Abstract
Extracellular protein disulfide isomerase (PDI) is required for platelet thrombus formation and fibrin generation after arteriolar wall injury in live mice. PDI is secreted from platelets and endothelial cells on cellular activation, but the mechanism of capture of secreted PDI within the injured vasculature is unknown. We establish that, like the endothelial β3 integrin αVβ3, the platelet integrin αIIbβ3 binds PDI. PDI also binds to recombinant β3. Using intravital microscopy, we demonstrate that PDI accumulation at the site of laser-induced arteriolar wall injury is markedly reduced in β3-null (β3−/−) mice, and neither a platelet thrombus nor fibrin is generated at the vessel injury site. The absence of fibrin after vascular injury in β3−/− mice is because of the absence of extracellular PDI. To evaluate the relative importance of endothelial αVβ3 versus platelet αIIbβ3 or αVβ3, we performed reciprocal bone marrow transplants on wild-type and β3−/− mice. PDI accumulation and platelet thrombus formation were markedly decreased after vessel injury in wild-type mice transplanted with β3−/− bone marrow or in β3−/− mice transplanted with wild-type bone marrow. These results indicate that both endothelial and platelet β3 integrins contribute to extracellular PDI binding at the vascular injury site.
Introduction
Protein disulfide isomerase (PDI), a prototypic thiol isomerase, catalyzes formation and isomerization of protein disulfide bonds.1 Despite the presence of an endoplasmic reticulum retention sequence,2 PDI is detected outside the cell after platelet and endothelium activation and secretion.3-6 We have shown that extracellular PDI accumulates on the injured luminal aspect of the arteriolar wall in a live mouse and is required for both fibrin formation and platelet thrombus formation.7 In vivo studies indicate the early appearance of endothelial cell–derived PDI, which is rapidly followed by platelet PDI during thrombus formation.6,7 Despite high shear rates in the arteriolar circulation, secreted PDI remains associated with the injured vessel wall and the developing thrombus.
The molecular basis for the role of PDI in thrombus formation remains unclear. In vivo studies have shown that PDI participates in both fibrin generation and platelet thrombus formation, regardless of whether experimental injury is induced via laser injury, ferric chloride treatment, Rose bengal oxidation, or mechanical disruption and regardless of the vascular bed: cremaster, mesentery, or carotid.6-8 Although its mechanism of action is unknown, PDI is required for tissue factor expression.7 Human umbilical vein endothelial cells in culture, when laser-activated while bathed in plasma, generate extracellular fibrin.9 The appearance of fibrin is inhibited by blocking antibodies to PDI and by blocking antibodies to tissue factor.6,9 PDI also plays an important role in platelet aggregation and is thought to exert its effect on the integrin αIIbβ3.10 Several studies have demonstrated that specific disulfide bonds in the EGF domains and the β-tail domain of β3 are critical for the activation of αIIbβ3.11-13 The cleavage of these bonds might be mediated by PDI.10
Integrins are heterodimeric transmembrane receptors consisting of noncovalently linked α- and β-subunits.14 These receptors regulate cell-cell and cell-matrix protein interactions. The β3 subunit, 1 of 8 mammalian β-subunits, is associated with αIIb and αV subunits. Although αIIbβ3 integrin is exclusively expressed on megakaryocytes and platelets, αVβ3 integrin is widely expressed on various cell types, including platelets and endothelial cells.15 The physical interaction between the β3 integrin and PDI remains controversial.16,17 Interaction of PDI with αVβ3 integrin on the surface of endothelial cells results in conversion of the integrin to the active state.16 In contrast, platelet β3 integrins were reported not to be physically associated with PDI during platelet activation.17
To investigate whether β3 integrins play a role in PDI binding during thrombus formation, we examined PDI accumulation in mice lacking β3 in either the platelet or endothelial cell compartment or both. The β3 integrin, in the form of αIIbβ3, is abundant on platelets18,19 ; αVβ3 contributes a smaller component of the β3 integrin on the platelet surface.15,20,21 Endothelial cells express αVβ3 but not αIIbβ3.21,22 In our studies, PDI accumulation and fibrin generation were greatly reduced or eliminated in β3−/− mice after vessel wall injury. Analysis of thrombus formation in chimeric mice generated by reciprocal bone marrow transplantation between wild-type (WT) and β3−/− mice revealed that both endothelial and platelet β3 integrins contributed to extracellular PDI interaction and accumulation.
Methods
Antibodies and reagents
Rat monoclonal anti–mouse P-selectin antibody conjugated to phycoerythrin and rat anti–mouse GPIbβ antibody conjugated to DyLight 649 were from Emfret. Human thrombin, ADP, neomycin, and rabbit polyclonal anti–bovine PDI antibody were purchased from Sigma-Aldrich. Recombinant human PDI was obtained from Prospec Bio. Alternatively, recombinant PDI was expressed in Escherichia coli, then purified by sequential chromatography with an Ni-NTA column and Superdex 200 column via fast protein liquid chromatography. Platelet-derived full-length αIIbβ3 was obtained from Abcam. Recombinant β3 was expressed in Drosophila S2 cells and purified to homogeneity by sequential chromatography with an Ni-NTA column and Superdex 200 column via fast protein liquid chromatography. A rabbit anti-PDI antibody, DL11, against a peptide was provided by Sigma-Aldrich free of albumin. Another rabbit anti-PDI antibody cross-reacted with human and mouse PDI and was immunopurified with bovine PDI covalently linked to CNBr-activated Sepharose, as described previously.7 A mouse monoclonal antifibrin-specific antibody was derived from hybridoma cell line 59D8.23 Immunoaffinity-purified rabbit anti-PDI antibody, mouse antifibrin antibody, and nonimmune control IgGs were labeled with Alexa 488 or Alexa 647 according to the manufacturer's instructions (Invitrogen). The molar ratio of Alexa to protein was varied from 2.5 to 3.0, as determined spectrophotometrically. Cephalin was purchased from Diagnostica Stago. A23187 and PPACK (d-Phe-Pro-Arg-chloromethylketone) were from EMD Chemicals.
Cells
Chinese hamster ovary (CHO) cells expressing P-selectin were generated as described previously,24 whereas those expressing αIIbβ3 and αVβ3 were a generous gift from Drs H. Kato and S. Shattil (University of California, San Diego). These cells were grown in DMEM containing 200mM glutamine, 10% FBS, 1% nonessential amino acids, and 1% penicillin/streptomycin solution at 37°C in a 5% CO2 incubator.
Flow cytometry
For analysis of the interaction of PDI with cell surface proteins, CHO cells expressing αIIbβ3, αVβ3, or P-selectin were resuspended in PBS containing 10mM Mn2+, unless otherwise described. Cells were then incubated with Alexa 488–labeled PDI for 10 minutes and analyzed by flow cytometry with a FACSCalibur flow cytometer (BD Biosciences). For analysis of surface platelet PDI expression, WT and β3−/− mouse platelets in HEPES-Tyrode buffer (10:l) containing 0.1% fatty acid–free bovine serum albumin (3 × 108 platelets/mL) were incubated with or without 0.3 U/mL human thrombin or both 10μM ADP and 5μM A23187 for 5 minutes at 37°C. PPACK (50μM) was added to the platelet suspension after thrombin activation. Platelets were incubated with either nonimmune rabbit IgG or rabbit anti-PDI antibodies conjugated to Alexa 488 (30 μg/mL) for 30 minutes. Platelets were fixed with 2% paraformaldehyde for 10 minutes and analyzed by flow cytometry. Data were analyzed with CellQuest software. The expression of surface PDI was obtained from subtraction of the geometric mean intensity value of Alexa 488–labeled rabbit IgG from the geometric mean intensity value of Alexa 488–labeled rabbit anti-PDI. Data were expressed as mean ± SD. The Student t test was used for comparison of WT and β3−/− mouse platelets. Differences were taken to be significant at P < .05.
Surface plasmon resonance
Direct binding of PDI to αIIbβ3 and to β3 was measured by surface plasmon resonance with a Biacore T100. Purified full-length αIIbβ3 (Abcam), isolated from platelets, or recombinant β3 was attached to the chip. Purified recombinant PDI at different indicated concentrations in 10mM HEPES, pH 7.5, 150mM NaCl, 0.05% P20 with or without 2mM MnCl2, was infused over the chip. Binding data were analyzed with Biacore T100 evaluation software.
Mice
The β3 integrin–null mice in a mixed C57BL/6 and 129Sv background have been described previously.25 These mice and matched WT control mice were obtained from The Jackson Laboratory. The Beth Israel Deaconess Medical Center Institutional Animal Care and Use Committee approved all animal care and experimental procedures.
Intravital microscopy in a mouse model of laser-induced arteriolar thrombosis
Intravital videomicroscopy of the cremaster muscle microcirculation was performed as described previously.7,26 Mice were anesthetized with intraperitoneal ketamine (125 mg/kg; Fort Dodge) and xylazine (12.5 mg/kg; Lloyd Laboratories). A tracheal tube (PE90; BD Biosciences) was inserted, and the mouse was maintained at 37°C on a thermo-controlled rodent blanket. To maintain anesthesia, pentobarbital (Ovation Pharmaceuticals) was administered through a cannula (PE10) placed in the jugular vein. After the scrotum was incised, the testicle and surrounding cremaster muscle were exteriorized onto an intravital microscopy tray. The cremaster preparation was superfused with thermo-controlled (37°C) and aerated (95% N2, 5% CO2) bicarbonate-buffered saline throughout the experiment. Alexa- or DyLight-labeled antibodies were infused into mice before arteriolar wall injury.
Arteriolar wall injury was induced with a MicroPoint laser system (Photonics Instruments) at the vessel wall as described previously.26 One or 2 pulses with an equal setting of laser power were used to induce vessel wall injury. Approximately 10 thrombi were generated in a single mouse, with new thrombi formed proximal to previous thrombi. Microvessel data were obtained with an Olympus AX microscope with a 60 × 0.9 numeric aperture water immersion objective. Digital images were captured with a Cooke Sensicam CCD camera in 640 × 480 format. Image analysis was performed with Slidebook Version 4.2 (Intelligent Imaging Innovations). Bright-field and wide-field fluorescence images were captured at exposure times of 10 and 50 ms, respectively. Data captured digitally were collected for 4-5 minutes after vessel wall injury. Representative images were binarized to facilitate visualization, but the median curves include the full range of data. The kinetics of PDI accumulation, fibrin generation, and/or platelet thrombus formation were analyzed by determining median fluorescence values over time in approximately 19-28 thrombi.7
Preparation of washed mouse platelets
Sodium citrate–treated mouse blood (0.8 mL) obtained from WT or β3−/− mice (6-8 weeks old) was centrifuged at 200g for 10 minutes. The plasma (150 μL) and buffy coat (150 μL) were transferred to a separate tube and recentrifuged at 200g for 3 minutes. The platelet-rich plasma was collected and centrifuged at 600g for 3 minutes in the presence of 0.5μM prostaglandin E1. The pellet was suspended in HEPES-Tyrode buffer containing 10% sodium citrate solution and 0.25μM prostaglandin E1 and centrifuged at 600g for 3 minutes. Platelets were resuspended in HEPES-Tyrode buffer.
Secretion of PDI from WT and β3−/− mouse platelets
Mouse platelets in HEPES-Tyrode buffer (1 × 109 platelets/100 μL) were incubated with human thrombin (0.3 U/mL) for 5 minutes at 37°C. PPACK (50μM) was added to quench thrombin activity, followed by centrifugation at 600g for 5 minutes. The supernatant was collected and recentrifuged at 1000g for 5 minutes to eliminate any residual platelets. The pellet was solubilized with 100 μL of SDS lysis buffer (Tris-HCl, pH 7.4, containing 150mM NaCl, 4% SDS, 6M urea, 2mM EDTA, and a protease inhibitor cocktail). The releasate and lysate of mouse platelets, 5 μL, were analyzed by SDS-PAGE under reduced conditions and immunoblotted with a rabbit polyclonal anti-PDI antibody.
Coagulation assay
Mouse plasma was obtained from sodium citrate–treated blood (0.8 mL) by centrifugation at 1000g for 10 minutes. The plasma was further centrifuged at 2000g for 5 minutes to eliminate any residual cells. Cephalin (120 μL) was added to 120 μL of the prewarmed mouse plasma. After incubation for 5 minutes at 37°C, CaCl2 was added to a final concentration of 10mM to initiate plasma clotting. The clotting time was measured with a platelet aggregometer (Chrono-log).
Bone marrow transplantation and genotype analyses
Bone marrow cells of WT and β3−/− male mice (6-8 weeks old) were harvested from both femurs of donor mice that were euthanized. Red blood cells in bone marrow cells were lysed with a lysis buffer (Sigma-Aldrich), and marrow cells were washed 3 times with ice-cold RPMI 1640, 2.1mM l-glutamine, 100 U/mL penicillin, 100 mg/mL streptomycin, 10 U/mL heparin, and 20mM HEPES, pH 7.4. Recipient WT and β3−/− male mice (6-8 weeks old) were fed with sterile food and acidic water, pH 3.0, containing 0.1 mg/mL neomycin 1 week before irradiation. The recipient mice underwent 2 cycles of radiation (650 rad; 6.5 Gy) given 3 hours apart before receiving 5 × 106 bone marrow nucleated cells in 0.2 mL RPMI via a tail-vein injection. Recipient mice were fed with sterile food and acidic water containing neomycin for 2 weeks. After that, the mice were provided with acidic water without the antibiotic. Seven to 8 weeks after transplantation, genotype studies were performed on blood from the transplanted mice. DNA isolated from blood cells was genotyped by PCR with a common forward primer 1 (5′-CTTAGACACCTGCTACGGGC-3′) and reverse primers 2 (5′-CACGAGACTAGTG AGACGTG-3′) and 3 (5′-CCTGCCTGAGGCTGAGTG-3′). PCR products were 538 bp for β3−/− mouse blood and 446 bp for WT mouse blood.25 PCR was performed for 35 cycles with the Advantage 2 PCR kit (BD Biosciences).
Blood counts
Sodium citrate–treated blood (0.8 mL) was collected from anesthetized WT, β3−/−, and transplanted chimeric mice (4-5 months old). Complete blood counts were determined with an automated cell counter (Hemavet 850 FS; Drew Scientific).
Results
We have previously observed the appearance and accumulation of endothelial cell–derived PDI followed by platelet-derived PDI in the injured arteriole during thrombus formation.6,7 We hypothesized that a mechanism must exist for the injured vasculature to bind the secreted PDI and prevent its removal from the injury site by blood flow. Given that β3 integrins may bind to PDI in vitro16 and are expressed on both endothelial cells and platelets, we reexamined whether β3 integrins bind to PDI on the cell surface.
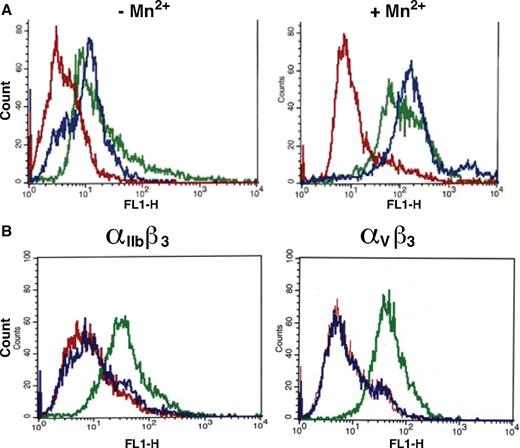
PDI interacts with activated αIIbβ3 and αVβ3
To demonstrate that the interaction of PDI and β3 occurs on the cell surface of platelets and endothelial cells, we examined the interaction of purified Alexa 488 hydrazide–labeled human PDI with CHO cells that expressed the major platelet β3 integrin, αIIbβ3, or the endothelial β3 integrin, αVβ3. Recombinant human PDI conjugated to Alexa 488 hydrazide retained full enzymatic activity, as monitored in the insulin reductase assay. The labeled PDI was added to CHO cells that expressed recombinant αIIbβ3, αVβ3, or P-selectin. Cells were incubated with Mn2+ to activate the integrins. In the presence of Mn2+, PDI bound to the cells that expressed either αIIbβ3 and αVβ3 integrins, whereas no binding was observed to CHO cells that expressed P-selectin (Figure 1A). This interaction was enhanced by the presence of Mn2+, although some binding of PDI to αIIbβ3 and αVβ3 was observed in its absence. This was likely because of ambient metal contamination, because the addition of EDTA completely inhibited PDI binding to both αIIbβ3 and αVβ3 (Figure 1B).
PDI interacts with β3 integrins on cell surfaces. (A) Interaction of PDI with P-selectin, αIIbβ3, or αVβ3. Histograms show fluorescence intensity of Alexa 488–labeled recombinant PDI interacting with CHO cells expressing either P-selectin (red), αIIbβ3 (green), or αVβ3 (blue). CHO cells were pretreated for 10 minutes in PBS with or without Mn2+ and incubated with PDI labeled with Alexa 488. (B) CHO cells expressing either αIIbβ3 (left) or αVβ3 (right) were incubated with Alexa 488–labeled PDI in the presence of Mn+2 (green) or EDTA (blue). The interaction of PDI with CHO cells expressing P-selectin (red) is shown as control.
PDI interacts with β3 integrins on cell surfaces. (A) Interaction of PDI with P-selectin, αIIbβ3, or αVβ3. Histograms show fluorescence intensity of Alexa 488–labeled recombinant PDI interacting with CHO cells expressing either P-selectin (red), αIIbβ3 (green), or αVβ3 (blue). CHO cells were pretreated for 10 minutes in PBS with or without Mn2+ and incubated with PDI labeled with Alexa 488. (B) CHO cells expressing either αIIbβ3 (left) or αVβ3 (right) were incubated with Alexa 488–labeled PDI in the presence of Mn+2 (green) or EDTA (blue). The interaction of PDI with CHO cells expressing P-selectin (red) is shown as control.
The direct interaction of purified αIIbβ3 with purified PDI was further studied by surface plasmon resonance. In the presence of Mn+2, a Kd of 0.67μM was measured in 1 experiment and 1.1μM in a separate experiment (Figure 2A). These results are within the experimental error of this methodology.
PDI interaction with αIIbβ3 and β3 by surface plasmon resonance. Full-length αIIbβ3 (25 μg/mL) or recombinant β3 (25 μg/mL) in 10mM acetate buffer, pH 5 or pH 4.5, respectively, was immobilized on the surface of a Biacore CM5 chip. Different concentrations of PDI (21μM [magenta], 7μM [gray], 2.33μM [gold], 0.78μM [turquoise], 0.26μM [pink], 0.09μM [blue], 0.03μM [green], or 0μM [red]) were injected, and the experiments were performed in duplicate with a running buffer of 10mM HEPES, pH 7.5, 150mM NaCl, 0.05% P20, 2mM MnCl2. The dissociation constant, Kd, was calculated based on the Kon and Koff value. (A) PDI binds to αIIbβ3 with a Kd of 0.67μM. (B) PDI binds to β3 with a Kd of 1.2μM.
