Abstract
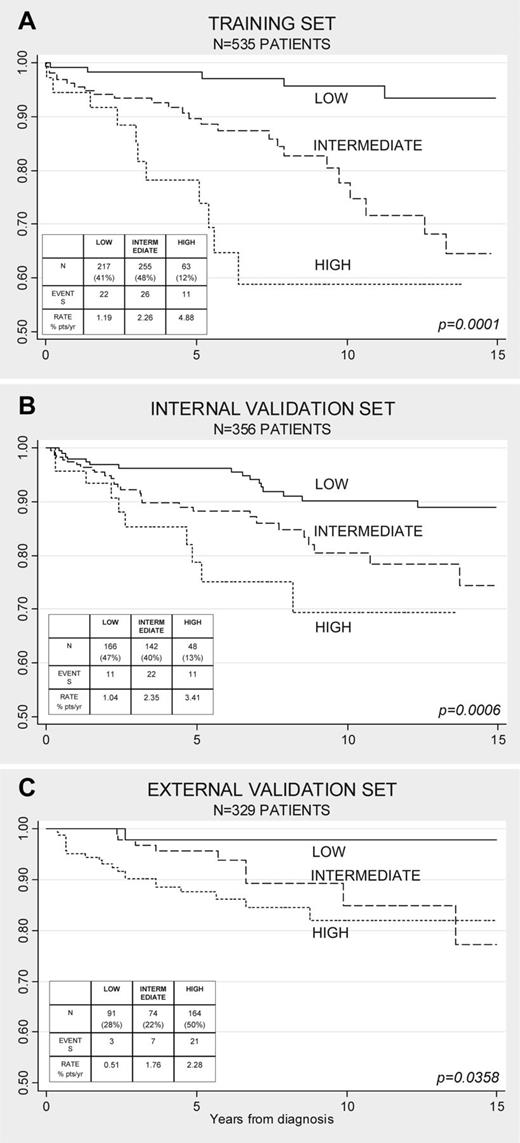
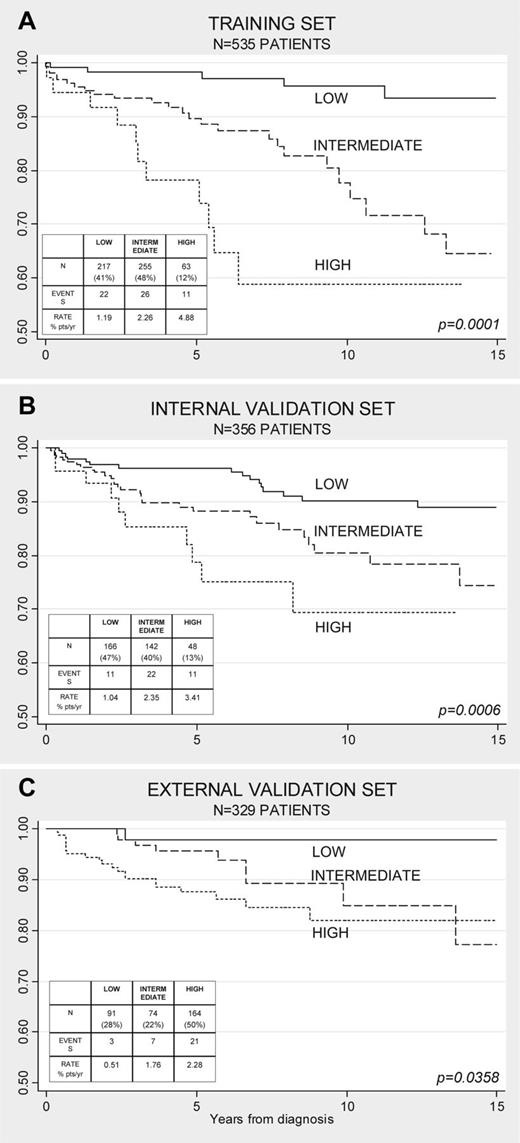
Accurate prediction of thrombosis in essential thrombocythemia (ET) provides the platform for prospective studies exploring preventive measures. Current risk stratification for thrombosis in ET is 2-tiered and considers low- and high-risk categories based on the respective absence or presence of either age > 60 years or history of thrombosis. In an international study of 891 patients with World Health Organization (WHO)–defined ET, we identified additional independent risk factors including cardiovascular risk factors and JAK2V617F. Accordingly, we assigned risk scores based on multivariable analysis–derived hazard ratios (HRs) to age > 60 years (HR = 1.5; 1 point), thrombosis history (HR = 1.9; 2 points), cardiovascular risk factors (HR = 1.6; 1 point), and JAK2V617F (HR = 2.0; 2 points) and subsequently devised a 3-tiered prognostic model (low-risk = < 2 points; intermediate-risk = 2 points; and high-risk = > 2 points) using a training set of 535 patients and validated the results in the remaining cohort (n = 356; internal validation set) and in an external validation set (n = 329). Considering all 3 cohorts (n = 1220), the 3-tiered new prognostic model (low-risk n = 474 vs intermediate-risk n = 471 vs high-risk n = 275), with a respective thrombosis risk of 1.03% of patients/y versus 2.35% of patients/y versus 3.56% of patients/y, outperformed the 2-tiered (low-risk 0.95% of patients/y vs high-risk 2.86% of patients/y) conventional risk stratification in predicting future vascular events.
Medscape EDUCATION Continuing Medical Education online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and the American Society of Hematology. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participationin the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 5252.
Disclosures
The authors, the Associate Editor Martin S. Tallman, and CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, declare no competing financial interests.
Learning objectives
Upon completion of this activity, participants will be able to:
Describe independent risk factors for thrombosis in essential thrombocythemia (ET), based on an international study of 891 patients with World Health Organization (WHO)–defined ET.
Describe a new 3-tiered prognostic model for thrombosis in ET, based on these independent risk factors.
Compare the performance of the new 3-tiered prognostic model with that of the current 2-tiered risk stratification.
Release date: December 20, 2012; Expiration date: December 20, 2013
Introduction
Essential thrombocythemia (ET) is the most common among the myeloproliferative neoplasms (MPNs), with an annual incidence estimated at 1.5-2 per 100 000 persons. The median age at presentation is 55-60 years.1 In 2005, JAK2V617F, an activating JAK2 mutation, was first reported in patients with MPN, including approximately 60% of those with ET.2-5 The natural history of ET is characterized by an increased incidence of vascular complications and an inherent tendency to progress into myelofibrosis or acute myeloid leukemia.1-6
Multiple factors are believed to contribute to the pathogenesis of thrombosis in ET, some of which are host related and others disease related. Advanced age and history of thrombosis are the 2 major risk factors for thrombosis in ET and define low-risk (no risk factors) and high-risk (presence of one or both risk factors) patient categories.6 Based on such risk stratification, the potential dangers of cytoreductive therapy with the intent of preventing thrombotic complications may be justified in high-risk patients.6,7
Recent studies have raised the possibility of additional thrombotic risk factors in ET. These factors include cardiovascular risk factors (eg, diabetes, hypertension, and smoking),1 leukocytosis,8-11 and the presence of JAK2V617F and its allele burden.12-15 However, the issue had been confounded by the lack of a broad-based multicenter study with large sample size and diagnostic accuracy. Previous prognostic studies had relied on the Polycythemia Vera Study Group (PVSG) criteria for diagnosis and did not distinguish true ET from prefibrotic myelofibrosis, as has since been established by the World Health Organization (WHO) diagnostic criteria for MPN.16,17 Furthermore, current risk factors for thrombosis are based on relative risk estimates such as odds ratio, risk ratio, or hazard ratio (HR), so that no direct meaning or relevance to prognostication of thrombosis in individual patient can be drawn from a single risk factor assessment. A more reliable risk prediction may be provided by combining multiple variables in prognostic models for which performance needs to be confirmed in other cohorts of patients.18 Accordingly, the aim of the present study was to construct an accurate prediction model for thrombosis from multiple variables predicting thrombosis in an inception multicenter cohort of 891 strictly WHO-defined ET patients and to validate its performance in new cohorts of patients.
Methods
Patients
Clinicians and pathologists from 7 international centers of excellence for MPNs convened to create a clinicopathologic database of 1104 patients previously diagnosed and treated as having ET.17 The study was approved by the institutional review board of each institution and was conducted in accordance with the Declaration of Helsinki.
