Abstract
Transfusion-dependent patients with severe cardiac siderosis often require intensive iron chelation therapy for a limited time to facilitate rapid removal of iron from the heart, allowing patients to move from a high-risk (cardiac T2*<10 ms) to lower risk (≥10 ms) status for heart failure. Oral deferasirox (DFX) monotherapy has been shown to improve cardiac T2*, but data on the combined use of DFX and deferoxamine (DFO) are limited.
To evaluate efficacy and safety of investigational DFX–DFO in combination followed by DFX monotherapy in patients with severe transfusional cardiac siderosis.
The prospective, Phase II, open-label, multinational HYPERION study evaluated DFX–DFO in combination followed by DFX monotherapy in transfusion-dependent patients with severe cardiac siderosis (NCT01254227). Patients enrolled were ≥10 years with CMR-measured cardiac T2* 5–<10 ms, left ventricular ejection fraction (LVEF) ≥56%, R2-MRI liver iron concentration (LIC) ≥7 mg Fe/g dw. Starting dose was DFX 20 mg/kg/d, 7 d/wk, plus DFO 40 mg/kg/d, 5 d/wk for ≥8 hrs/d. DFX dose could be increased to 30 and 40 mg/kg/d after Month 1 and 6, respectively. Patients achieving cardiac T2* ≥10 ms and a relative T2* increase of ≥10% from baseline (BL) any time after 6 months were switched to DFX monotherapy. Combination therapy was resumed if cardiac T2* fell to <10 ms with a relative decrease of ≥10% from previous T2* value. Dose adjustments were based on efficacy and safety parameters. Primary efficacy endpoint was change in geometric mean cardiac T2* at Month 12 divided by that at BL. A key secondary objective was the proportion of patients achieving T2* ≥10 ms and a ≥10% relative increase from BL after 6 and 12 months. Efficacy was analyzed for all evaluable patients in the full analysis set (FAS) who received ≥1 dose of study drug and had a BL and post-BL assessment; cardiac T2* is also reported for patients with T2* at BL and Month 12 (12-month completers).
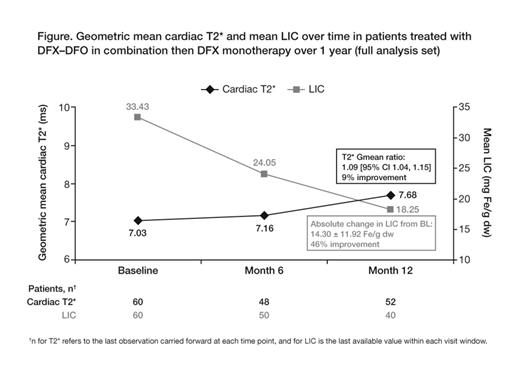
60 patients were enrolled (59 β-thalassemia major, 1 Diamond–Blackfan anemia; mean age 22.8 years; 46.7% male) with severe iron overload (geometric mean [Gmean] cardiac T2* 7.03 ms, mean LIC 33.4 ± 14.5 mg Fe/g dw, median serum ferritin 5551 ng/mL [range 1163, 11,317]). Overall, 20 patients discontinued; 5 consent withdrawals, 4 adverse events (AEs: pruritus, arthritis, abdominal pain, drug rash with eosinophilia and systemic symptoms), 4 abnormal test procedure results (all T2* <5 ms), 4 lost to follow-up, 2 administrative problems, 1 death (central nervous system infection, suspected relationship to DFO). Mean dose was DFX 29.6 ± 6.3, 7 d/wk, and DFO 37.4 ± 5.8 mg/kg/d, 5 d/wk. In the evaluable FAS (n=52, last observation carried forward) cardiac T2* increased 9% and LIC decreased 46% (Fig); serum ferritin levels decreased by 2174 ng/mL (–6138, 1570). Among 12-month completers (n=36), cardiac T2* increased from 7.24 at BL to 8.24 ms (14% improvement). In patients with BL LIC <30 and ≥30 mg Fe/g dw, cardiac T2* improvement was 17% (7.85 to 9.15 ms, n=16) and 6% (6.69 to 7.11 ms, n=36), respectively. Overall, 12.5 and 19.2% of patients achieved T2* ≥10 ms and ≥10% relative increase from BL at Month 6 and 12, respectively. Mean LVEF remained stable and no patient had cardiac failure. AEs with suspected relationship to study drug (≥5%) were abdominal pain, nausea (both 6.7%); increased blood creatinine, diarrhea, increased urine protein/creatinine ratio (all 5.0%). 1 patient had serum creatinine >33% increase from BL and >upper limit of normal at 2 consecutive visits.
Cardiac T2* improved during 12 months of treatment with DFX–DFO in patients with severe transfusional body iron burden. High BL LIC levels decreased considerably with DFX–DFO. Overall, as LIC decreased cardiac T2* increased, most notably after 6 months. The higher DFX dose permitted after Month 6 possibly influenced this trend. Cardiac T2* improvements were observed irrespective of BL LIC value, but were most marked in those with BL LIC <30 mg Fe/g dw, consistent with previous data showing that cardiac iron removal follows liver iron removal (Noetzli Blood 2008). Safety of DFX–DFO was consistent with established monotherapy profiles, with no unexpected findings. 2-year follow-up for HYPERION will evaluate the impact of longer-term DFX–DFO in combination on liver and cardiac iron removal.
Aydinok:Shire: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding, Speakers Bureau. Off Label Use: Deferasirox and deferoxamine are both indicated as a monotherapy for the treatment of chronic iron overload due to frequent blood transfusions. Patients with severe cardiac iron overload are at increased risk of heart failure and are often treated by off-label combination therapy for a limited time to facilitate rapid removal of iron from the heart, allowing patients to move to a lower-risk status. This abstract describes off-label use of the combination of deferasirox and deferoxamine to treat patients with severe transfusional cardiac iron overload. Kattamis:Novartis: Research Funding, Speakers Bureau; ApoPharma: Speakers Bureau. Cappellini:Genzyme: Honoraria; Novartis: Honoraria, Speakers Bureau. Perrotta:Novartis: Research Funding. Karakas:Novartis: Honoraria, Research Funding. Viprakasit:GPO, Thailand: Honoraria, Research Funding; Shire: Research Funding; Novartis: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding, Speakers Bureau. Habr:Novartis: Employment. Wegener:Novartis: Employment. Shen:Novartis: Employment. Porter, MD on behalf of the HYPERION investigators:Shire: Consultancy, Honoraria; Celgene: Consultancy; Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.