Abstract
Abstract 3693
Histopathologically, some FLs have components of DLBCL at diagnosis. In the pre-rituximab era, there were two reports regarding the characteristics and prognosis of patients (pts) with these particular FLs1,2). Hans et al. reported that the overall survival (OS) of pts with FL grade 3 having a predominant (> 50%) DLBCL component is similar to that of pts with DLBCL1). Ghesquières et al. concluded that pts with DLBCL presenting with a low-grade component have a similar OS to those with de novo DLBCL2). However, the clinical implications and prognosis of FL pts with coexisting DLBCL at diagnosis undergoing rituximab-containing chemotherapy remain unclear.
We retrospectively analyzed the clinicopathologic features of 59 FL pts with coexisting DLBCL (FL/DLBCL) initially undergoing rituximab-containing chemotherapy. Furthermore, the prognosis of FL/DLBCL pts was compared with that of 223 FL pts without DLBCL as well as 285 DLBCL pts without FL3). All pts received a rituximab-containing regimen as the initial chemotherapy. These pts with FL/DLBCL or FL were diagnosed and treated at our institution between 2001 and 2010, and DLBCL pts between 2003 and 2010.
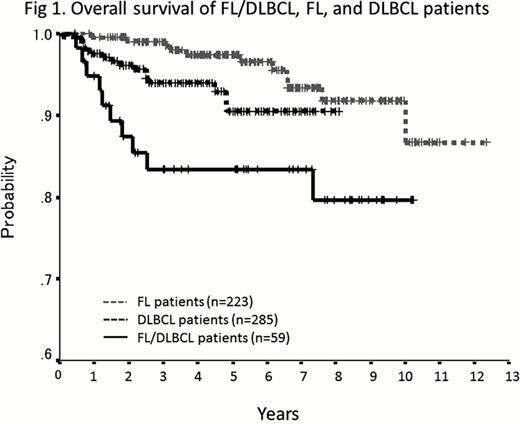
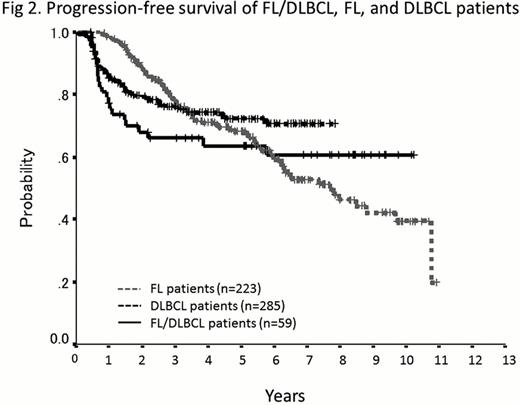
The median age of the 59 pts with FL/DLBCL was 54 years (range: 22–83). Among them, 41 (69%) pts had FL grade 1–3a and the remaining 18 (31%) had FL grade 3b components. Thirty (51%) pts had a predominant (> 50%) DLBCL component. With regard to treatment, all pts except one received the R-CHOP regimen. Forty-nine (83%) pts achieved CR, but 22 of them (37%) relapsed. With a median follow-up of 5.4 years, the estimated 5-year OS and progression-free survival (PFS) for all 59 pts were 83 and 64%, respectively. The International Prognostic Index (IPI) and FLIPI were not correlated with OS and PFS, whereas the revised-IPI (R-IPI) and FLIPI2 were significantly correlated with PFS. A predominant DLBCL component was predictive of neither OS nor PFS. In the 41 pts with FL grade 1–3a with DLBCL, %CR, 5-year OS, and PFS rates were 80, 84, and 60%, respectively. On the other hand, in the 18 pts with FL grade 3b with DLBCL, they were 89, 82, and 72%, respectively. The %CR and PFS rates of the latter cohort showed superior tendencies to those of the former cohort, with no statistically significant difference. Among 22 relapses, 10 were confirmed histologically: 5 DLBCL, 4 FL, and 1 HL. In 16 relapsed pts with FL grade 1–3a at initial diagnosis, 4 relapsed as FL, one each as DLBCL and HL. Two pts who had relapsed as FL and HL subsequently developed DLBCL. On the other hand, 4 out of 5 relapsed pts with FL grade 3b at the initial diagnosis relapsed as DLBCL. Additionally, the prognosis of FL/DLBCL pts was compared with that of FL and DLBCL pts. The 5-year OS rate of FL/DLBCL pts (83%) was significantly worse than that of DLBCL pts (91%, p=0.039) as well as FL pts (97%, p=0.001) (Fig 1). The 5-year PFS rate of FL/DLBCL pts (64%) was not significantly different from that of DLBCL pts (72%, p=0.120). The PFS curves (Fig 2) suggested a slight increase in progression or mortality in FL/DLBCL pts during the first 2 years. However, the FL/DLBCL pts had a low incidence of events after 2 years. The PFS curve of FL/DLBCL pts was similar to that of DLBCL pts. By multivariate analysis of pts with FL/DLBCL and DLBCL, coexisting FL components was a significant predictor of inferior OS, but not PFS.
The PFS curve of FL/DLBCL pts was similar to that of DLBCL pts, although pts with FL/DLBCL had poorer prognosis than DLBCL pts in the rituximab era. Furthermore, in our present analysis, predominant DLBCL component was predictive of neither OS nor PFS.
Kobayashi:Nippon Shinyaku: Research Funding; Ariad: Research Funding; Ohtsuka: Research Funding; Celgene: Research Funding; Behringer : Research Funding. Tobinai:Grant Support: Zenyaku, Chugai/Roche, GSK, Biomedics Other.
References:
Author notes
Asterisk with author names denotes non-ASH members.