Study eligibility criteria included availability of treatment-naive BM specimens obtained within 1 year of diagnosis. All BM samples subsequently underwent a central re-review by 1 of the authors (J.T.) of the WHO chapters on diagnostic criteria for ET, polycythemia vera, and primary myelofibrosis.16 The central histology review by J.T. was completely blinded to outcome data, which were analyzed after the completion of the histopathology review. Diagnosis was confirmed as ET in 891 patients (81%) and was revised to early/prefibrotic primary myelofibrosis in 180 patients (16%); 33 patients were not evaluable. The present study focuses on the 891 patients with WHO-defined ET, which included 438 (49%) patients with conventionally assigned low-risk disease (ie, age < 60 years and no history of thrombosis).
For the purposes of this study, we considered only major vasoocclusive events, including ischemic stroke, cerebral transient ischemic attacks, acute myocardial infarction, peripheral arterial thrombosis, and venous thromboembolism.
Prognostic factors
The Cox proportional hazard regression model was used for multivariable analysis, adjusting for sex, age ≥ 60 years, previous thrombotic event, laboratory parameters measured at diagnosis (ie, hemoglobin, platelet count, and WBC count), JAK2V617F mutational status, cardiovascular risk factors (ie, hypertension, diabetes, and active tobacco use), and the need for cytoreductive therapy (including hydroxyurea in 90% of patients and busulfan and anagrelide in the rest) and antiplatelet drugs during follow-up.
Prognostic model
An integer weight close to the corresponding HR resulting from the analysis was assigned to each of the factors found to be associated with thrombosis. The entire cohort of 891 patients was then randomized in 2 distinct datasets equally stratified for the belonging center of each patient. The training set included 60% of the cohort and was used to test the prognostic model. The Kaplan-Meier product-limit method was used to estimate univariate thrombosis-free survival curves, and the log-rank test was adopted to compare survival curves. The internal validation set, including the remaining 40%, was used to validate the model. External validation was assessed at another site (Policlinico Gemelli, Rome, Italy) using a retrospective cohort set of 329 patients with WHO-ET diagnosis histologically confirmed by the local hematologist and pathologist.
Discrimination power of the model
The discrimination power of the International Prognostic Score for Essential Thrombocytopenia (IPSET) model was compared with that of conventional risk factors by the Harrell C-concordance index: a C-index of 0.50 indicates a model that does not discriminate better than chance alone and a C-index of 1.00 indicates perfect discrimination.19
Results
Development of the prognostic model
The main clinical and laboratory features of the 891 patients with strictly WHO-defined ET at diagnosis are presented in Table 1. Cytoreductive therapy was usually not given in low-risk patients at diagnosis. Some patients (37%) needed cytoreduction during follow-up because they met the criteria for being high risk. In contrast, the great majority (76%) of high-risk patients at diagnosis were treated with cytoreductive therapy. Low-dose aspirin therapy was documented in 602 (68%) patients. After a median follow-up of 6.2 years, 109 (12%) patients experienced major arterial (n = 79) or venous (n = 37) thrombotic complications. The annual rate of fatal and nonfatal events was 1.9% of patients. The incidence of nonfatal arterial events (1.2% of patients/y) was higher than that of venous thrombosis (0.6% of patients/y).
In multivariable Cox regression analysis, predictors of total major thrombotic events included age more than 60 years, thrombosis history, cardiovascular risk factors (including tobacco use, hypertension, or diabetes mellitus), and presence of JAK2V617F. Leukocyte and platelet counts were not found to be independently predictive.20 On the basis of the HR and assigned score values, patients were divided into the low-risk (sum of score = 0-1), intermediate-risk (score = 2), and high-risk (sum of score ≥ 3) categories (Table 2).
By Kaplan-Meier analysis of the training cohort of 535 patients, a significantly different thrombosis-free survival (P = .0001) was documented in the 3 groups (Figure 1A). Low-risk patients (41%) had a thrombosis-free survival of 87% after 15 years of follow-up. In contrast, the high-risk group (12%) had a probability of thrombosis-free survival of 50% starting after 7 years from diagnosis. The intermediate-risk patients (48%) showed a probability of events close to the low-risk category for the first 10 years and then progressively reached the high-risk curve in the subsequent 5 years.