PDI interaction with αIIbβ3 and β3 by surface plasmon resonance. Full-length αIIbβ3 (25 μg/mL) or recombinant β3 (25 μg/mL) in 10mM acetate buffer, pH 5 or pH 4.5, respectively, was immobilized on the surface of a Biacore CM5 chip. Different concentrations of PDI (21μM [magenta], 7μM [gray], 2.33μM [gold], 0.78μM [turquoise], 0.26μM [pink], 0.09μM [blue], 0.03μM [green], or 0μM [red]) were injected, and the experiments were performed in duplicate with a running buffer of 10mM HEPES, pH 7.5, 150mM NaCl, 0.05% P20, 2mM MnCl2. The dissociation constant, Kd, was calculated based on the Kon and Koff value. (A) PDI binds to αIIbβ3 with a Kd of 0.67μM. (B) PDI binds to β3 with a Kd of 1.2μM.
Similar results were obtained for the interaction of purified recombinant β3 with purified PDI by surface plasmon resonance. In the presence of Mn+2, a Kd of 1.2μM was measured in 1 experiment and 2.4μM in a separate experiment (Figure 2B). These results are consistent with the primary importance of β3 in this interaction with PDI.
Swiatkowski et al have described the interaction of PDI and αVβ3 also using surface plasmon resonance.16 The apparent Kd for an experiment of 6 minutes, similar to our conditions and performed in the presence of Mn+2, revealed a value of 0.017μM.
PDI activity is not required for PDI-β3 integrin interaction
To determine whether PDI enzymatic function is required for PDI-β3 interaction, Alexa 488 hydrazide–labeled human PDI was incubated with the blocking antibody RL90, then exposed to CHO cells that expressed αIIbβ3 or αVβ3 in the presence of Mn2+. Antibody concentrations of up to 10-fold molar excess over integrin did not interfere with the binding of PDI to β3 integrins (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). We labeled recombinant PDI with Alexa 488 maleimide to covalently modify free sulfhydryl groups in the active site. Alexa 488 maleimide–labeled PDI bound to αVβ3 and αIIbβ3 expressed on CHO cells (supplemental Figure 2) in a manner parallel to Alexa 488 hydrazide–labeled PDI. Thus, integrin activation, but not PDI activity, is required for the interaction of PDI and β3 integrins.
Characterization of laser-induced thrombus formation in β3−/− mice
β3−/− mice are resistant to FeCl3-induced carotid arterial thrombosis.25,26 To confirm that β3−/− mice are protected from platelet thrombus formation at the site of laser-induced arteriolar wall injury used in these studies, intravital microscopy was used in WT and β3−/− mice to monitor platelet accumulation. Platelet thrombi were monitored with rat anti–mouse GPIbβ antibody conjugated to DyLight 649 (red). The expression levels of GPIbβ on the surfaces of WT and β3−/− mouse platelets were equivalent, as determined by flow cytometry (supplemental Figure 3). As previously observed, β3−/− mice did not form a platelet thrombus at the site of vessel wall injury (Figure 3A-B).27 In WT mice, initial platelet accumulation was observed at 15-30 seconds, and the maximum thrombus was detected at 90-100 seconds after vascular injury. Any variability in comparison of these experiments with our earlier experiments can be ascribed to (1) operator variation, in which the time from laser injury to the recording of video may vary; (2) the use of antiplatelet antibodies with different fluorescence intensities (we switched to a CD42 antibody in the present study after using an Fab of a CD41 antibody previously; these antibodies use different fluorochromes and have different fluorescent intensities); and (3) antibody dosage. These differences are not significant, and the temporal pattern of the appearance of PDI, then platelets, then fibrin was routinely observed in all of our experiments with WT mice. These results on β3−/− mice confirm that platelet β3 integrins are required for platelet thrombus formation at the site of arteriolar wall injury.
Platelet thrombus formation after laser-induced arteriolar wall injury in β3−/− mice. (A) Nonblocking rat anti–mouse GPIbβ antibody conjugated to DyLight 649 (0.2 μg/g body weight) was infused into a wild-type (wt) or β3−/− mouse 5 minutes before laser-induced arteriolar wall injury. Representative images of fluorescence associated with platelets (red) are shown over the course of 180 seconds after vessel injury within the context of the bright-field microvascular histology. (B) The median integrated platelet fluorescence (Fplatelets) for 22-23 thrombi in 2 WT or 2 β3−/− mice infused with the anti-GPIbβ antibody conjugated to DyLight 649 is presented over the course of 250 seconds after vessel injury.
Platelet thrombus formation after laser-induced arteriolar wall injury in β3−/− mice. (A) Nonblocking rat anti–mouse GPIbβ antibody conjugated to DyLight 649 (0.2 μg/g body weight) was infused into a wild-type (wt) or β3−/− mouse 5 minutes before laser-induced arteriolar wall injury. Representative images of fluorescence associated with platelets (red) are shown over the course of 180 seconds after vessel injury within the context of the bright-field microvascular histology. (B) The median integrated platelet fluorescence (Fplatelets) for 22-23 thrombi in 2 WT or 2 β3−/− mice infused with the anti-GPIbβ antibody conjugated to DyLight 649 is presented over the course of 250 seconds after vessel injury.
