentages of suppression are indicated. Data are intraexperimental mean ± SD. (B) Representative autologous and allogeneic suppression assays for a GT-treated patient compared with an HD. Percentages of suppression are indicated. (C-D) Stimulated Tregs (Treg*) of the same PEG-ADA-treated (C) and GT-treated (D) patients with their respective HDs and reversion of Treg anergy by IL-2. (E-F) Summarized percentages for autologous (E) and allogeneic (F) suppression assays in PEG-ADA– and GT-treated patients compared with healthy controls. Data are interexperimental mean ± SD. ***P < .0005 (Mann-Whitney test). **P < .005 (Mann-Whitney test). *P < .05 (Mann-Whitney test).
It has previously been reported that, after an average of 4 months of treatment, proliferative responses normalize in some PEG-ADA–treated patients before declining over time.25 To exclude a possible contribution of proliferation defects in the PEG-ADA–treated effector T cells, we tested the same patients in allogeneic settings (Figure 2A-B). Similarly to autologous suppression assays, HD and gene-corrected Tregs suppressed allogeneic effector cells, whereas Tregs from PEG-ADA–treated patients did not. Summaries of all suppression assays performed in 14 HD, 4 GT patients between 2 and 4 years after GT, in whom the majority of CD4+ cells were genetically corrected12 and 6 patients under PEG-ADA are shown in Figure 2E and F.
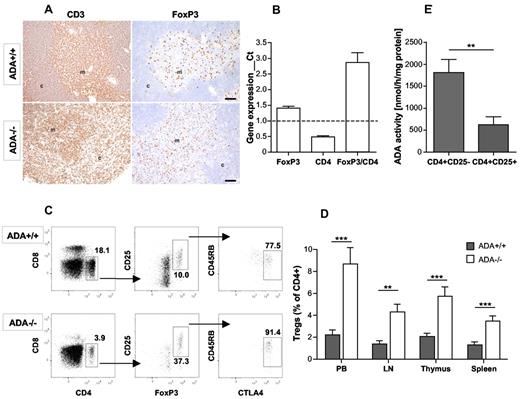
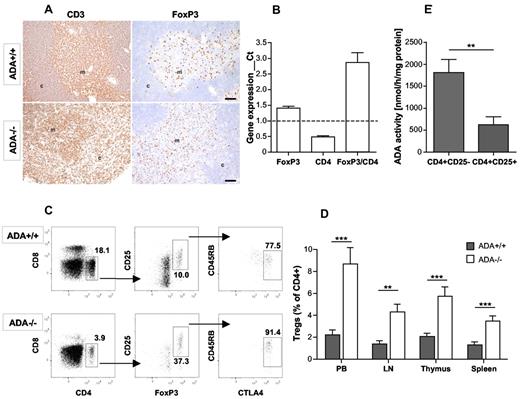
Enrichment of Treg cells in untreated ADA−/− mice
To dissect the cellular mechanisms leading to loss of function in Tregs from PEG-ADA–treated patients, we moved to the more accessible ADA−/− mouse model. ADA−/− mice retain many features associated with ADA deficiency in humans, including T- and B-cell lymphopenia and a profound metabolic defect.17 Elevated adenosine levels cause abnormal alveolar development, leading ADA−/− mice to die postnatally within 3 weeks. In contrast to the analyzed human samples, we took advantage from the possibility to study ADA−/− mice before and after treatment with PEG-ADA, GT, and BMT. To assess a possible origin of immune dysregulation resulting from impaired Treg development, we investigated the thymic architecture and CD4+CD25+FoxP3+ Treg compartment in untreated ADA−/− mice. ADA−/− thymi are approximately 50% smaller than age-matched controls.17 As shown by anti-CD3 staining, ADA−/− thymi are severely lymphopenic, resulting in a misbalance of effector and regulatory compartments with an increased proportion of FoxP3+ cells compared with wild-type (WT; Figure 3A). The observed misbalance in ADA−/− thymi was confirmed by gene expression analyses of FoxP3 with respect to CD4 in total ADA−/− thymi (Figure 3B). Whereas FoxP3 expression was slightly increased in total thymus from ADA−/− mice, the CD4 compartment was significantly smaller, which resulted in a 3-fold higher FoxP3/CD4 ratio compared with WT.
Expansion of the Treg compartment in untreated ADA−/− mice. (A) Anti-CD3 and FoxP3 immunohistochemistry in thymi of 3-week-old ADA+/+ and ADA−/− mice (original magnification ×10). (B) TaqMan gene expression analysis for CD4 and FoxP3 on total thymi of ADA−/− (n = 6) mice compared with ADA+/+ (n = 6). ADA+/+ gene expression was arbitrarily considered 1 as represented by the dashed line. Data are mean ± SD. (C) Representative FACS analysis for CD4+CD25+FoxP3+CTLA4+CD45RBlow Tregs in ADA+/+ and ADA−/− PB. (D) Percentage of CD25+FoxP3+CTLA4+CD45RBlow Tregs in CD4+ compartment in PB, lymph nodes (LN), thymus, and spleen of ADA+/+ (n = 11) and ADA−/− (n = 11) mice. Data are mean ± SD. **P = .005-.0005. ***P ≤ .0005. (E) ADA enzymatic activity in ADA+/+ CD4+CD25− T effector (n = 3) and CD4+CD25+ T regulatory cells (n = 3). Data are mean ± SD. **P = .008.
Expansion of the Treg compartment in untreated ADA−/− mice. (A) Anti-CD3 and FoxP3 immunohistochemistry in thymi of 3-week-old ADA+/+ and ADA−/− mice (original magnification ×10). (B) TaqMan gene expression analysis for CD4 and FoxP3 on total thymi of ADA−/− (n = 6) mice compared with ADA+/+ (n = 6). ADA+/+ gene expression was arbitrarily considered 1 as represented by the dashed line. Data are mean ± SD. (C) Representative FACS analysis for CD4+CD25+FoxP3+CTLA4+CD45RBlow Tregs in ADA+/+ and ADA−/− PB. (D) Percentage of CD25+FoxP3+CTLA4+CD45RBlow Tregs in CD4+ compartment in PB, lymph nodes (LN), thymus, and spleen of ADA+/+ (n = 11) and ADA−/− (n = 11) mice. Data are mean ± SD. **P = .005-.0005. ***P ≤ .0005. (E) ADA enzymatic activity in ADA+/+ CD4+CD25− T effector (n = 3) and CD4+CD25+ T regulatory cells (n = 3). Data are mean ± SD. **P = .008.
