Abstract
Abstract 4540
The impact of HLA DRB3 and DRB4 allele mismatch after allogeneic HSCT using unrelated donors is unclear. We therefore examined retrospectively the outcome of 35 patients who received HLA-10/10 unrelated hematopoietic stem cell transplantation with a DRB3 or DRB4 mismatch between 2005 and 2011. This cohort of 35 patients was a part of a cohort of 132 consecutive patients who underwent allogeneic HSCT between 2005–2011 with a 10/10-HLA matched donor.
There were 18 males (51.4%) and 17 females (48.6%) with a median age of 48 years (range, 6–64), there were 13 (37%) AML, 9 (26%) ALL, 4 (11.5%) MDS, 3 (8.5%) multiple myeloma and 6 (5.7%) other (CML, CLL, NHL). Twenty patients (57%) received a myeloablative conditioning (MAC) and 15 (43%) received a reduced intensity conditioning (RIC). At transplantation, 21 patients (60%) were in complete remission (CR), 4 patients (11.5%) in partial remission (PR) and 10 (28.5%) in relapse; 13 (37%) patients received peripheral blood stem cell (PBSC) and 22 (63%) received bone marrow (BM). Twelve (34%) patients had a mismatched DRB4 donor and 23 (66%) patients had a mismatched DRB3 donor.
In the remains of 97 patients, there were 55 male (57%) and 42 female (43%), 28 (29%) patients received a MAC and 69 (71%) a RIC as regimen before allogeneic HSCT. The stem cell source was BM for 32 (34%) patients and PBSC for 65 (66%). At transplantation, 34 (35%) patients are in CR and 63 (65%) were in PR. The distribution of diagnosis was acute leukaemia and MDS for 44 (45%), CLL for 2 (2.5%) and other diagnosis (aplastic anemia, NHL, CML, MPS) for 51 patients (52.5%).
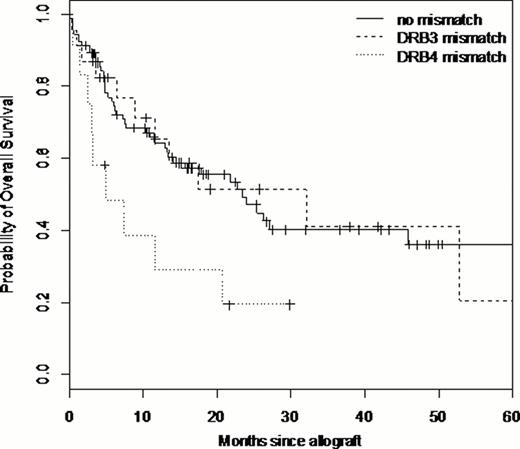
After HSCT, 124 (94%) patients engrafted. After a median follow-up of 11.5 months (range, 0–76), the cumulative incidence of acute GvHD≥2 at 3 months was 20% (95%CI,16.5–24) and the cumulative incidence of chronic GvHD at one year was 19 % (95%CI, 15–22). In univariate analysis, the mismatch DRB3 or DRB4 had no effect on engraftment and no effect on acute GvHD (p=0.08) or chronic GvHD (p=0.63). There was no impact of DRB3 or DRB4 mismatch on relapse (p=0.33 and p=0.53, respectively) and on PFS (p=0.63 and p=0.07, respectively). We found an impact of the DRB4 mismatching (p=0.016) on overall survival. The median survival for patient without DRB3 or DRB4 mismatch was 23 months (14-NR), for patients with DRB3 mismatch 32 months (12-NR), and for DRB4 mismatched patients 5 months (3-NR). The probability of survival at 24 months, for patients without mismatch DRB3 or DRB4 is 47% (36–61), for patients with DRB3 mismatch 51% (32–82) and for DRB4 mismatched patients 19% (6–66%). (figure1).
The multivariate analysis that studied age, type of disease, DRB3 or DRB4 mismatch, sexmatching, TBI, ATG, disease status at transplantation and type of conditioning and stem cell source showed a significant impact of mismatch DRB4 on survival (HR= 2.5 [95%CI, 1.2–5.5] p=0.019); there was no impact for DRB3 mismatch (HR= 1.3 (95%CI,0.5–3.9 p=0.58). We found also an impact of the DRB4 mismatch on TRM (HR= 3.5; [95%CI, 1.6 –8] p= 0.026). The incidence of TRM at 24 months for patients without DRB3 or DRB4 mismatch is 29% (24–34), for patients with DRB3 mismatch 17% (9–26%) and for DRB4 mismatched patients 50% (34–66%). (figure 2).
The HLA DRB4 matching donor is relevant for survival of patients who undergo allo-HSCT from unrelated donor in the HLA-10/10 matching settings. In view of the important impact of these loci mismatches on clinical outcome, it seems to be important to consider this matching loci in the unrelated donor selection.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.