Abstract
Abstract 4198
Chronic Graft-versus-Host-Disease (GvHD) remains a serious complication after allogeneic stem cell transplantation. In 2005 the National Institutes of Health (NIH) established new criteria for chronic GvHD based on retrospective data and expert recommendations.
Here we are reporting the prospectively evaluation of the incidence of NIH-defined chronic GvHD and its prognostic impact in 113 consecutive patients who underwent unmanipulated peripheral blood graft from an HLA-haploidentical relative after a treosulfan based conditioning at our Institution.
The peculiarity of this setting relies on the exploitation of a rapamycin-based, calcineurin-inhibitor-free regimen for prophylaxis of GvHD to induce in-vivo expansion of T-regulatory cells (Tregs).
Chronic GvHD was evaluable in 81 patients: 41 patients were diagnosed with chronic GvHD according to the revised Seattle criteria, 28 were classified as having extensive chronic GvHD and 13 were classified as having limited. The 1-year cumulative incidence was 43 +/− 9%.
According to the NIH Consensus Criteria, 1 patient was reclassified as having late-acute GvHD, 20 patients as having overlap syndrome and 20 patients as having classic chronic GvHD. The late-acute consisted of late onset subtype.
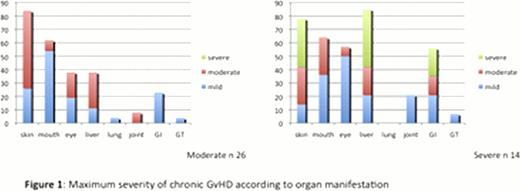
The 40 patients with classic chronic GvHD and overlap syndrome were graded as moderate (26 patients) and severe (14 patients) by NIH consensus criteria. The onset was classified as progressive in 4 cases, de novo in 27 cases, quiescent in 9 cases.
The median number of organs involved was 3 (range 1–7), the majority of patients presented with skin and oral involvement, but also eyes, liver, joint, genitalia and gastro-intestinal damages were present – maximum severity of chronic GvHD according to organ manifestation is presented in figure 1.
Twenty-seven out of 40 patients started a specific immunosuppressive treatment for chronic GvHD, noteworthy 21 patients restarted rapamycin (in combination with prednisone, or alone) with clinical benefit.
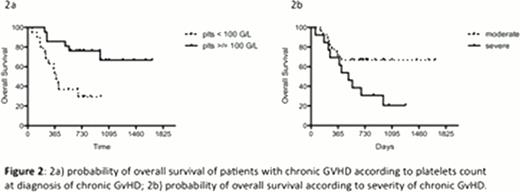
In univariable analysis patients with overlap GvHD tended to present a lower overall survival (OS) compared to those with classic chronic GvHD (36% versus 63%, p 0.07). Patients with severe chronic GvHD at onset had a significantly lower OS compared to those with moderate chronic GvHD (19% versus 69%, p0.017). OS was significantly worse for patients with platelets counts below 100 g/l at onset of chronic GvHD (29% vs 67%, p0.003)– figure 2.
This analysis confirms in haploidentical setting thrombocytopenia, overlap category and severe presentation as prognostic items for overall survival after allogeneic stem cell transplantation. Further investigations on implementation of immunosuppressive treatment strategy for high-risk GvHD patients (namely patients with overlap GvHD diagnosis and concomitant thrombocytopenia and/or progressive onset) are actually ongoing to enhance response and improve outcome.
Bordignon:MolMed SpA: Employment. Bonini:MolMed S.p.A.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.