To the editor:
Leukemoid reaction (white blood cells [WBCs] >50 000/μL) secondary to inflammatory or neoplastic process describes elevated WBC counts in the peripheral blood (PB).1 To our knowledge, there has only been 1 case report of a leukemoid reaction in the cerebrospinal fluid (CSF) as a late complication of zoster.2 We report a leukemoid reaction in the CSF of an acute myelogenous leukemia (AML) survivor with human herpes zoster (VZV) meningoencephalitis.
A 54-year-old male underwent allogeneic hematopoietic transplantation (AHT) for AML using a fully matched brother. The AML showed diploid cytogenetics; FLT-3, NMP, and CEBPA mutation analysis was not available. His conditioning consisted of melphalan, fludarabine, and alemtuzumab; tacrolimus was used for graft-versus-host disease prophylaxis. He did well post AHT, only having chronic limited skin graft-versus-host disease that did not require continued immunosuppressants. At 1 year post AHT, he received the diphtheria, tetanus, pertussis, meningococcal, pneumococcal, Haemophilus influenzae b, hepatitis A and B, and inactivated poliovirus vaccine vaccinations; he was not vaccinated for measles or zoster. He was on bactrim and acyclovir prophylaxis. At 1.8 months post AHT, he presented with headache, seizures, and vesicular skin rash.
Magnetic resonance imaging showed diffuse meningeal enhancement without focal lesions. CSF analysis showed xanthochromic fluid with red blood cells 252/cmm, WBCs 576/cmm, and glucose 159 mg/dL (blood glucose 154).
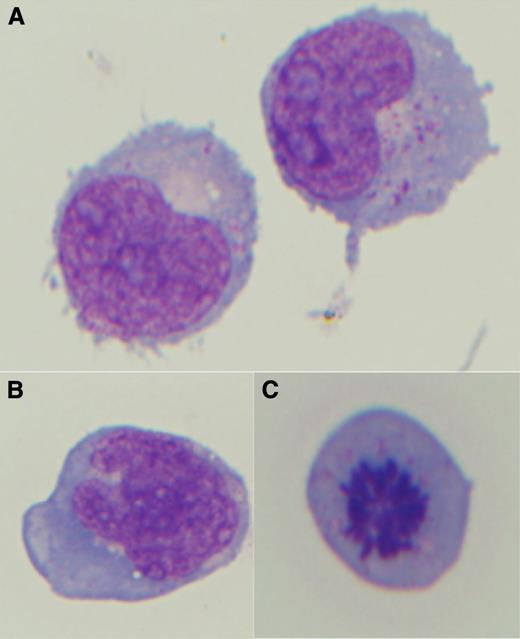
Two CSF cytology specimens showed monocytic cells that morphologically resembled blasts, with delicate chromatin, moderate gray-blue cytoplasm with vacuoles and azurophilic granules, and occasional mitosis (Figure 1). Corresponding flow cytometry showed 21% and 24% mature monocytes with no immunophenotypic aberrancy. No myeloblasts and no cells of the prior leukemic immunophenotype (CD34+, CD117+, CD33+, CD13+, CD14–) were identified by flow cytometry. There were no nucleated red blood cells, megakaryocytes, or left-shifted granulocytes in different stages of maturation that would suggest bone marrow contamination. Cytogenetics studies were not performed on the CSF.
CSF cytology shows atypical reactive monocytic cells. (A) Morphologic features show delicate nuclear chromatin, multiple prominent nucleoli, and moderate gray-blue cytoplasm with azurophilic granules. (B) Some reactive monocytes show delicate-lacey chromatin with more irregular nuclear contours. (C) Occasional mitosis is present.
CSF cytology shows atypical reactive monocytic cells. (A) Morphologic features show delicate nuclear chromatin, multiple prominent nucleoli, and moderate gray-blue cytoplasm with azurophilic granules. (B) Some reactive monocytes show delicate-lacey chromatin with more irregular nuclear contours. (C) Occasional mitosis is present.
The PB showed the following hematologic indices: WBCs 10 400/μL (4.5-11), hemoglobin 13.2 g/μL (12-16), mean corpuscular volume 94.7 fl (82-100), mean corpuscular hemoglobin 91 pg (27-34), platelets 166 000/μL (150-400), with a differential of 85% neutrophils, 7% lymphocytes, 7% monocytes, and 1% basophils. The morphologically immature cells seen in the CSF were not seen in the PB, suggesting that these cells originated in the CSF. PB flow cytometry showed no blasts and 7% mature monocytes with no aberrancy.
CSF and PB polymerase chain reaction for VZV revealed >1.0 × 108 and 327 000 copies (Vira core), respectively. He had a childhood history of chicken pox without recent VZV exposure. Despite antiviral treatment and supportive care, he died. Autopsy showed histologic findings of subacute/chronic meningoencephalitis with no acute leukemia involving the central nervous system.
When considering AML relapse in the CSF of an AHT patient, consider flow cytometric and microbiology studies to rule out a reactive process. Disseminated VZV is the most frequent late infection of AHT.3
Authorship
Contribution: R.K.B. and A.W.Z. provided the pathological findings; and R.T.K. provided the clinical findings.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rammurti T. Kamble, The Methodist Hospital, 6565 Fannin St, Houston, TX 77030; e-mail: rtkamble@tmhs.org.