Abstract

History of major bleed during vitamin K-antagonist (VKA) therapy is an important predictor for future major bleeds. However, these patients do have an increased risk for thromboembolic events (TE) due to the underlying disease, and clinicians face a dilemma whether or not to continue VKA after major bleeding. We aim to present here long term follow-up (FU) of VKA patients after occurrence of a major bleeding complication, to increase knowledge of the clinical outcome and the consequences of (dis)continuation of VKA in this specific patient population.
Consecutive patients who presented with a major non-cranial bleed for which Prothrombin Complex Concentrate (PCC) was indicated, enrolled prospectively in a previous study comparing two dosing strategies for PCC (Khorsand et al. Haematologica 2012). The FU for the present study started from the day of discharge from hospital until death or until January 2012. Information on VKA management, occurrence of any recurrent major bleed or TE, mortality as well as the reason and date of mortality were collected retrospectively, from hospital charts, primary physicians and thrombosis services.
189 patients who survived a major non-cranial bleed were enrolled after a median hospital stay of 7 days [1-96]. Mean age was 74 years (sd 13), 50% were male, and median FU duration was 25 months [0-49].
A total of 91 major rebleeds occurred in 60 patients (32%) of which 5 were fatal. Furthermore, 16 TEs occurred in 16 patients (8%) of which 6 were fatal. Seventy nine patients (42%) died after a median FU of 5.9 months [0-44]. These patients were significantly older (mean age 79 versus 71, P<0.01) and suffered from more co-morbidities (mean Charlson Comorbidity Index 3.2 versus 2.4, P<0.01).
Our data describe a considerable impact of VKA-related major bleed. First, patients who presented with VKA-related major bleeding were old and had a high prevalence of comorbidity. During two years of FU, the risk of another major bleed was 32%, risk of TE was 8% and risk of mortality was 42%. This compares very unfavorable with the rates in an unselected population starting VKA therapy: Palareti et al (Lancet, 1996) reported the occurrence of major bleed in 0.8% and TE in 2.4% during 9 months of FU. Second, in the selection of patients in whom the treating physician decided to continue anticoagulation, the achieved quality of anticoagulation was substandard in 47% and only 21% continued VKA therapy successfully.
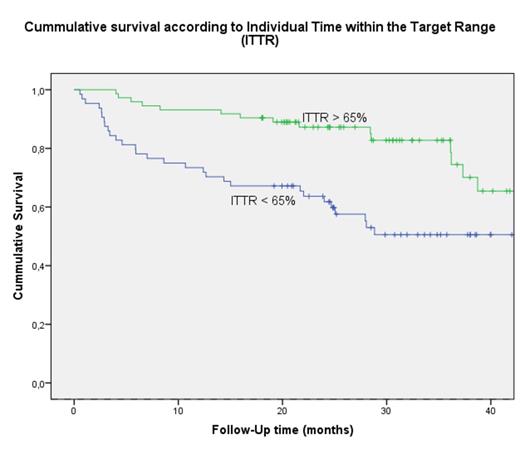
While there is no consensus on when and in whom resumption of VKA is indicated, clinicians seem to base their choice on patients health status (e.g. number of co-morbidities and malignancy) at the time of discharge, only restarting VKA in healthier patients. In our opinion, this is the explanation for the difference in survival which is depicted in figure 1. However, Witt et al. (Arch Intern Med, 2012) showed the same trend in survival after occurrence of VKA-associated gastrointestinal bleed despite corrections for multiple factors and therefore concluded a surprising benefit for overall survival when VKA is restarted.
In conclusion, our two-year FU, being the longest for this patient category, reports on the outcome of 189 consecutive patients after a VKA-associated major bleed. In this population 42% dies and 32% faces a recurrent major bleed, 8% a TE, while only 21% continues VKA therapy successfully.
Khorsand:Sanquin BV, Amsterdam: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract