Abstract
Abstract 2722
Follicular lymphoma (FL) is the commonest type of indolent lymphomas and is considered as an incurable malignancy with a relapsing and remitting course. Most patients are diagnosed with FL when they have an advanced stage of disease, only less than 20% presenting with stage I or II. Initial management of early stage (Ann Arbor stage I or II) FL remains undefined. Numerous options exist but radiotherapy appeared to be the standard of care for early stage disease based on single institution or retrospective series. Our aim was to revisit the outcome of patients with localized FL in the era of rituximab.
We analyzed 145 patients treated in our institution with early stage (I or II) FL between January 01/1967 and 01/2011. Patients were retrospectively divided into six groups according to their initial treatment: watch and wait (WW), chemotherapy alone (CT), radiotherapy alone (RT), combination of radiotherapy and chemotherapy (RT-CT), Rituximab alone (Ri) and immuno-chemotherapy (Ri-CT).
Of the 145 patients (79 females and 66 males), 84 (57.9%) patients had stage I disease and 61 (42.1%) a stage II. Median age was 55 years (20% of patients > 65 years). Only 22 (15.2%) of them had a bulky disease (> 7cm). FLIPI score was 0–1 in 116 pts, 2 in 29 pts and none had a score >2.
The management of patients significantly varied over the different time (period I: <1990; period II: 1991–2000 and period III: 2001–2011) Use of RT decreased (43% for period I versus 24% for period III) whereas watchful waiting increased from 19.5% for period I up to 75% for the period III. Rituximab and Ri- CT use increased rapidly to 86% for the period III.
Patients characteristics were similar in terms of age between the 6 groups but differed in term of stage and prognostic factors, essentially more stage II (61%) and bulky disease (42%) in the Ri-CT group compared to the others.
The CR rate varied from 57% for the Ri group to 95% for the RT-CT group with 69% for CT, 75% for Ri-CT and 81% for RT alone. As expected, the proportion of PR was higher in the Ri group (43%). With a median follow-up of 7 years, the relapse rate was significantly lower in the Ri-CT group (40% versus 90.5% RT, 84% RT-CT, 69% CT and 58% WW respectively).
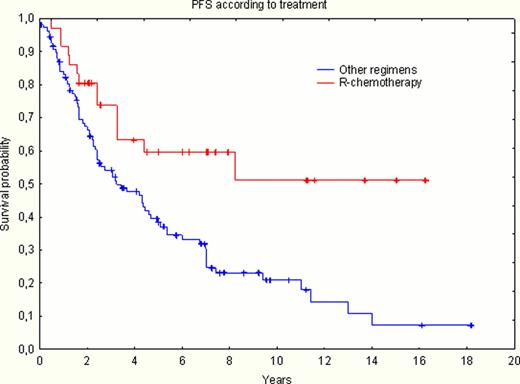
According to the modifications of management over time, OS and PFS are analyzed according to two period of time: < year 2000 and ≥ 2000. OS at 7.5 years for the patients managed after >2000 was better (75%) than for those managed <2000 (59%) (not statistically significant, p= 0.29). OS according to the different treatments did not show any difference: 72% WW, 74% CT, 74% Ri-CT, 67% RT-CT, 66% RT, and 100% for Ri, respectively. By contrast, a significant difference was found for PFS at 7.5 years in favor of the combination of Ri-CT (60%) versus the others (19% RT, 26% RT-CT, 23% CT and 26% for the WW strategy, respectively) (p= 0.00135) as described in Figure 1.
Within the inherent limits of this retrospective study, delayed start of therapy was associated with a similar OS than the one observed in patients receiving immediate intervention, and PFS was not different between WW versus RT or RT-CT. Thus, the “watch and wait” strategy could be proposed as first line therapy, like it is in stage III and IV follicular lymphoma patients with a low tumor burden. However, when a treatment is required, the combination of immunochemotherapy seems to be the best option.
Legends: R-CT: Ri CT or immunochemotherapy
Others regimens: WW, RT, RT+CT, CT
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.