Abstract
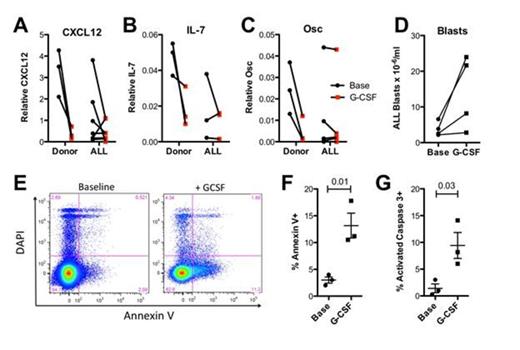
Similar to normal lymphoid progenitors, acute lymphoblastic leukemia (ALL) blasts receive key growth and survival signals from the bone marrow microenvironment which contributes to chemotherapy resistance and disease relapse. We previously reported that treatment with G-CSF in mice results in a marked a marked suppression of lymphopoiesis by targeting lymphoid niches in the bone marrow (Day et al., ASH abstract #1246, 2012). Specifically, G-CSF suppresses the expression of lymphoid trophic factors from osteoblasts and CXCL12-abundant reticular (CAR) cells, including CXCL12, stem cell factor, and interleukin-7, and interleukin-6. We hypothesized that disruption of lymphoid niches in the bone marrow by G-CSF mediated suppression of lymphoid trophic factors will render ALL cells more sensitive to chemotherapy.
We conducted a pilot study of G-CSF priming in patients with relapsed or refractory ALL (NCT01331590). Our preclinical data indicates that the timing of G-CSF in relation to chemotherapy is critical and that G-CSF must be given for at least 4 days prior to chemotherapy to achieve its maximal effect on the BM microenvironment. In this study, G-CSF (10 µg/kg/d) was administered continuously from day 1 until neutrophil recovery followed by ifosfamide 3330 mg/m2/d CIVI on days 4-6, etoposide 150 mg/m2 IV BID, and dexamethasone 5 mg/m2 BID on Days 4-10. Peripheral blood and BM samples are obtained at baseline and after 4 days of G-CSF (prior to chemotherapy). Where sufficient material was available, the baseline and day 4 G-CSF blood and BM samples were analyzed to assess: 1) changes in the BM microenvironment; 2) ALL cell mobilization into the blood; and 3) ALL cell proliferation and apoptosis. To assess expression of B trophic factors by BM stromal cells, we analyzed RNA from BM core biopsies at baseline and at day 4.
Ten patients with with relapsed or refractory ALL with a median age of 47 years (range 21-69) have been enrolled. One subject developed leukocytosis to 67K/mm3 from baseline of 20K/mm3 requiring temporary cessation of G-CSF and earlier initiation of chemotherapy. One treatment related death occured on study. Three of 10 patients have achieved a CR/CRi (30%). Importantly, there were no cases of delayed hematologic recovery. Compared to healthy volunteers, the baseline expression of CXCL12, IL-7, and osteocalcin mRNA in the bone marrow was markedly variable, with some samples displaying very low expression. Nonetheless, G-CSF resulted in a 2-fold or greater decrease in CXCL12 expression in 6 of 7 cases tested. These data suggest that, although the BM microenvironment is disrupted at baseline in many patients with relapsed/refractory ALL, G-CSF can suppress lymphoid trophic factors even further. In 4 of 5 cases, mobilization of ALL blasts after G-CSF to the peripheral blood was observed (average fold-increase: 3.1 ± 0.95; range 1.3 to 6.2-fold). Interestingly, in the single case with minimal mobilization, little change in bone marrow expression of CXCL12 with G-CSF treatment was observed. ALL blast proliferation and apoptosis in the bone marrow was measured by flow cytometry before and after G-CSF priming. In all 3 samples that were analyzed, a significant increase in apoptosis, as measured by Annexin V surface expression, was observed [% Annexin V+ ALL blasts: 2.9 ± .81% (baseline) versus 13.2 ± 4.0% (G-CSF); p = 0.01]. Similar data were observed measuring apoptosis by activated caspase 3 expression. No change in ALL cell blast proliferation (as measured by Ki67 and DAPI staining) was observed.
Off Label Use: sorafenib for AML.
Author notes
Asterisk with author names denotes non-ASH members.