Abstract
Abstract 4931
Autoimmunity, evidenced by positive serology or autoimmune diseases, has been noted to co-exist in pts with MDS. Autoimmune dysfunction has been found in some pts with a variant of MDS called hypocellular MDS, where immune suppressant medications have role in treatment. Clinical implications of AI on survival are not well described.
To study clinical influence of autoimmunity on pts with LR-MDS.
All adult pts diagnosed with LR (RCUD, RARS, and RCMD) MDS at the Mayo Clinic between 1996 to 2000 were studied. Retrospective data collection included pts' demographics, laboratory tests, bone marrow biopsies, treatment modalities and survival information. Autoimmunity (AI) was considered present if pts had evidence of positive serological testing (such as rheumatoid factor (RF), anti-nuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA)) and/or were diagnosed with autoimmune diseases (such as rheumatoid arthritis, vasculitis, autoimmune hemolytic anemia (AIHA), immune thrombocytopenia (ITP)). IRB approval was obtained in accordance with Helsinki Declaration. Chi-Square, t-test and Anova were used for comparatives between groups, and Kaplan-Meier test was applied for survival estimates using JMP 9. 0 software.
A total of 134 adult pts were found to have LR-MDS at the time of their diagnosis. Sixty-six percent (89) were males, 13% (17) had antecedent hematological disease (AHD), and only 7% (9) had prior radio- or chemotherapy. Thirty-nine (29%) had evidence of AI. At the time of diagnosis, pts' median Hgb was 9. 3 g/dL, white blood cells (WBC) 4. 1×109/L, and platelets 151×109/L. On comparison, there was no difference between pts with AI (group 1) to the rest of the sample (group 2) (p = 0. 12, 0. 85 and 0. 23, respectively). Bone marrow cytogenetics were abnormal in 42% (56) pts, with 44 pts have one cytological anomaly, and only 2 have four anomalies. Twenty-four pts (18%) had RCUD, 60 (44%) RARS and 50 (37%) RCMD, as defined by World Health Organization (WHO) classification (Vardiman et al, 2008). Karyotype anomalies within the three WHO classes were found in 12/19 pts (63%), 15/52 pts (29%), and in 29/42 pts (70%), respectively. Of note, among those with karyotype anomalies, the mean number of cytogenetic abnormalities was significantly different across the three categories (F=6. 89, p=. 0014), with means of 0. 5, 0. 3, and 0. 9 respectively. Seven pts (5%) progressed into acute myeloid leukemia. Seventy percent of pts (94) remained as stable disease.
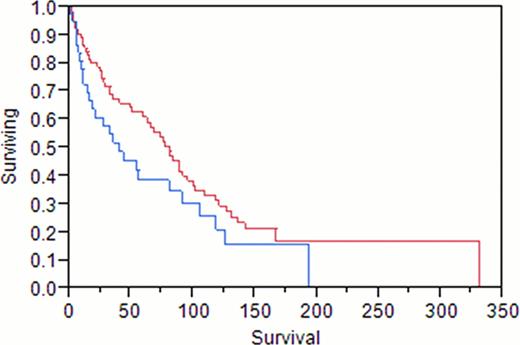
Of the 134 pts studied, 39 (29%) were found to have evidence of AI, with 24/48 (50%) had abnormal serological tests, and 29/134 (21%) had an autoimmune disease. When tested, positive RF was found in 7/25 (28%), ANA in 14/42 (33%), anti dsDNA in 1/11 (9%), anti SS-A/-B in 2/3 (66%), ANCA in 1/12 (8%), anti-smooth muscle in 1/2 (50%), and anti-histone in 1 pt. As per autoimmune diseases, rheumatoid arthritis was identified in 6 pts (4%), vasculitides in 9 (7%), AIHA in 4 pts (3%), Sjögren syndrome in 3 (2%), myositis in 2 (1. 4%), ITP in 2 pts (1. 4%). There was no difference in AI frequency based on WHO classification (p 0. 17) or based on cytogenetic grouping (p 0. 37). Overall survival in pts with LR-MDS was found to be lower in group 1 as compared to group 2 but did not reach statistical significance (p=0. 109), with median survival of 40 months and 81 months, respectively.
AI is a frequent finding in pts with LR-MDS, seen in up to 29% of pts. On comparison there was no difference in hematological parameters of both groups with or without AI (CBC, cytogenetics, and WHO classification). There was no survival difference in LR-MDS pts with AI compared to pts without AI. Larger size studies are needed to confirm our findings.
Blue color AI+, red color AI -
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.