Abstract
Abstract 1594
Follicular Lymphoma (FL) is the most frequent low-grade NHL. Clinical course is heterogeneous, some patients (pts) presenting an indolent clinical course with overall survival (OS) over 15 y and others developing a more aggressive disease with shorter survival. The Follicular Lymphoma International Prognostic Index (FLIPI) or FLIPI-2 are commonly used to predict pts outcome, but fail to identify pts with a really poor prognosis. At diagnosis, few FL pts present with detectable leukemic phase (FL-LP) and this characteristic has been seldom described.
The aim of the study was to describe the clinical features and outcome of FL-LP pts.
Among 499 pts diagnosed with FL according to the WHO criteria in the Centre Hospitalier Lyon Sud (transformation and grade 3b excluded) and treated between 01/1992 and 01/2012, 37 (7.4%) had characteristic FL-LP detected by cytological blood smears analysis with confirmation by flow cytometry (kappa/lambda clonality). Median age was 58 y and FLIPI score repartition was 4 pts in low, 16 in intermediate, and 17 in high risk groups. Splenomegaly was present in 23 pts, high tumour burden (GELF criteria) in 11, B symptoms in 8, and ECOG PS>1 in 3. Seven pts had anaemia, 17 platelets <150.109/L, 22 β2-microglobulin (β2-m) >UNL, and 11 LDH >UNL. The circulating lymphoma cells expressed the CD10 in 29/37 cases and surface Ig expression was detected in 31/35 cases, mainly IgM or IgG isotype. The median count of circulating lymphoma cells was 1.95.109/L, ranging from 0.6 to 129.109/L, 15 pts having count >4.109/L and 6 pts >10.109/L. Cytogenetic data were available for 21 pts, 20 carried the t(14;18), or its variant t(18;22), 16 of them having complex karyotype.
Two pts were on watchful waiting for 24 and 82 m and 35 received a chemotherapy regimen at diagnosis including rituximab in 27 cases. Overall response rate was 83% (29/35) with 23 CR/CRu. Median progression-free survival (PFS) was 29 m. PFS and OS estimates were 37% and 86% at 5 y and 31% and 68% at 10 y, respectively. Splenomegaly (P=.035), high tumour burden (P=.017), lymphoma cells count greater than 4.109/L (P=.028), β2-m>UNL (P=.036), and thrombocytopenia (<150.109/L) (P=.003) were all associated with a shorter PFS. Exploratory multivariate analysis identified thrombocytopenia (HR 6.62; P=.0014) and circulating lymphoma cells >4.109/L (HR 5.92; P=.000916) as independent prognostic factors. After progression, 12 pts received high-dose therapy (HDT) with HSCT as salvage with a long second PFS (68% at 10 y) compared to 8.3 m median PFS in first line. Pts not receiving HDT at salvage had a median second PFS of 27 m.
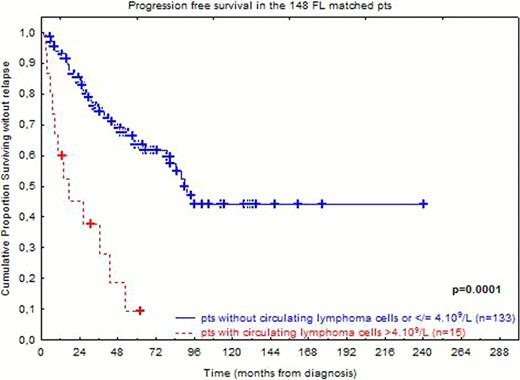
To further evaluate the impact of FL-LP on pts outcome, a 1:3 matched analysis was performed. The FL-LP 37 pts were successfully matched with 111 newly diagnosed FL without FL-LP according to FLIPI score, age, treatment type (abstention vs chemotherapy, with or without rituximab) and treatment period (before or after 2000). In these 111 matched pts, 5- and 10-y OS was 97% and 91%, respectively. Considering all 148 pts, high FLIPI score, presence of FL-LP, and β2-m>UNL were all significantly associated with a worse PFS. In a Cox regression model for PFS (120/148 pts with complete data), high FLIPI score (P=.0034; HR=2) and presence of FL-LP (P=.0085; HR=2.2) remained independently associated with shorter PFS. High FLIPI score and presence of FL-LP were also associated with a shorter OS. Interestingly pts with less than 4.109/L of circulating lymphoma cells had a similar PFS than those without. When circulating lymphoma cells >4.109/L as variable (see abstract figure) instead of FL-LP were tested in the Cox regression model for PFS including β2-m>UNL and FLIPI score as variables, the most significant predictor for a shorter PFS was circulating lymphoma cells >4.109/L (P=.0004; HR=3.56) as compared to FLIPI score (P=.051; HR=1.6) and β2-m (P=.09; HR=1.52).
The presence of circulating lymphoma cells in FL is a rare event and is associated with shorter PFS independently of FLIPI score and β2-m level. A validation of these findings on pts from the PRIMA study is on progress. However, this population is not homogenous and pts with circulating lymphoma cells >4.109/L have a poorer outcome. Although ∼1/3 of the pts experience long term PFS, these pts should be monitored carefully during and after first line treatment to consider HSCT as a therapeutic option to achieve a sustained response.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.