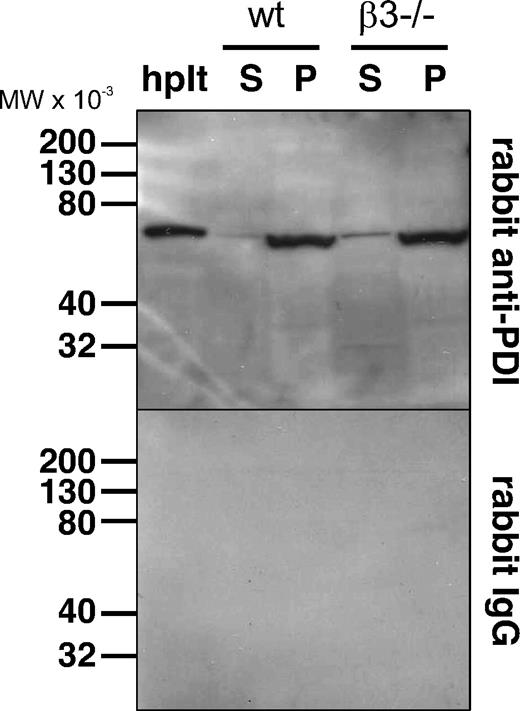
Mouse β3−/− platelets and WT platelets contain equivalent amounts of PDI and secrete PDI
We investigated whether β3 deficiency influences platelet storage or secretion of PDI. The releasate and lysate of thrombin-activated WT and β3−/− mouse platelets were subjected to electrophoresis and analyzed for PDI by immunoblotting with rabbit polyclonal anti-PDI antibodies. Equivalent amounts of PDI were detected in the lysate of WT and β3−/− mouse platelets (Figure 4). Furthermore, β3−/− mouse platelets released similar amounts of PDI as WT platelets in response to thrombin (Figure 4).
Comparison of PDI secretion from WT and β3−/− mouse platelets. (A) Platelets from wild-type (wt) and β3−/− mice (1 × 109 platelets/100 μL) were incubated with thrombin for 5 minutes, and the supernatant and pellet were separated. The pellet was solubilized with 0.1 mL of SDS lysis buffer. Washed human platelets (1 × 109 platelets/mL) were lysed with 0.1 mL of SDS lysis buffer. Washed human platelets (10 μL), the platelet releasates (S; 5 μL), and platelet lysates (P; 5 μL) of WT and β3−/− mouse platelets (5 μL) were electrophoresed in an SDS-PAGE gel and immunoblotted with rabbit polyclonal anti-PDI antibodies or nonimmune rabbit IgG. hplt indicates human platelets.
Comparison of PDI secretion from WT and β3−/− mouse platelets. (A) Platelets from wild-type (wt) and β3−/− mice (1 × 109 platelets/100 μL) were incubated with thrombin for 5 minutes, and the supernatant and pellet were separated. The pellet was solubilized with 0.1 mL of SDS lysis buffer. Washed human platelets (1 × 109 platelets/mL) were lysed with 0.1 mL of SDS lysis buffer. Washed human platelets (10 μL), the platelet releasates (S; 5 μL), and platelet lysates (P; 5 μL) of WT and β3−/− mouse platelets (5 μL) were electrophoresed in an SDS-PAGE gel and immunoblotted with rabbit polyclonal anti-PDI antibodies or nonimmune rabbit IgG. hplt indicates human platelets.
β3−/− plasma supports normal fibrin generation
Because we wished to assess fibrin formation after laser-induced injury in β3−/− mice, we determined that there was no unanticipated defect in fibrin generation in plasma from β3−/− mice using a modified activated partial thromboplastin time. WT and β3−/− mouse plasma were incubated in the presence of cephalin and Ca2+. There was no significant difference in the time to clot formation between WT (45.6 ± 8.3 seconds) and β3−/− (38.1 ± 4.2 seconds) mouse plasma (data represent mean ± SD, n = 4; P = .15 vs WT control by Student t test).
PDI accumulation is greatly reduced at the site of vessel injury in β3−/− mice
To investigate whether β3 integrins are important for PDI capture after laser-induced vessel wall injury, we compared PDI accumulation in WT and β3−/− mice after vascular injury using intravital microscopy. Because a platelet thrombus does not form in the β3−/− mice, the effect of the absence of αVβ3 integrin on accumulation of PDI secreted by endothelial cells can be monitored in these mice.6,25,27 A noninhibitory rabbit anti-PDI antibody conjugated to Alexa 488 (green) and a monoclonal anti-fibrin–specific antibody conjugated to Alexa 647 (red) were infused before vessel injury to label PDI and fibrin, respectively. In contrast to WT mice, β3−/− mice showed minimal accumulation of extracellular PDI at the site of arteriolar wall injury (Figure 5A-B). Failure to observe PDI accumulation at the site of laser injury indicates a role for β3 in binding PDI in vivo at a site of vascular injury. Fibrin generation was decreased markedly after vessel injury in β3−/− mice compared with that observed in WT mice (Figure 5A,C). The absence of fibrin cannot be explained by the absence of a platelet surface to support thrombin generation, because we have previously shown that normal levels of fibrin are generated after laser injury in Par4−/− mice lacking the platelet thrombin receptor28 and in WT mice without platelet thrombi after treatment with eptifibatide.6 These results indicate that β3 integrins play a role in fibrin generation at the site of vessel injury that is unrelated to the presence of activated platelets and is dependent on β3 integrin–supported PDI accumulation at the site of injury.
PDI accumulation and platelet thrombus formation in β3−/− mice. Noninhibitory rabbit anti-PDI antibody conjugated to Alexa 488 (0.5 μg/g body weight) and antifibrin-specific antibody conjugated to Alexa 647 (0.3 μg/g body weight) were infused into a wild-type (wt) or β3−/− mouse 5 minutes before laser-induced arteriolar wall injury. (A) Representative images of the fluorescence signals associated with PDI (green) and fibrin (red) are shown over a course of 180 seconds after vessel injury within the context of the bright-field microvascular histology. The median integrated fluorescence associated with PDI fluorescence (FPDI) and fibrin fluorescence (Ffibrin) after infusion of anti-PDI antibodies (B) and antifibrin antibodies (C) in 3 WT mice (n = 28 thrombi) and 3 β3−/− mice (n = 25 thrombi) is presented over a course of 250 seconds after vessel wall injury.
PDI accumulation and platelet thrombus formation in β3−/− mice. Noninhibitory rabbit anti-PDI antibody conjugated to Alexa 488 (0.5 μg/g body weight) and antifibrin-specific antibody conjugated to Alexa 647 (0.3 μg/g body weight) were infused into a wild-type (wt) or β3−/− mouse 5 minutes before laser-induced arteriolar wall injury. (A) Representative images of the fluorescence signals associated with PDI (green) and fibrin (red) are shown over a course of 180 seconds after vessel injury within the context of the bright-field microvascular histology. The median integrated fluorescence associated with PDI fluorescence (FPDI) and fibrin fluorescence (Ffibrin) after infusion of anti-PDI antibodies (B) and antifibrin antibodies (C) in 3 WT mice (n = 28 thrombi) and 3 β3−/− mice (n = 25 thrombi) is presented over a course of 250 seconds after vessel wall injury.