The proportion of FoxP3+ cells was also analyzed by FACS analyses for CD4+CD25+FoxP3+, CTLA-4, and CD45RB in the peripheral blood (PB) and lymphoid organs of ADA+/+ and ADA−/− mice. A representative FACS analysis for PB is shown in Figure 3C. A significantly increased frequency of CD4+CD25+FoxP3+CTLA4+CD4RB−/low Tregs was also observed in the PB, lymph nodes, and spleen of ADA−/− mice (Figure 3D). Interestingly, FoxP3 expression, as measured by MFI, was significantly higher in ADA−/− Treg compared with WT (data not shown). Indicating that the previously reported mechanism on extracellular adenosine inducing FoxP3 expression in adaptive Tregs26 might also apply to naturally occurring Tregs.
The relative increase of Treg cells in the context of severe lymphopenia of conventional T cells is particularly noteworthy. Recent studies have demonstrated that different T-cell subsets are subject to distinct homeostatic controls in vivo,27 and this may contribute to an imbalance of Tregs and effector T cells in some instances.1 The increased proportion of Treg cells in the CD4 compartment of ADA−/− mice might be the result of a different susceptibility to cellular stress and apoptosis compared with conventional T cells.28 This hypothesis is supported by our finding that ADA activity is significantly lower in murine Treg cells with respect to CD4+CD25− effector T cells (Figure 3E), indicating a lower dependency of Tregs on the ADA enzyme. Their reduced tendency to cell division probably decreases their need for deoxynucleotide recycling, thereby protecting Tregs from the toxic effects of deoxyadenosine accumulation and contribute to their prolonged survival in an ADA-deficient environment.
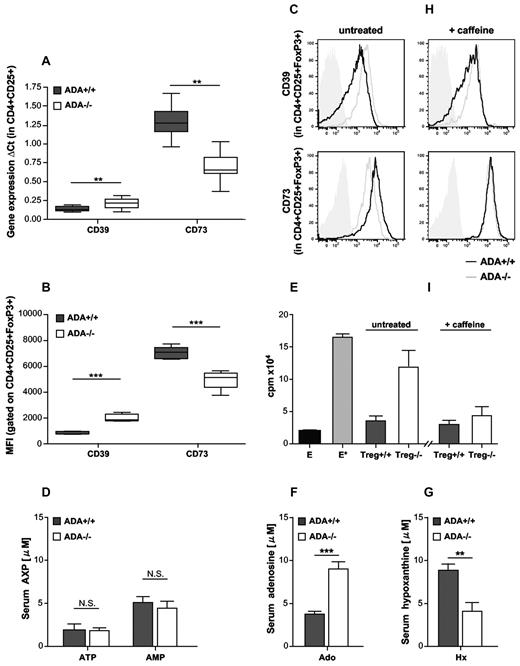
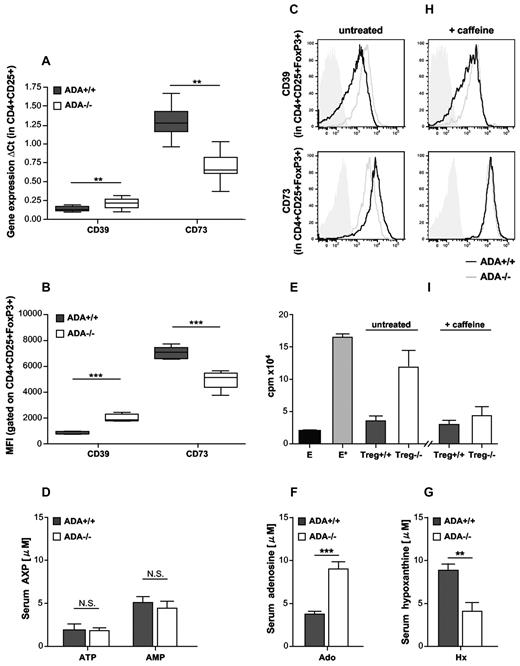
Altered CD39 and CD73 expression and decreased Treg function in ADA−/− mice
To assess whether the absence of ADA and subsequent accumulation of its metabolites cause alterations in the adenosinergic machinery of murine ADA−/− Tregs, we measured the RNA and protein expression levels of CD39 and CD73. As shown in Figure 4A and Figure 4B for RNA or protein, respectively, ADA−/− Tregs showed significantly higher expression of CD39, while expressing significantly less CD73. A representative histogram analysis for CD39 and CD73 in the CD4+CD25+FoxP3+ compartment is shown in Figure 4C.
Altered CD39 and CD73 expression and decreased suppressive function of ADA−/− Tregs. (A) TaqMan gene expression analysis for CD39 (ADA+/+: n = 15, ADA−/−: n = 16; **P = .0047) and CD73 (ADA+/+: n = 9, ADA−/−: n = 10. **P = .0045) in purified CD4+CD25+ Tregs; box and whiskers graphs. (B) Summarized MFI of CD39 and CD73 gated on CD4+CD25+FoxP3+ cells from ADA+/+ (n = 5) and ADA−/− (n = 5) mice; box and whiskers graphs. (C) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from untreated ADA+/+ and ADA−/− mice. Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (D) AXP levels divided into ATP and AMP illustrate ectonucleotidase activity in serum samples from ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. *P < .05. (E) Representative suppression assay using ADA+/+ effector cells cocultured with Tregs from untreated ADA+/+ (n = 3) or ADA−/− mice (n = 5). E indicates unstimulated effector cells; and E*, effector cells stimulated with anti-CD3 and anti-CD28. Data are interexperimental mean ± SD. (F) Serum adenosine levels in ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. ***P < .0005. (G) Serum hypoxanthine levels in ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. **P < .005. (H) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from ADA+/+ and ADA−/− mice treated with 50 mg/kg of caffeine (nonselective Adora antagonist). Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (I) Representative suppression assay using ADA+/+ effector cells cocultured with Tregs from ADA+/+ (n = 4) or ADA−/− mice (n = 6) treated with 50 mg/kg of caffeine. Data are intraexperimental mean ± SD.