Thrombosis-free survival curves. Shown are survival curves according to the International Prognostic Score for Essential Thrombocytopenia (IPSET) thrombosis model in the training set (A), internal validation set (B) and external validation set (C).
Thrombosis-free survival curves. Shown are survival curves according to the International Prognostic Score for Essential Thrombocytopenia (IPSET) thrombosis model in the training set (A), internal validation set (B) and external validation set (C).
Validation of the model
The predictive accuracy of the training set was assessed on the second portion of the cohort (internal validation set; Table 1) and in an external inception cohort of WHO-ET cases with comparable hematologic and clinical characteristics and including all the significant variables. (Table 3). A statistically significant performance by log-rank test was achieved in both cases (P = .0006 and P = .0358, respectively; Figure 1B-C).
Comparison with the standard model and discrimination power
The risk classification of all 1220 ET patients included in the 3 cohorts according to IPSET-thrombosis model or standard risk factors was compared (Table 4). A total of 48% of patients considered to be low risk by the standard model (younger and asymptomatic) were confirmed as low risk by the new model, whereas 47% and 5% of these patients were reclassified as intermediate or high risk, respectively. Regarding the previously defined high-risk patients, there was redistribution in 3 groups including approximately 30% of cases each. The annual rate of events in each subgroup is shown in the Table 4. By C-statistical analysis, the IPSET-thrombosis model better predicted future vascular events than conventional risk factors. The discrimination power of the model applied to 65% of patients, whereas the conventional factors applied to 60%.
Discussion
The present study presents a new prognostic model for thrombosis in ET, IPSET-thrombosis, that was developed to improve risk classification to optimize clinical decision making in individual patients. This model has several potential advantages over the previous conventional system, which was based on age and previous thrombosis and had limitations.
The first advantage of IPSET-thrombosis is that it has been developed according to the currently accepted formal rules for producing prognostic scores.18 The model includes a representative sample of patients at diagnosis with a long follow-up period and is sufficiently powered in terms of sample size and number of events to reduce the effect of chance. Candidate predictors have been selected from multivariate analysis of patients with strictly defined WHO-ET diagnosis who are known to have distinct clinical presentations and outcomes compared with those with early, prefibrotic myelofibrosis presenting with thrombocythemia.17-20 Therefore, IPSET-thrombosis can be applied more properly to currently diagnosed ET patients16 than can the conventional system developed before 2008 in the PVSG diagnostic era.21 IPSET-thrombosis was developed by combining single predictors in the first randomly split portion of our 891-patient cohort (the training set included 535 patients), and was clinically validated on the second portion (internal validation) and in an external cohort of WHO-ET patients with comparable sample size, patient presentation, and follow-up period. Therefore, reproducibility was confirmed in patients who were not included in the development model and generalizability was confirmed in an external single center retrospective cohort in which no important predictors were missing and treatments were comparable. The lower performance of the model in these patients (P = .03 vs P = .0001 in the training set) may reflect differences of case-mix (heterogeneity made by different populations considered) and different prevention policy of these events, as suggested by the higher use of aspirin and cytoreductive therapy in the external validation cohort.