Chimeric mice generated by reciprocal bone marrow transplantation in WT and β3−/− mice
We independently studied the roles of endothelial and platelet β3 integrins in extracellular PDI accumulation after vessel injury by performing bone marrow transplantation with WT and β3−/− mice. We generated the following chimeric mice by reciprocal bone marrow transplantation in WT and β3−/− mice: WT donor bone marrow into WT recipient mice (WT/WT); β3−/− donor bone marrow into WT recipient mice (β3−/WT); β3−/− donor bone marrow into β3−/− recipient mice (β3−/β3−); and WT donor bone marrow into β3−/− recipient mice (WT/β3−). In these chimeric mice, WT mice receiving donor bone marrow from β3−/− mice have platelets that lack β3 integrins, whereas β3−/− mice receiving donor bone marrow from WT mice have endothelial cells that lack β3 integrins.
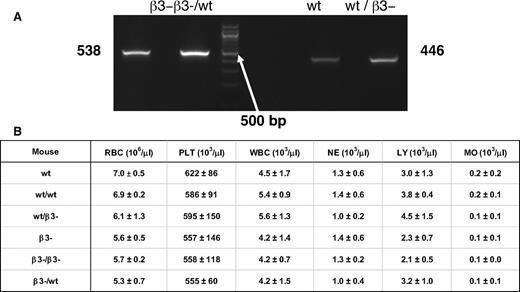
Characterization of mice after bone marrow transplantation
To confirm transplantation of the donor mouse hematopoietic cells into the recipient mice, we performed PCR using chimeric mouse blood and blood from β3−/− and WT mice. In representative genotyping experiments, PCR products in WT/β3− chimeras exhibited the 446-bp fragment observed in WT mouse blood; β3−/WT chimeras exhibited the 538-bp fragment observed in β3−/− mouse blood (Figure 6A). These results indicate that WT/β3− chimeras were WT for their hematopoietic cells, whereas β3−/WT chimeras were positive for the β3−/− genotype for their hematopoietic cells.
Analysis of chimeric and homozygous mouse blood. (A) PCR was performed with whole blood of β3−/−, WT, and WT/β3−/− and β3−/−/WT chimeric mice. PCR products were obtained as 538 bp for β3−/WT and 446 bp for WT/β3−/−. (B) Blood cell counts of mice after bone marrow transplantation. Complete blood counts were obtained, including red cells (RBC), platelets (PLT), white blood cells (WBC), neutrophils (NE), lymphocytes (LY), and monocytes (MO). Data represent mean ± SD of 4-5 independent experiments.
Analysis of chimeric and homozygous mouse blood. (A) PCR was performed with whole blood of β3−/−, WT, and WT/β3−/− and β3−/−/WT chimeric mice. PCR products were obtained as 538 bp for β3−/WT and 446 bp for WT/β3−/−. (B) Blood cell counts of mice after bone marrow transplantation. Complete blood counts were obtained, including red cells (RBC), platelets (PLT), white blood cells (WBC), neutrophils (NE), lymphocytes (LY), and monocytes (MO). Data represent mean ± SD of 4-5 independent experiments.
Transplanted mice had normal numbers and distribution of blood cells (Figure 6B). Blood cell counts and leukocyte differential counts in representative chimeric mice were comparable with those in control mice.
To determine whether fibrin generation was significantly affected by transplantation, we performed modified partial thromboplastin times on the plasma isolated from chimeric mouse blood. There was no significant difference in clotting times between chimeric and control mice.
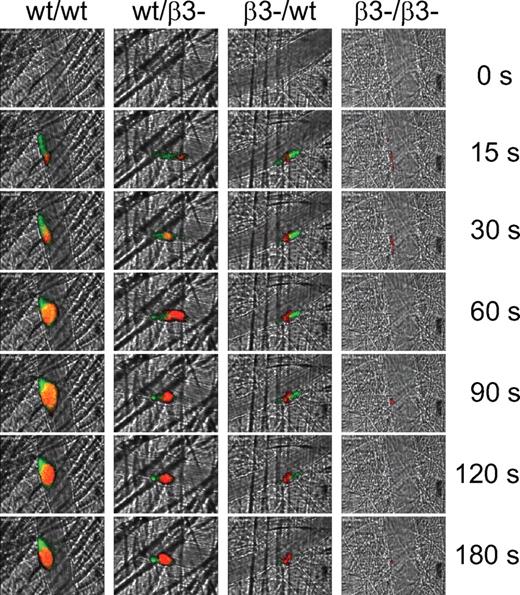
PDI accumulation and function in chimeric mice
To determine the contribution of endothelial and platelet β3 integrins in PDI accumulation after vessel injury, both Alexa 488–labeled anti-PDI antibody and DyLight 649–labeled anti-GPIbβ antibody were infused into transplanted mice before vessel injury to detect and quantitate PDI and platelets, respectively. The representative results of studies of PDI accumulation and platelet thrombus formation are shown in Figure 7. Quantitative results of the median of multiple thrombi in each group are presented in Figure 8.
PDI and platelet accumulation in chimeric mice after vascular injury. Chimeric mice were generated by reciprocal bone marrow transplantation between wild-type (WT) and β3−/− mice. Noninhibitory rabbit anti-PDI antibody (0.5 μg/g body weight) conjugated to Alexa 488 was infused into mice with a nonblocking rat anti–mouse GPIbβ antibody conjugated to DyLight 649 5 minutes before laser-induced arteriolar wall injury. Representative images associated with platelets (red) and PDI (green) are shown over a time course of 180 seconds after vessel injury within the context of the bright-field microvascular histology.
PDI and platelet accumulation in chimeric mice after vascular injury. Chimeric mice were generated by reciprocal bone marrow transplantation between wild-type (WT) and β3−/− mice. Noninhibitory rabbit anti-PDI antibody (0.5 μg/g body weight) conjugated to Alexa 488 was infused into mice with a nonblocking rat anti–mouse GPIbβ antibody conjugated to DyLight 649 5 minutes before laser-induced arteriolar wall injury. Representative images associated with platelets (red) and PDI (green) are shown over a time course of 180 seconds after vessel injury within the context of the bright-field microvascular histology.