Altered CD39 and CD73 expression and decreased suppressive function of ADA−/− Tregs. (A) TaqMan gene expression analysis for CD39 (ADA+/+: n = 15, ADA−/−: n = 16; **P = .0047) and CD73 (ADA+/+: n = 9, ADA−/−: n = 10. **P = .0045) in purified CD4+CD25+ Tregs; box and whiskers graphs. (B) Summarized MFI of CD39 and CD73 gated on CD4+CD25+FoxP3+ cells from ADA+/+ (n = 5) and ADA−/− (n = 5) mice; box and whiskers graphs. (C) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from untreated ADA+/+ and ADA−/− mice. Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (D) AXP levels divided into ATP and AMP illustrate ectonucleotidase activity in serum samples from ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. *P < .05. (E) Representative suppression assay using ADA+/+ effector cells cocultured with Tregs from untreated ADA+/+ (n = 3) or ADA−/− mice (n = 5). E indicates unstimulated effector cells; and E*, effector cells stimulated with anti-CD3 and anti-CD28. Data are interexperimental mean ± SD. (F) Serum adenosine levels in ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. ***P < .0005. (G) Serum hypoxanthine levels in ADA−/− (n = 7) and age-matched ADA+/+ mice (n = 8) at 3 weeks of age. Data are mean ± SD. **P < .005. (H) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from ADA+/+ and ADA−/− mice treated with 50 mg/kg of caffeine (nonselective Adora antagonist). Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (I) Representative suppression assay using ADA+/+ effector cells cocultured with Tregs from ADA+/+ (n = 4) or ADA−/− mice (n = 6) treated with 50 mg/kg of caffeine. Data are intraexperimental mean ± SD.
In the absence of ADA, adenosine and other purine metabolites such as ATP accumulate. We hypothesized that the increased CD39 expression contributes to the conversion of accumulating adenine nucleotides spilling over into alternative pathways. Indeed, ATP hydrolysis was increased in ADA−/− Tregs (data not shown), and serum ATP and AMP levels in ADA−/− mice were comparable with WT, thereby indicating intact CD39 ectonucleotidase activity (Figure 4D). Despite the increased percentage of Tregs with respect to CD4 effector cells in ADA−/− mice, we addressed whether low expression of CD73 might interfere with their relative suppressive activity. We therefore performed in vitro suppression assays using 50 000 ADA+/+ or ADA−/− CD4+CD25+ Tregs together with 50 000 stimulated ADA+/+ responder cells (untreated ADA−/− effector cells proliferate poorly upon TCR triggering). On average, the suppressive activity of ADA−/− Tregs toward WT effector cells was more than 75% reduced compared with WT Tregs (P = .0004; representative suppression assay is shown in Figure 4E).
Treatment with the nonselective Adora antagonist caffeine restores CD73 expression and Treg function in ADA−/− mice
Adenosine elicits its physiologic responses by binding to and activating one or more of the 4 transmembrane adenosine receptors, Adora1, Adora2a, Adora2b, and Adora3.8 Cells of the immune system express these receptors and are responsive to the modulatory effects of adenosine in an inflammatory environment. Lack of ADA manifests as a block of adenosine conversion in the uric acid pathway.9 Serum adenosine levels are therefore significantly increased in ADA−/− mice, whereas downstream products of adenosine conversion by ADA, such as hypoxanthine, are significantly reduced (Figure 4F-G). To assess whether the observed alterations in the adenosinergic machinery of ADA−/− Tregs were the result of their sensitivity to accumulating adenosine, we used caffeine, a nonselective adenosine receptor antagonist, to treat ADA+/+ and ADA−/− mice.
Daily intraperitoneal caffeine treatment had little effect on CD39 expression, which remained significantly different from caffeine-treated WT mice (Student t test: caffeine-treated ADA+/+ vs caffeine treated ADA−/−, P < .0001). CD73 expression, on the other hand, was increased to comparable levels in ADA+/+ and ADA−/− mice, which was even significantly higher than in their untreated counterparts (Student t test: ADA+/+ vs caffeine-treated ADA+/+, P < .0001; and ADA−/− vs caffeine-treated ADA−/−, P < .0001). A representative histogram analysis for CD39 and CD73 in the CD4+CD25+FoxP3+ compartment is shown in Figure 4H. Consistently, ADA−/− or ADA+/+ Tregs from caffeine-treated animals suppressed the proliferation of WT effector cells at comparable levels (Figure 4I). These results thereby indicate that Tregs can sense extracellular adenosine via Adora signaling. Blocking of Adora signaling by caffeine treatment increases CD73 expression both in WT and ADA−/− mice, whereas accumulating adenosine levels, hence increased Adora signaling, deceases CD73 expression in ADA−/− mice. In agreement with the defective suppressive activity in human Tregs without CD73 expression (E.T., manuscript in preparation), our data confirm that low CD73 levels correlate with a reduced suppressive activity of ADA−/− Tregs.
