Abstract
Abstract 2035
We previously reported 23 MM patients, treated in first relapse by a sequential autologous-allogeneic tandem transplantation (aATT) approach. Data from this series compared favorably with a non allografted control population (Karlin, 2011). However, most of the patients were treated before the availability of novel anti-myeloma agents. We now report a larger series of 50 patients and conducted an overall survival (OS) comparison with a matched cohort.
From 2002 to 2011, fifty patients with MM were treated by a sequential autologous-allogeneic tandem approach in our institution. All were included in the study. A series of 64 non-allografted MM patients treated during the same period was used as a control group. An individual matching procedure was completed using the following factors: response to first line therapy, delay from first treatment to relapse, patient's age, year of relapse, ISS, serum Beta 2 microglobulin and albumin. OS comparisons were performed by using proportional hazards models stratified on each individual matched pair, or adjusted on strata to allow interaction test between cohort and stratum.
Median age of the allografted patients was 50.8 years (range 28.5 to 59.5 years). Forty-three (86%) were in first relapse, 7 (14%) in second relapse. First line treatment included a first high dose therapy with an autologous blood stem cell transplantation (aSCT) for all patients; 31 (62%) pts relapsed less than 2 years after this aSCT. At relapse, all patients received novel agents (IMID's and/or bortezomib). Overall response rate before aATT was 96%, including 8% complete response (CR), 42% of very good partial response (VGPR), and 46% of partial response (PR). First transplant of aATT was performed after high dose melphalan alone (n=28, 56%) or combined with bortezomib (n=22, 44%). For allotransplant, all patients received a reduced intensity conditioning regimen based on 2 Gy TBI with (n=14) or without (n=22) fludarabine). Acute GvHD prophylaxis used cyclosporine plus MMF. Donors were HLA-identical siblings in 29 patients (58%) while 21 (42%) had an unrelated-donor including 2 with one mismatch. The source of stem cells was peripheral blood in all patients. After allotransplant, complete donor chimerism was detected in all cases at day 100. The cumulative incidence function (CIf) of acute graft-versus-host disease (GvHD) grade II to IV was 27% at day 100 (95%CI 14 – 40) and 27 patients developed a chronic GvHD.
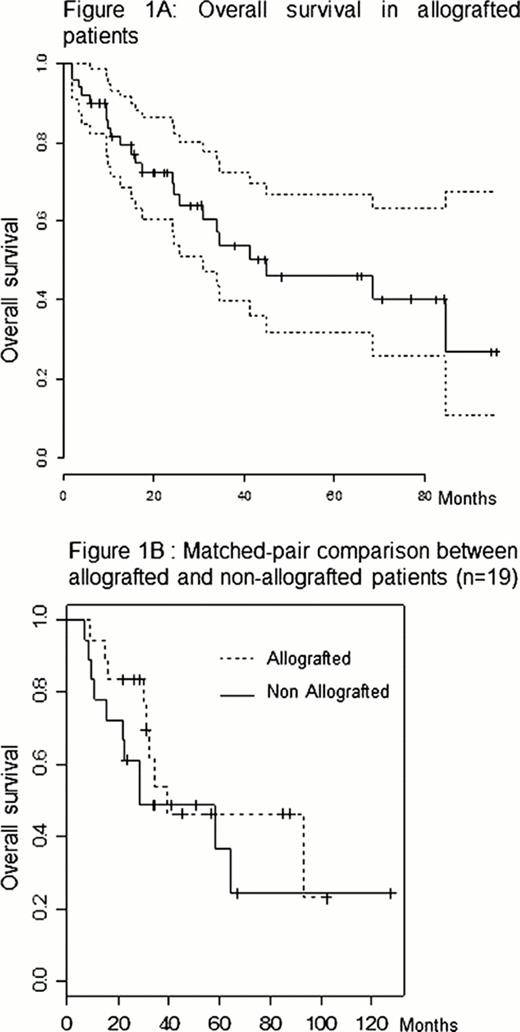
After a median follow-up of 24.3 months (IQR: 11.3–44.2), 23 patients died, including 12 free of relapse (Infections, n=7; GvHD, n=5) leading to a 1 year-CIf of TRM of 16.4% (5.8–27.0). Twenty four patients relapsed. Sixteen patients received a revlimid-based salvage therapy. Donor lymphocyte infusions were performed for 3 patients. The disease free survival (DFS) at 2-year was 61.2% (95%CI 47.0–75.4). The OS at 2 and 5 years was 72.3% and 46.1% respectively (Figure 1A). No factor allowed to predict neither TRM, relapse, DFS nor OS.
In the non-allograft group, within a median post relapse follow up of 1.8 years, post relapse 2 year OS was 47.8%. We identified 19 pairs of allograft and non-allograft pts eligible for a matched-pair comparison. All experienced their first relapse less than 2 year after initial high dose therapy with aSCT performed frontline. There was no significant difference between survival of allografted pts as compared to the control group (p = 0.35, HR = 0.68 [95% IC 0.3 – 1.55]) (Figure 1B).
In this single center study of 50 young MM patients treated in relapse by tandem autologous-allogeneic transplantation, we observed a relatively low TRM of 16.8%. In contrast to our first series, a matched-pair analysis suggested similar OS between allografted and non-allografted patients. These results questioned the role of non myeloablative allogeneic hematopoietic stem cell transplantation in the management of multiple myeloma in the era of novel anti-myeloma agents, but they should be confirmed. Incidence of relapse post aATT may justify a systematic post allo maintenance therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.