Quantitation of fluorescence associated with PDI and platelets in 4 transplanted mouse cohorts. The median integrated platelet (A) and PDI (B) fluorescence (F) after infusion of anti-GPIb antibody and anti-PDI antibody in each of the transplanted mice is presented over a time course of 240 seconds after vessel wall injury. 1 indicates WT/WT (n = 25 thrombi); 2, WT/β3− (n = 28 thrombi); 3, β3−/WT (n = 26 thrombi); and 4, β3−/β3− (n = 26 thrombi; donor/recipient).
Quantitation of fluorescence associated with PDI and platelets in 4 transplanted mouse cohorts. The median integrated platelet (A) and PDI (B) fluorescence (F) after infusion of anti-GPIb antibody and anti-PDI antibody in each of the transplanted mice is presented over a time course of 240 seconds after vessel wall injury. 1 indicates WT/WT (n = 25 thrombi); 2, WT/β3− (n = 28 thrombi); 3, β3−/WT (n = 26 thrombi); and 4, β3−/β3− (n = 26 thrombi; donor/recipient).
As in WT mice (Figure 5), PDI rapidly accumulated on the vessel wall and within the developing platelet thrombus in the WT/WT control mice. A typical platelet thrombus formed at the site of vessel injury site in WT/WT mice (Figures 7 and 8A). Similarly, as in the β3−/− mice (Figures 3 and 5), PDI and platelets did not accumulate on the vessel wall in the β3−/β3− control mice. In contrast, PDI accumulation and platelet thrombus formation were significantly reduced at the vessel injury site in WT/β3− mice compared with WT/WT mice (Figure 8), which indicates that endothelial αVβ3 integrin plays a role in both PDI and platelet accumulation at the vessel injury site. In β3−/WT mice, a minimal platelet thrombus formed at the injury site in the absence of β3 integrins on platelets. Significantly reduced PDI accumulation was also observed at the site of vessel injury (Figure 8B). These results suggest that both endothelial αVβ3 integrin and platelet β3 integrins are important for initial and sustained PDI accumulation and platelet thrombus development after vessel injury. Furthermore, these results indicate that in addition to platelet β3 integrins, the endothelial αVβ3 integrin is important for platelet thrombus formation at the site of laser-induced vessel injury.
Discussion
PDI is secreted first from the endothelium and then from bound platelets during cell activation after vascular injury, and this is among the initial steps in thrombus generation. Inhibition of extracellular PDI after injury greatly impairs platelet thrombus formation and fibrin generation, which emphasizes the functional importance of PDI.7-9 One of the primary questions raised by these observations is the mechanism by which secreted PDI remains associated with the disrupted endothelium and developing thrombus. The capture of PDI by the endothelium and platelet thrombus requires a critical interaction between extracellular PDI and a cell surface receptor. Given the distribution of β3 integrins on both platelets and endothelium and literature reports indicating the interaction of PDI with the αVβ3 integrin,16 we explored the role of β3 integrins in the capture of PDI secreted from the endothelium and from platelets after vascular injury.
Jordan et al observed the interaction of PDI with ERp5, another thiol isomerase, but reported that they observed no interaction between PDI and β3.17 In contrast, Swiatkowska et al described the interaction of endothelial αVβ3 with PDI.16 This controversy over the interaction of PDI with integrins containing β3 led us to reinvestigate this question. We confirmed that PDI binds directly to αVβ3, as was originally demonstrated with endothelial cells treated with Mn+2.16 PDI bound to CHO cells that expressed αVβ3 but not cells that expressed P-selectin. Moreover, we observed interaction between PDI and platelet αIIbβ3 by analysis of binding of PDI to CHO cells that expressed αIIbβ3. Measurement of the binding constant, Kd, between purified PDI and purified full-length αIIbβ3 revealed a value of approximately 1μM. Given the similarity of the binding affinity of PDI for αIIbβ3 and β3, we suggest that the α-subunit does not contribute significantly to the binding properties of PDI to αIIbβ3. The interaction of PDI with β3 integrins required stabilization of the active conformer of the integrin with Mn+2 but was not inhibited by either an inhibitory antibody to PDI or derivatization of free sulfhydryl groups on PDI. PDI lacks the Arg-Gly-Asp sequence found in many integrin ligands that is responsible for cell adhesion and cell matrix interaction.29
β3 deficiency in mice has been shown to be associated with a greatly prolonged bleeding time, impaired clot retraction, and nearly absent uptake of fibrinogen on β3−/− platelets.25 Spontaneous hemorrhage in β3−/− mice reduced survival. Unlike WT mice, β3−/− mice were protected from hemorrhagic lesions as a complication of the local Shwartzman reaction.25 Carotid artery thrombosis after ferric chloride treatment was significantly impaired in β3−/− mice compared with WT and β3+/− heterozygotes.27 In contrast to WT mice in which a platelet-rich thrombus occluded the lumen, β3−/− mice showed but a single layer of platelets but no occlusive thrombus.27 We now extend these original findings to demonstrate the absence of fibrin generation after laser-induced vascular injury in β3−/− mice because of the lack of accumulated PDI. This raises the question of whether the deficiency in fibrin generation contributes to the hemorrhagic phenotype of patients with Glanzmann thrombasthenia, particularly homozygotes or compound heterozygotes.30 Although a role for platelets in fibrin generation was proposed on the basis of a defect in thrombasthenic platelets,31-33 more recently this defect has been ascribed as possibly related to a release defect associated with platelet polyphosphates.34 However, we suggest that the procoagulant defect ascribed to Glanzmann thrombasthenia may be caused by the absence of PDI during thrombus formation rather than the failure of polyphosphate secretion,34 because we have previously demonstrated that PDI is required for fibrin generation.7 In the present work, we demonstrate that fibrin generation is greatly impaired in β3−/− mice, not because of the failure to form a platelet thrombus or the inability to activate platelets, but rather because of the failure to accumulate extracellular PDI at the injury site because of the absence of its cellular receptor, β3 integrin.
Decreased extracellular PDI in β3−/− mice could be caused by decreased stored PDI in β3−/− platelets or decreased secretion of PDI from β3−/− platelets. We demonstrate that PDI content and PDI secretion of β3−/− platelets appear similar to WT platelets. Therefore, we suggest that the failure of secreted PDI to remain associated with the injured vasculature and developing thrombus is attributable to the absence of a counterreceptor, specifically the β3 integrins, exposed in the lumen of the vasculature.