Murine model for autoimmunity in ADA deficiency using long-term PEG-ADA treatment
Untreated ADA−/− mice die within only 3 weeks of age because of a severe pulmonary insufficiency. At death, the severe immune deficiency and organ alterations are the most prominent features, whereas no apparent autoimmune manifestations can be observed. We therefore rescued ADA−/− mice with PEG-ADA, lentiviral GT, or BMT to assess which treatment is most efficacious in preventing the development of autoimmunity in these mice. For the present study, ADA−/− mice in the PEG-ADA–treated group starting from postnatal day 10, received 1000 U/kg intraperitoneally per week, which has been reported to provide metabolic detoxification and T-, B-, and NK-cell reconstitution.29 BMT with WT BM and lentiviral GT were performed as described previously.18,20
As shown in supplemental Figure 2A, the long-term survival of PEG-ADA–, GT-, and BMT-treated mice was comparable between the 3 groups (60%-70% with respect to WT). This outcome was the result of an early mortality in the BMT- and GT-treated groups, whereas PEG-ADA–treated mice had a less stable long-term survival. To monitor treatment efficacy and metabolic and immunologic reconstitution, surviving mice were bled at 10, 14, and 18 weeks after treatment. Supplemental Figure 2C-E compares the metabolic reconstitution in PEG-ADA–, BMT-, and GT-treated mice with WT controls. ADA activity in RBCs from GT- and BMT-treated mice was comparable to ADA+/+. As expected from the fact that PEG-ADA remains in circulation without entering in cells, ADA activity in PEG-ADA–treated mice was exclusively detectable in the plasma. Reconstitution of enzymatic activity in BM, spleen, and thymus from BMT-treated mice is comparable with WT, although slightly lower in GT-treated mice. This observation is consistent with our previous report showing that the engraftment levels of vector-transduced cells in GT-treated mice are lower compared with ADA−/− mice treated with fresh ADA+/+ BM cells.18
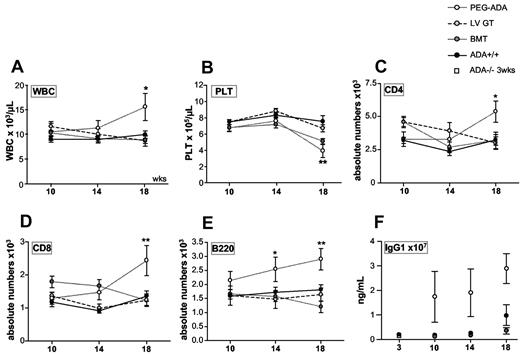
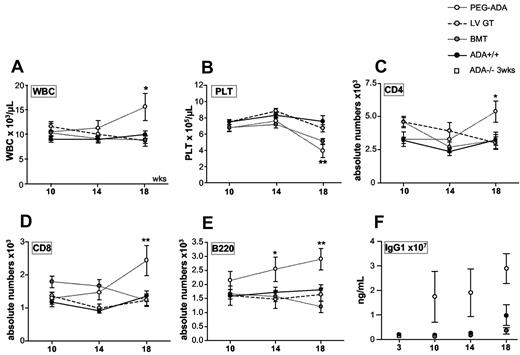
Whereas white blood cells (Figure 5A) in PEG-ADA–treated mice significantly increased over time, platelet counts (Figure 5B) significantly decreased. RBC counts remained stable over time (supplemental Figure 2B). FACS analyses of PB samples revealed a significant increase of total CD3+ T cells (supplemental Figure 2F), CD4+ T cells (Figure 5C), CD8+ cells (Figure 5D), total B220+ B cells (Figure 5E), and monocytes (supplemental Figure 2G) in PEG-ADA but not GT- or BMT-treated mice after 18 weeks of treatment. Granulocytes (supplemental Figure 2H) and NK cells (not shown) remained comparable among all groups.
Immunologic reconstitution in ADA−/− mice treated with PEG-ADA, GT, and BMT. (A) After 18 weeks (wks), white blood cell counts (WBC) significantly increase in PEG-ADA–treated mice (n = 12) compared with GT (n = 8) or BMT (n = 15) treated ADA−/− mice and ADA+/+ mice (n = 17). Data are mean ± SD. *P < .05. (B) Compared with control groups, platelet (PLT) counts in PEG-ADA–treated mice significantly decrease after 18 weeks of treatment. Data are mean ± SD. **P < .005. Absolute numbers of PB lymphocyte populations measured by FACS analyses as percentage of WBC counts, at weeks 10, 14, and 18. Data are mean ± SEM. (C) CD4+ T cells. (D) CD8+ T cells. (E) B220+ B cells. *P = .05-.005. **P = .005-.0005. (B-E) PEG-ADA–treated ADA−/− (n = 12), GT-treated ADA−/− (n = 8), BMT-treated ADA−/− (n = 15), and ADA+/+ mice (n = 17). (F) IgG1 (ng/mL × 107) serum immunoglobulin levels in PEG-ADA (n = 7), GT (n = 6), or BMT treated ADA−/− mice (n = 10) compared with ADA+/+ (n = 7) and 3-week-old ADA−/− (n = 6) and ADA+/+ (n = 6) mice. Data are mean ± SD.
Immunologic reconstitution in ADA−/− mice treated with PEG-ADA, GT, and BMT. (A) After 18 weeks (wks), white blood cell counts (WBC) significantly increase in PEG-ADA–treated mice (n = 12) compared with GT (n = 8) or BMT (n = 15) treated ADA−/− mice and ADA+/+ mice (n = 17). Data are mean ± SD. *P < .05. (B) Compared with control groups, platelet (PLT) counts in PEG-ADA–treated mice significantly decrease after 18 weeks of treatment. Data are mean ± SD. **P < .005. Absolute numbers of PB lymphocyte populations measured by FACS analyses as percentage of WBC counts, at weeks 10, 14, and 18. Data are mean ± SEM. (C) CD4+ T cells. (D) CD8+ T cells. (E) B220+ B cells. *P = .05-.005. **P = .005-.0005. (B-E) PEG-ADA–treated ADA−/− (n = 12), GT-treated ADA−/− (n = 8), BMT-treated ADA−/− (n = 15), and ADA+/+ mice (n = 17). (F) IgG1 (ng/mL × 107) serum immunoglobulin levels in PEG-ADA (n = 7), GT (n = 6), or BMT treated ADA−/− mice (n = 10) compared with ADA+/+ (n = 7) and 3-week-old ADA−/− (n = 6) and ADA+/+ (n = 6) mice. Data are mean ± SD.
