Abstract
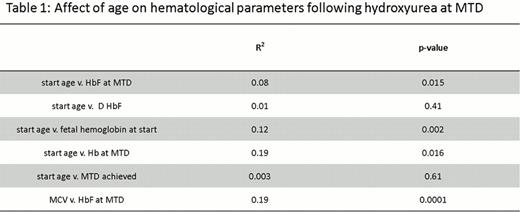
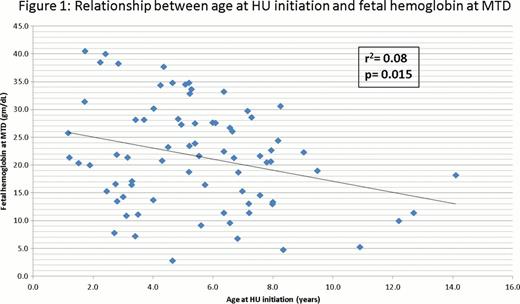
Hydroxyurea (HU) is approved for use in adults with Sickle Cell Disease (SCD) and increases the production of fetal hemoglobin (HbF). Increased HbF is associated with decreased clinical severity in adults and children with SCD, such as decreased numbers of vaso-occlusive events, transfusions, and hospitalizations. Higher HbF at initiation of HU is predictive of HbF response, but association between age of hydroxyurea initiation and HbF response has not been investigated. We hypothesize that starting hydroxyurea at an early age may improve hematological and clinical response. In order to determine if younger age at hydroxyurea initiation affects the percentage of HbF achieved with hydroxyurea, we conducted a retrospective cohort study. We identified subjects enrolled in the Duke University Medical Center Comprehensive Sickle Cell program who initiated hydroxyurea when they were less than 17.99 years of age and were prescribed hydroxyurea for at least six months. The following data were abstracted from the medical record between December 1996 and April 2011: age, hemoglobin, percentage HbF, and mean corpuscular volume (MCV) at start of HU and at maximum tolerated dose (MTD) of HU therapy. The correlation coefficient and p-values for various parameters were calculated. Seventy-three patients (41 males and 32 females) were included in the analysis. The mean age at hydroxyurea initiation was 5.5 years (1.2–14.1). The mean hydroxyurea dose at MTD was 28.6 ± 3.2 mg/kg/day. At initiation, the mean hemoglobin was 8.2 ± 1.2 g/dL, the mean MCV was 83±7.4 fl and mean HbF was 10 ± 5.7%. At MTD, the mean hemoglobin was 9.4 ± 1.1 g/dL, the mean MCV was 99 ± 11.1 fl, and the mean HbF was 21.7 ± 9.4%. As expected, at MTD, an elevated MCV was correlated with elevated fetal hemoglobin (r2= 0.19, p= 0.0001) [Table 1]. There was a statistically significant relationship between the age at HU initiation and the HbF at MTD (r2= 0.08, p= 0.015) [Figure 1] as well as the age at HU initiation and the hemoglobin at MTD (r2= 0.19, p= 0.016). The relationship between the age at starting HU and the overall change in HbF (DHbF) was not statistically significant (r2= 0.01, p= 0.41). There was not a statistically significant relationship between age at HU initiation and the MTD of HU (r2= 0.003, p= 0.61). The 6 patients started on HU at age less than 2 years (mean 1.5 ± 0.3 years) maintained a mean elevated HbF of 19.1 ± 5% at last documented follow-up with follow-up ranging from 1.4–13 year of uninterrupted hydroxyurea use. Starting hydroxyurea therapy at a younger age appears to improve HbF response as measured at MTD, although there is variability in the level of fetal hemoglobin attained. There is not an association seen with the DHbF or dose at MTD and age at hydroxyurea initiation. In summary, starting hydroxyurea at a younger age, when HbF is >20%, leads to persistence of HbF production and overall improvement in hematological efficacy. This was not simply the result of achieving MTD at a younger age before physiologic decline of HbF.
Off Label Use: Hydroxyurea for complications of sickle cell disease in pediatrics. Shah:Eisai: Research Funding; Adventrx: Consultancy.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.