We have previously shown eptifibatide blocks αIIbβ3-mediated platelet binding to the injured vessel wall, thus precluding the delivery of extracellular PDI6 ; in the β3−/WT chimera, we anticipate that there would be neither αIIbβ3-mediated platelet binding nor αVβ3-mediated platelet binding to the injured vessel wall, again precluding the delivery of extracellular PDI. We might expect that the results from these 2 experiments would be similar. However, significantly less PDI was observed in the β3−/WT chimera than in the eptifibatide-treated WT mouse. We can speculate between 2 possible explanations. First, platelets from the β3−/WT chimera will lack αIIbβ3 and αVβ3, whereas eptifibatide-treated WT mice will interfere only in αIIbβ3-mediated platelet binding. If αVβ3 contributes to platelet binding in any significant way, this interaction will be preserved in the eptifibatide-treated WT mouse and will allow delivery of PDI to the WT endothelium. Alternatively, eptifibatide, a pharmacologic agent, may allow for the coating of a monolayer of platelets in an interaction that is not dependent on αIIbβ3. These platelets may secrete PDI on activation.
PDI plays a central role in the initiation of thrombus formation and is important for both platelet aggregation and fibrin generation. Whether it functions as an oxidoreductase or chaperone and whether it acts directly on platelet receptors or tissue factor remain unknown. It has been suggested that both αIIbβ3 and tissue factor may undergo changes in their oxidation state (αIIbβ3 by reduction of several disulfide bonds14 and tissue factor by formation of a disulfide bond35 ), leading to protein activation. Regardless of this mechanism, the presence of PDI at the site of vascular injury is critical for thrombus formation, and the β3 integrins are required for capture of PDI at this site.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Uri Seligsohn for a critical review of the manuscript and his thoughtful suggestions. Dr Sanford Shattil provided CHO cells expressing β3 integrins.
This work was supported by grants from the National Institutes of Health.
National Institutes of Health
Authorship
Contribution: J.C. and D.R.K. designed and performed experiments, analyzed the results, and wrote the manuscript; L.L., M.H., and G.M.-S. performed experiments and analyzed the results; and B.C.F. and B.F. designed the experiments and wrote the manuscript.
Conflict-of-interest statement: The authors declare no competing financial interests.
The current affiliation for J.C. is Department of Pharmacology, University of Illinois College of Medicine, Chicago, IL. The current affiliation for D.R.K. is Western New England University, Springfield, MA.
Correspondence: Dr Bruce Furie, Center for Life Science, Rm 903, 3 Blackfan Cir, Boston, MA 02215; e-mail: bfurie@bidmc.harvard.edu.

![Figure 2. PDI interaction with αIIbβ3 and β3 by surface plasmon resonance. Full-length αIIbβ3 (25 μg/mL) or recombinant β3 (25 μg/mL) in 10mM acetate buffer, pH 5 or pH 4.5, respectively, was immobilized on the surface of a Biacore CM5 chip. Different concentrations of PDI (21μM [magenta], 7μM [gray], 2.33μM [gold], 0.78μM [turquoise], 0.26μM [pink], 0.09μM [blue], 0.03μM [green], or 0μM [red]) were injected, and the experiments were performed in duplicate with a running buffer of 10mM HEPES, pH 7.5, 150mM NaCl, 0.05% P20, 2mM MnCl2. The dissociation constant, Kd, was calculated based on the Kon and Koff value. (A) PDI binds to αIIbβ3 with a Kd of 0.67μM. (B) PDI binds to β3 with a Kd of 1.2μM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/120/3/10.1182_blood-2011-08-372532/4/m_zh89991293890002.jpeg?Expires=1766140231&Signature=wv1J3CeG7Ip4q4-itY~CF66lfzo7snGuxv0k7jTBc0jjOcqrGyo9MdNpG2tEm8zR1yu4oF0htpV9bDtFfUpmWf5gxp-WMcn6hBKNk84I7q9WbCZ159z98n5qCuEsgI3qE3OWY3efnCRGjkGRIpPH-Poyz3HY83Oh8qFYBAh0-jN2C4iHLKTCss9VLChUm0ovvu5~hNr7WkXaP~Frb8~QfgvEPmfxGNjgUCXhBFhjAav4AVJtuaMdsBzYXf~hctcDYf6DNvKU4f3wrAhERlX-rxisD6YfANF1Nuc-NX1u2akEN18HXuI7JnvURJBPF9RUiNXbsr2KGSqTCeUO9SfUeg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)







![Figure 2. PDI interaction with αIIbβ3 and β3 by surface plasmon resonance. Full-length αIIbβ3 (25 μg/mL) or recombinant β3 (25 μg/mL) in 10mM acetate buffer, pH 5 or pH 4.5, respectively, was immobilized on the surface of a Biacore CM5 chip. Different concentrations of PDI (21μM [magenta], 7μM [gray], 2.33μM [gold], 0.78μM [turquoise], 0.26μM [pink], 0.09μM [blue], 0.03μM [green], or 0μM [red]) were injected, and the experiments were performed in duplicate with a running buffer of 10mM HEPES, pH 7.5, 150mM NaCl, 0.05% P20, 2mM MnCl2. The dissociation constant, Kd, was calculated based on the Kon and Koff value. (A) PDI binds to αIIbβ3 with a Kd of 0.67μM. (B) PDI binds to β3 with a Kd of 1.2μM.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/120/3/10.1182_blood-2011-08-372532/4/m_zh89991293890002.jpeg?Expires=1766214251&Signature=aXmfKRyiieW5VCU21WX-mpiVWHGFIWuYhZ~g0AL9IyFlkHn2mXe4b-2jH0DCQtuixHti5MRn1VBhPSPX3B~afN4l8LrtEviRuf2Vczad9g2nRKgmfa8kHYu8b7QkwxwSimbcSZzKWbv6lXvUASg5oXCm2r9lc8u1ZygVnsMrqIuBibySOZFwfr8yJcLTYZ5G~kz2w-um33Z-pSdEiiNOaUC-w9Rqa2FYVZ5iPbevZrvaGChMQArSCLPD880AaLvUPw-7eWEOTTwQHbZTsyK75~Uk1abpJXzdGR2AYFx1raSLadIBUOqs88IiZ1cSqr2ZfxK0ss0~X55bKXLSc1vvkg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)