Increased immunoglobulin and autoantibody production in PEG-ADA–treated mice
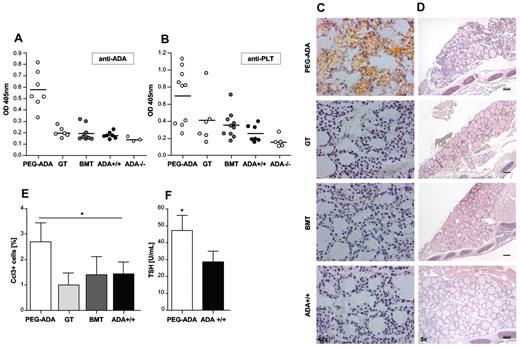
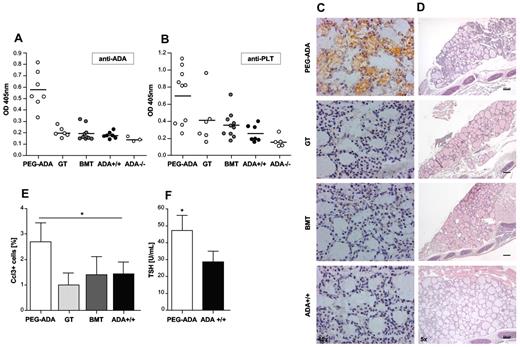
Breakdown of B-cell tolerance and autoantibody production is a characteristic of most autoimmune diseases.30 We therefore assessed the serum immunoglobulin levels in ADA−/− mice rescued with PEG-ADA, GT, and BMT by multiplex assays. In PEG-ADA–treated mice, serum IgG1, IgG2a, IgG3, IgA, IgE, and IgM subclasses were significantly increased at all time points tested (Figure 5F; supplemental Figures 3A-F), whereas BMT- and GT-treated mice were comparable with WT controls. Moreover, as described for ADA-SCID patients under enzyme replacement therapy,25 anti-ADA antibodies were detected in all PEG-ADA–treated animals by ELISA, whereas no antibodies were found in GT- and BMT-treated mice (Figure 6A). To address whether the reduced platelet counts in PEG-ADA–treated mice reported in Figure 5B could be associated with the development of autoantibodies, we measured the presence of anti-platelet antibodies by ELISA. As shown in Figure 6B, anti-platelet antibodies were detectable in 6 of 10 PEG-ADA–treated mice at 18 weeks of treatment. One sample from both the GT and BMT groups also tested positive for reactivity against platelets.
Increased antibody production in PEG-ADA–treated ADA−/− mice. (A) ELISA assessing antibody production against ADA in PEG-ADA (n = 7), GT (n = 6), and BMT (n = 10) treated ADA−/− mice compared with ADA+/+ mice (n = 7) and 3-week-old ADA−/− mice (n = 3); scatter plot; horizontal bars represent mean. (B) ELISA assessing autoantibody production against platelets in PEG-ADA (n = 10), GT (n = 6), and BMT (n = 10) treated ADA−/− mice compared with ADA+/+ mice (n = 7) and 3-week-old ADA−/− mice (n = 5); scatter plot; horizontal bars represent mean. (C) Autoantibody production directed against thyroid tissue in PEG-ADA but not GT- and BMT-treated ADA−/− or ADA+/+ mice. (D) Thyroid damage occurring in autoantibody-producing PEG-ADA–treated mice compared with a GT- or BMT-treated ADA−/− and WT control. (E) Percentage of apoptotic Ccl3-positive nuclei in the thyroid of PEG-ADA–treated ADA−/− (n = 7) compared with GT (n = 5) and BMT (n = 5) treated ADA−/− and ADA+/+ mice (n = 5). Data are mean ± SD. *P = .05. (F) Concentration of TSH in sera of PEG-ADA–treated ADA−/− mice (n = 14) compared with ADA+/+ mice (n = 8). Data are mean ± SD. *P = .05.
Increased antibody production in PEG-ADA–treated ADA−/− mice. (A) ELISA assessing antibody production against ADA in PEG-ADA (n = 7), GT (n = 6), and BMT (n = 10) treated ADA−/− mice compared with ADA+/+ mice (n = 7) and 3-week-old ADA−/− mice (n = 3); scatter plot; horizontal bars represent mean. (B) ELISA assessing autoantibody production against platelets in PEG-ADA (n = 10), GT (n = 6), and BMT (n = 10) treated ADA−/− mice compared with ADA+/+ mice (n = 7) and 3-week-old ADA−/− mice (n = 5); scatter plot; horizontal bars represent mean. (C) Autoantibody production directed against thyroid tissue in PEG-ADA but not GT- and BMT-treated ADA−/− or ADA+/+ mice. (D) Thyroid damage occurring in autoantibody-producing PEG-ADA–treated mice compared with a GT- or BMT-treated ADA−/− and WT control. (E) Percentage of apoptotic Ccl3-positive nuclei in the thyroid of PEG-ADA–treated ADA−/− (n = 7) compared with GT (n = 5) and BMT (n = 5) treated ADA−/− and ADA+/+ mice (n = 5). Data are mean ± SD. *P = .05. (F) Concentration of TSH in sera of PEG-ADA–treated ADA−/− mice (n = 14) compared with ADA+/+ mice (n = 8). Data are mean ± SD. *P = .05.
To assess whether rescued ADA−/− mice produce autoantibodies, which might cause organ damage, we incubated serum samples with tissue sections from the pancreas, intestine, stomach, thyroid, salivary, and adrenal glands. Positive reactivity for the thyroid, stomach, and intestine was detected in PEG-ADA–treated mice, whereas all other organs stained negative for autoantibodies.
As shown in Figure 6C and D, sera from PEG-ADA, but not GT- or BMT-treated ADA−/− mice, reacted against thyroid tissue, causing focal atresia of thyroid follicles and small nonsecreting follicles, indicating reduced organ functionality. Moreover, a significantly increased percentage of apoptotic cells was detected by staining for cleaved Caspase 3 (Ccl3+) and Aperio image analyses in thyroids from PEG-ADA–treated mice (Figure 6E). As shown in Figure 6F, significantly increased levels of serum TSH were detected in PEG-ADA–treated mice, indicating chronic thyroid dysfunction and unresponsiveness to TSH stimulation.