A second advantage to our study is that IPSET-thrombosis includes novel risk factors for thrombosis in ET, such as the JAK2V617F mutation, which has been consistently reported in various studies,12-14 but not yet incorporated in a prognostic system. In our model, the relative risk of vascular complication associated with the mutation was double, in agreement with published meta-analysis.15 Because it is unpractical to propose different scoring systems for arterial and venous thrombosis, leukocytosis shown as an independent risk factor for only arterial events20 was not included in the present study because our model considers total thrombosis. In this context, leukocytosis was found to be more frequent and predictive of total thrombotic complications in patients with early prefibrotic myelofibrosis and not in those with WHO-ET.22
The third advantage is that IPSET-thrombosis defines an “intermediate-risk” group of patients who were not previously clearly identified. The existence of this “intermediate” category has been previously advocated, but never consistently demonstrated. We previously1,23 considered otherwise low-risk (ie, young and asymptomatic) ET patients with associated general risk factors for thrombosis (eg, smoking, hypertension, or diabetes) at intermediate risk for vascular complications. British investigators defined “intermediate-risk” as asymptomatic patients without hypertension or diabetes who were 40-59 years of age with platelet counts below 1500 × 109/L.24 Given these uncertainties, the European Leukemia Net (ELN) expert consensus conference decided not to include the intermediate-risk category for thrombosis in their recently published guidelines.6 Our score system now provides a clear definition of this group of patients and gives a well-defined weight to the so-called general cardiovascular risk factors for thrombosis. Overall, the present IPSET-thrombosis risk classification score significantly modifies the conventional system.6 Only 48% of the previously defined “low-risk” patients (young and asymptomatic) are considered to be low risk with the new classification; the other 52% are included in the intermediate-risk category (eg, young, asymptomatic patients carrying the JAK2V617 mutation) or in a small fraction (5%) of high-risk (eg, young, asymptomatic carrying JAK2V617F mutation and cardiovascular risk factors). Moreover, the majority of patients judged at high risk according to the conventional risk factors (eg, symptomatic or age more than 60 years) are now re-classified at intermediate (31%) or even at low (31%) thrombotic risk (eg, age > 60 years but no previous thrombosis, no cardiovascular risk factors, and no JAK2V617 mutation). Compared with the currently used risk classification that defines low risk (younger than 60 years or no previous thrombosis) and high risk when only one of these predictors is present,6 the IPSET-thrombosis system has shown a better discriminating power as measured by the Harrell C-concordance index. Given 2 ET patients, the chance that 1 will develop thrombosis and the other will not was predicted in 65% of patients by applying the IPSET-thrombosis model; that number was only 60% with the conventional system. Interestingly, we calculated the C-concordance index for age or previous thrombotic events, which was 0.51 and 0.60, respectively, indicating the poor discrimination power of age alone.
A potential limitation of our study is its retrospective design, which may generate the concern that antithrombotic treatments and cytoreductive therapy can affect prognosis, leading to an underestimate of the observed differences between the 3 groups. We are aware that only prognostic studies from prospective randomized trials may disentangle the effects of the prognostic factors from the effect of treatment; however, these latter studies may have restricted generalizability because of strict eligibility criteria required by the trials.18
Changing the risk classification may have therapeutic implications. As outlined by recent recommendations, current treatment in ET is shaped according to thrombotic risk.6,25 We are aware that treatment guidelines should be established by prospective studies and/or consensus of experts. Therefore, our findings are most useful in providing the tools to risk-stratify future study patients and not necessarily to dictate current therapy. An approach we suggest on the basis of our results is to recommend the cytoreductive therapy in the presence of thrombosis history at any age or a combination of advanced age with either cardiovascular risk factors or JAK2V617F-positive mutational status. Older patients who are JAK2V617F negative may not need cytoreductive therapy in the absence of cardiovascular risk factors. We recommend aspirin use in younger patients with no thrombosis history in the presence of either cardiovascular risk factors or JAK2V617F-positive mutational status, because the expected rate of major bleeding (1% of patients/y)26,27 is lower than the expected benefit.28
In conclusion, our validated IPSET-thrombosis model provides objective estimates of the probability of thrombotic events in patients with newly diagnosed ET that can be useful for future prospective clinical studies.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
A.M.V. and A.R. were supported by a grant from the Associazione Italiana per la Ricerca sul Cancro (Milan, Italy) Special Program Molecular Clinical Oncology 5 × 1000 to the Italian Association for Cancer Research (Associazione Italiana per la Ricerca sul Cancro) Gruppo Italiano Malattie Mieloproliferative (project number 1005). A detailed description of the project is available at http://www.progettoagimm.it.
Authorship
Contribution: T.B., G.F., A.C., J.T., and A.T. and designed the research, contributed patients, participated in the data analysis and interpretation, and wrote the manuscript; J.T. reviewed all BM histopathology; the remaining authors either contributed patients or participated in reviewing BM histopathology; and all authors read and approved the final draft of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Tiziano Barbui, Ospedali Riuniti di Bergamo, Largo Barozzi 1, Bergamo 24128, Italy; e-mail: tbarbui@ospedaliriuniti.bergamo.it.
References
Author notes
T.B., G.F., A.C., J.T., F.P., and A.T. contributed equally to this work.