Abstract
Abstract 4208
Despite preventive and therapeutic antiviral medication cytomegalovirus (CMV) infection is still a major cause of morbidity and mortality after allogeneic hematopoietic stem cell transplantation (SCT). Only limited data on CMV infection and disease are available in autologous SCT recipients. Previous studies have demonstrated that the probability of CMV infection is nearly 60% in seropositive patients and 23% in seronegative patients undergoing autologous SCT, but its impact in mortality is unclear.
We retrospectively reviewed the medical records of 101 patients undergoing autologous SCT at Hospital Israelita Albert Einstein from January, 2005 to July, 2012. CMV infection was defined as a quantitative real time PCR assay showing greater than 165 copies and/or positive CMV pp65 antigenemia assay. Lymphocyte count was registered at 15th day after SCT and lymphopenia was defined as an absolute lymphocytes count (ALC) < 500 at that time point. Overall survival (OS) was estimated from the time of transplant until death, with surviving patients censored at last follow-up. Variables entered into the multivariate Cox analysis were those with a p-value <0.10 in the univariate analysis. CMV infection was analyzed as a time-dependent covariate, considering the time to CMV infection. Statistical analysis was performed with STATA (v11.0) and alfa error was defined as 5%.
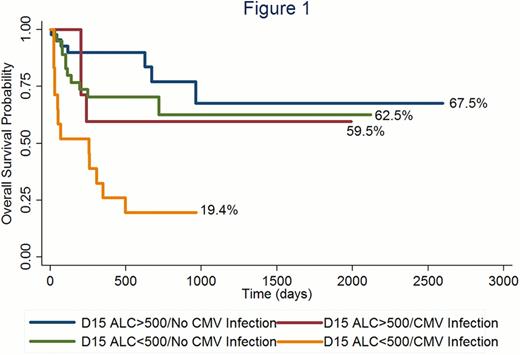
The majority of patients were male (62.4%) and the median age was 58 years old (range: 3–76). Peripheral stem cell harvest was the main source of cells (92%). A positive serological CMV status was found in 93.75% of patients. Most common indications for autologous SCT were multiple myeloma (34%), non-Hodgkin's lymphoma (40%) and Hodgkin's lymphoma (6%). After a median follow-up of 2 years, the OS for the whole cohort was 61% (95% confidence interval [CI] 48–72%). CMV infection post SCT was seen in 26% of patients. In the univariate analysis, development of CMV infection and presence of D15 lymphopenia were associated with a higher mortality (CMV infection-hazard ratio [HR] 3.32 [95%IC 1.61–6.84]; p= 0.001; D15 lymphopenia- HR 2.37 [95% IC 1.11–5.05]; p= 0.024). Patients who developed CMV infection in the setting of D15 lymphopenia had the worse outcome (2-years OS 19%; 95% CI 9–43%; figure 1). D15 lymphopenia was not associated with a higher rates of CMV infection (p=0.41). In Cox multivariate analysis, lower overall survival was demonstrated in female patients (HR= 2.23, 95%IC 1.08–4.58; p= 0.029), in the presence of D15 lymphopenia (HR= 2.56, 95%IC 1.19–5.51; p= 0.016) and CMV infection (HR: 3.33, 95% IC1.61–46.86; p= 0.001).
CMV infection post-autologous SCT is associated with a decreased survival, and in the concomitant presence of D15 lymphopenia appears to indicate a subgroup of patients with very poor outcome. It is possible that CMV infection does not lead directly to increased mortality, but is rather a surrogate marker of decreased immune function post-ASCT. Future studies should prospectively evaluate the incidence and prognostic impact of CMV infection post-ASCT and correlate with markers of immune recovery.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.