Autoantibodies against the gastrointestinal tract were detected exclusively in PEG-ADA–treated mice but did not result in autoimmune manifestations, such as inflammatory infiltration or colitis (supplemental Figure 4A-E). Nonetheless, it is noteworthy that, although PEG-ADA–treated mice initially gained weight quicker than their irradiated GT- or BMT-treated counterparts, they showed a tendency to lose weight after longer treatment, indicating a possible inhibition of nutrient uptake (supplemental Figure 4F). In approximately 20% of PEG-ADA–treated mice, anti-dsDNA antibodies were detected, whereas all BMT- and GT-treated ADA−/− mice, such as WT mice, tested negative (data not shown).
Defective Treg compartment in ADA−/− mice is corrected by BMT and GT but not by PEG-ADA
ADA−/− Tregs from untreated mice showed a significantly reduced CD73 expression and suppressive activity compared with WT cells. To address whether Treg defects contribute to the onset of autoimmune manifestations in PEG-ADA–treated mice, we analyzed their Treg compartment compared with healthy BMT- or GT-treated ADA−/− and WT mice.
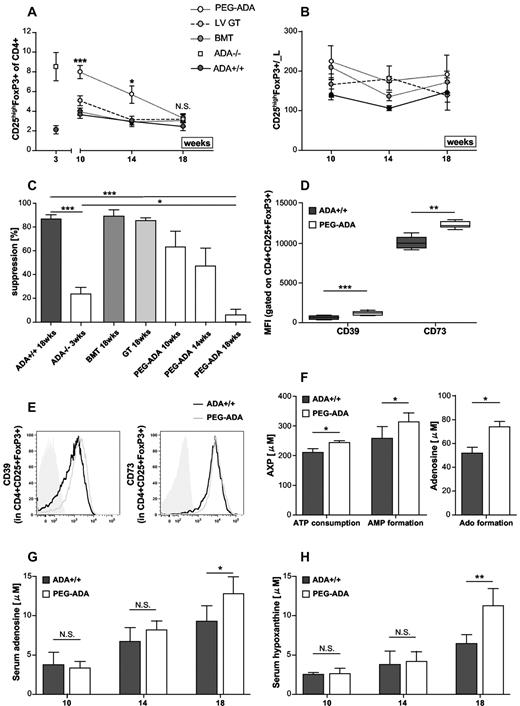
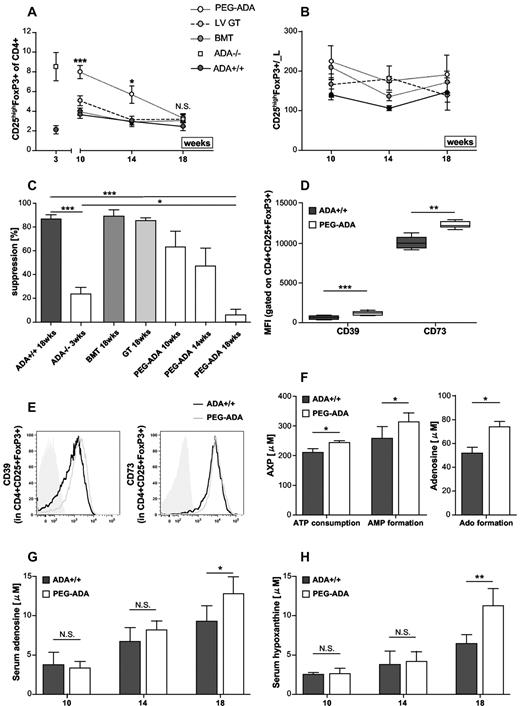
As shown in Figure 7A, ADA−/− mice treated with ADA+/+ or LV-transduced ADA−/− BM have a comparable percentage of Tregs in the CD4+ compartment as WT mice. PEG-ADA–treated animals initially showed a similar Treg percentage as untreated ADA−/− mice, which subsequently decreased to levels comparable with WT mice. Contemporarily, CD4+ T-cell counts significantly increased in PEG-ADA–treated mice, whereas their absolute number of Tregs remained considerably stable throughout followup (Figure 7B). Tregs from PEG-ADA–treated animals suppressed normally after 10 weeks of treatment, approximately 50% at 14 weeks, but by 18 weeks their suppressive function was completely abolished (Figure 7C). Whereas PEG-ADA treatment only temporarily rescued suppressive activity, Tregs from GT- or BMT-treated mice showed consistently normal suppressive activity similarly to WT Tregs. We therefore hypothesized that PEG-ADA might directly interfere with the adenosine-mediated suppression of effector cells because newly produced adenosine can become metabolized by PEG-ADA in the extracellular space.
Inhibition of Treg function in the presence of PEG-ADA. (A) Percentage of CD25+FoxP3+ Tregs in ADA−/− rescued with PEG-ADA (n = 20), lentiviral GT (n = 8), and BMT (n = 11) compared with ADA+/+ mice (n = 23). Data are mean ± SEM. ***P = .0001. *P = .05. N.S. indicates not significant. (B) Absolute numbers of Tregs. Data are mean ± SEM. (C) Suppressive function versus ADA+/+ effector cells of ADA+/+ (n = 11) and ADA−/− (n = 8) Tregs compared with Tregs from ADA−/− mice treated with BMT (n = 3), GT (n = 3), and PEG-ADA after 10 (n = 3), 14 (n = 3), and 18 (n = 7) weeks. Data are interexperimental mean ± SD. ***P < .0005. **P < .005. *P < .05. (D) Summarized MFI of CD39 and CD73 gated on CD4+CD25+FoxP3+ cells from ADA+/+ (n = 6) mice compared with ADA−/− mice treated with PEG-ADA for 18 weeks (n = 4). (E) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from ADA+/+ and ADA−/− mice treated with PEG-ADA for 18 weeks. Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (F) Measurement of ATP consumption and AMP formation (left panel) as well as adenosine formation (right panel) by purified CD4+CD25+ Treg cells from PEG-ADA–treated ADA−/− (n = 4) and ADA+/+ mice (n = 3). Data are interexperimental mean ± SD. *P < .05. (G) Serum adenosine levels in PEG-ADA–treated ADA−/− (n = 4) and age-matched ADA+/+ mice (n = 4) at 10, 14, and 18 weeks of follow-up. Data are interexperimental mean ± SD. *P < .05. (H) Serum hypoxanthine levels in PEG-ADA–treated ADA−/− (n = 4) and age-matched ADA+/+ mice (n = 4) at 10, 14, and 18 weeks of follow-up. Data are interexperimental mean ± SD. **P < .005.
Inhibition of Treg function in the presence of PEG-ADA. (A) Percentage of CD25+FoxP3+ Tregs in ADA−/− rescued with PEG-ADA (n = 20), lentiviral GT (n = 8), and BMT (n = 11) compared with ADA+/+ mice (n = 23). Data are mean ± SEM. ***P = .0001. *P = .05. N.S. indicates not significant. (B) Absolute numbers of Tregs. Data are mean ± SEM. (C) Suppressive function versus ADA+/+ effector cells of ADA+/+ (n = 11) and ADA−/− (n = 8) Tregs compared with Tregs from ADA−/− mice treated with BMT (n = 3), GT (n = 3), and PEG-ADA after 10 (n = 3), 14 (n = 3), and 18 (n = 7) weeks. Data are interexperimental mean ± SD. ***P < .0005. **P < .005. *P < .05. (D) Summarized MFI of CD39 and CD73 gated on CD4+CD25+FoxP3+ cells from ADA+/+ (n = 6) mice compared with ADA−/− mice treated with PEG-ADA for 18 weeks (n = 4). (E) Representative histogram plots for CD39 and CD73 on CD4+CD25+FoxP3+ splenocytes from ADA+/+ and ADA−/− mice treated with PEG-ADA for 18 weeks. Isotype-identical monoclonal antibodies served as controls (solid gray histogram). (F) Measurement of ATP consumption and AMP formation (left panel) as well as adenosine formation (right panel) by purified CD4+CD25+ Treg cells from PEG-ADA–treated ADA−/− (n = 4) and ADA+/+ mice (n = 3). Data are interexperimental mean ± SD. *P < .05. (G) Serum adenosine levels in PEG-ADA–treated ADA−/− (n = 4) and age-matched ADA+/+ mice (n = 4) at 10, 14, and 18 weeks of follow-up. Data are interexperimental mean ± SD. *P < .05. (H) Serum hypoxanthine levels in PEG-ADA–treated ADA−/− (n = 4) and age-matched ADA+/+ mice (n = 4) at 10, 14, and 18 weeks of follow-up. Data are interexperimental mean ± SD. **P < .005.
Elevated adenosine turnover by PEG-ADA interferes with ADA−/− Treg function
As shown in Figure 7D, Tregs from PEG-ADA–treated animals maintained increased expression of CD39 and up-regulated CD73 expression compared with age-matched WT controls. RNA expression levels were increased, although not significantly for both markers (data not shown). A representative histogram analysis for CD39 and CD73 in the CD4+CD25+FoxP3+ compartment is shown in Figure 7E.
Because CD39 and CD73 appeared up-regulated to allow for increased adenosine production, we assessed ATP hydrolysis by purified Tregs from ADA+/+ and PEG-ADA–treated ADA−/− mice. Indeed, CD39 activity measured by ATP consumption and AMP formation was increased in Treg from PEG-ADA–treated mice (Figure 7F). Consistently, adenosine formation by CD73 was also significantly increased compared with WT Tregs (Figure 7F). To assess adenosine turnover in the presence of extracellular ADA, we measured adenosine and hypoxanthine levels in sera from WT and PEG-ADA–treated mice. As shown in Figure 7G, serum adenosine levels in PEG-ADA–treated mice were comparable to WT at 10 and 14 weeks of follow-up, indicating adequate detoxification from accumulating purine metabolites. We observed an age-related increase of adenosine levels in both groups, but at 18 weeks of follow-up serum adenosine levels in PEG-ADA–treated mice were significantly elevated compared with WT. As shown in Figure 7H, the block of adenosine conversion present in ADA−/− mice (Figure 4F-G) was overcome by PEG-ADA treatment. But with adenosine levels increasing over time, a significantly enhanced turnover and hypoxanthine production were observed. In long-term treated ADA−/− mice, the increasing adenosine metabolization coincides with the up-regulation of CD73 expression, therefore suggesting a higher requirement for adenosine conversion. The elevated ATP hydrolysis by these cells and instantaneous adenosine turnover by PEG-ADA in the extracellular space support our hypothesis that PEG-ADA interferes with the adenosine-mediated suppression of effector cells.
Discussion
Immune dysregulation, including autoimmunity, and allergic manifestations are a frequent finding in milder forms of ADA deficiency, although commonly observed also in patients on PEG-ADA.13,14 To prevent autoimmune complications in these patients and to compare current treatment regimens, we aimed to provide new insights into the pathogenesis and underlying mechanisms causing the onset of autoimmunity. Particularly, we assessed to what extent Treg-mediated mechanisms of peripheral tolerance might be specifically affected in ADA deficiency.
Herein we describe a possible predisposition to autoimmunity in ADA−/− mice resulting from functional alterations in the Treg compartment. Despite CD4+ lymphopenia, Tregs were proportionally increased in all lymphoid organs and the PB, probably as consequence of a higher resistance to apoptosis or cellular stress. The finding that WT Tregs express a lower ADA activity compared with effector T cells supports this hypothesis. Cycling ADA−/− effectors with a higher dependency on the ADA enzyme can be expected to undergo apoptosis mediated by deoxynucleotide accumulation more easily than ADA−/− Tregs with a reduced tendency to cell division.
Moreover, we show that Tregs are sensitive to extracellular adenosine concentrations and that at least CD73 expression is regulated by this metabolite. The underlying mechanism accounting for increased CD39 expression in ADA−/− Tregs remains to be elucidated. Intracellular cAMP levels, which are elevated in the absence of ADA, have been reported to increase CD39 expression.31 Interestingly, ATP has recently been described to influence the suppressive potential and stability of Tregs, which might also interfere with Treg function in ADA deficiency.32 Although both CD39 and CD73 are rate limiting for extracellular adenosine generation, CD73 is the last component of the ectoenzymatic chain. With adenosine accumulating in ADA−/− mice, possibly to avoid a further increase of extracellular concentrations, CD73 is reduced and ADA−/− Tregs display a decreased suppressive activity toward T effector cells.
Nevertheless, untreated ADA−/− mice do not manifest any signs of autoimmunity, when they die at approximately 3 weeks of age. FoxP3-deficient mice die between 16 and 24 days of age from uncontrolled lymphoproliferation and multiorgan infiltration, indicating that 3 weeks are sufficient for autoimmunity to develop in the absence of Tregs.33 In ADA−/− mice, on the other hand, the almost complete absence of effector T- and B-cell populations might allow Tregs despite their lower suppressive activity to maintain peripheral tolerance. Reconstitution of effector T and B cells after PEG-ADA, GT, and BMT treatment alongside defects in Treg function can therefore be considered prerequisites for the manifestation of autoimmunity.
Indeed, mice treated with long-term PEG-ADA developed higher T- and B-cell counts, abnormal immunoglobulin levels, and autoantibody production compared with control groups. This mouse model for autoimmunity in ADA−/− mice resulting from long-term use of PEG-ADA partially re-creates the phenomena reported in humans and therefore will be essential for future studies on the in vivo effects of PEG-ADA on immune cell function. The obtained results revealed an elevated adenosine catabolism in PEG-ADA–treated mice, characterized by high adenosine production as part of the ADA-deficient disease background and a significantly increased turnover by the enzymatic activity of PEG-ADA. Although short-term PEG-ADA treatment initially rescued Treg-mediated suppression compared with untreated ADA−/− mice, their functionality became exhausted by long-term PEG-ADA treatment.
These results confirmed our observation in ADA-SCID patients, showing that Tregs isolated from PEG-ADA–treated patients suppress the proliferation of effector cells significantly less than Tregs from GT-treated patients and HD. In addition, the percentage of CD4+CD25+FOXP3+CD127−/low Tregs was significantly reduced in PEG-ADA–treated patients, which might additionally lower Treg control over T effector proliferation in vivo. As described herein for Tregs from PEG-ADA–treated mice, we observed a significantly increased expression of the CD39 and CD73 ectonucleotidase in ADA-SCID patients. Alterations in the adenosinergic machinery coincided with adenosine accumulation and increased turnover by PEG-ADA. Up-regulation of CD73 in treated ADA−/− mice and patients can therefore be interpreted as a compensatory mechanism representing a higher requirement for ATP/ADP to adenosine conversion in the presence of extracellular PEG-ADA. These findings fit well with our hypothesis that PEG-ADA present in the extracellular space eliminates adenosine produced by this ectoenzymatic chain and hinders adenosine-mediated suppression by interfering between adenosine and Adora2a expressed on T effector cells. Despite the initial rescue of suppressive activity by up-regulation of CD73 for elevated adenosine production, long-term PEG-ADA treatment interfered with Treg function by augmenting adenosine turnover. Thus, Tregs require a balanced adenosine metabolism because excessively high adenosine concentrations, as found in untreated ADA−/− mice, or excessive conversion of extracellular adenosine by PEG-ADA interferes with their suppressive function.
ADA-SCID remains a challenging condition to treat.11 With the occurrence of neutralizing anti-ADA antibodies and autoimmune manifestations, immunologic reconstitution in PEG-ADA patients is considered variable. Moreover, high costs and a lifelong burden associated with weekly PEG-ADA treatment represent major drawbacks for this choice of therapy. Our data show a superior efficacy of BMT and GT over PEG-ADA treatment in allowing the development of functional Tregs and in preventing the onset of autoimmunity in ADA−/− mice. Nevertheless, it shall be noted that some autoimmune manifestations have also been reported in BMT patients34,35 as well as in patients treated with hematopoietic stem cell GT.12 Accurate survey and long-term follow-up will be essential to determine the incidence of autoimmune complications after different treatments. Moreover, future studies on additional aspects of T- and/or B-cell tolerance and autoimmunity will be necessary to continue the adjustment of current therapeutic options.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Miriam Casiraghi and Francesca Ferrua, all physicians and nurses of the Pediatric Clinical Research Unit of HSR-TIGET for patient care, Dr Shimon Slavin and Dr Memet Aker at the Hadassah University Hospital for patient specimens, Chiara Villa for FACS sorting, and Martina Rocchi for processing histopathologic specimens.
This work was supported by the Italian Telethon Foundation (TIGET, core grant A1), the independent drug research program of the Italian Medicines Agency (FARM5JRXRM), and the European Commission: Advanced Cell–based Therapies for the treatment of Primary ImmunoDeficiency (CELL-Pin; HEALTH F5-2010-261387).
Authorship
Contribution: A.V.S. designed and performed research, analyzed data, and wrote the paper; I.B. designed and performed experiments and analyzed data; N.C. and R.J.H. performed animal experiments; S.S. processed patient material; D.C. performed Aperio image analysis; F.S. and P.L.P. performed histologic analyses; N.G. designed experiments; A.T. and F.C. conducted the biochemical studies; M.G.R. and A.V. contributed to the study design; E.T. performed ELISAs and contributed to the study design; A.A. designed the research, analyzed data, and revised the paper; and all authors checked the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alessandro Aiuti, San Raffaele Telethon Institute for Gene Therapy, Via Olgettina 58, 20132 Milano, Italy; e-mail: a.aiuti@hsr.it.
References
Author notes
A.V.S. and I.B. contributed equally to this study.