Abstract

Post-transplant lymphoproliferative disease (PTLD) remains an important complication of solid organ transplantation. For B-cell PTLD, current first line therapies are Rituximab monotherapy (R-Mono) or R-CHOP. However, optimal selection of initial treatment is challenging due to concerns about the relative efficacy and toxicity of these modalities, and because of uncertainty about the prognostic value of baseline factors.
This retrospective study identified 72 biopsy-proven cases of PTLD, diagnosed between 2000 and 2012, from 4 UK centres. These included 34 liver, 32 renal and 6 cardiothoracic transplant recipients. The median age at histological diagnosis was 47 years (range 16 - 72 years) and 68% were male. The median time from transplant to diagnosis of PTLD was 93 months (range 2 – 302 months), with 83% of cases occurring after 1 year. Tumour histology included 14 polymorphic and 49 monomorphic lesions (including 34 diffuse large B-cell, 5 plasmablastic, 4 Hodgkin and 1 T-cell lymphomas) whilst in 9 cases the PTLD subtype was unspecified. EBV-association was noted in 39/72 (54%) and this was significantly related to disease presenting within a year of transplant (X2 p=0.004).
Initial therapy was R-Mono in 16/72 (22%) and R-CHOP in 34/72 (47%). Selection of R-CHOP versus R-Mono was significantly associated with stage ≥3 disease (odds ratio [OR] 6.7, p=0.01), onset more than 1 year after transplant (OR 7.3, p=0.03), lack of EBV association (OR 0.1, p=0.002) and monomorphic versus polymorphic histology (OR 14.0, p=0.004). In a multivariate logistic model, advanced stage (OR 11.0, p=0.06) and monomorphic histology (OR 8.5, p=0.03) retained significance.
Of patients who received R-Mono, 15/16 (94%) completed at least 4 infusions, with no treatment-related deaths. Of these, 4 patients subsequently received R-CHOP for consolidation of response (2 patients) or for relapsed / refractory disease (2 patients). Of those who received R-CHOP as initial therapy, 23/34 (68%) completed at least 6 cycles, with 4 treatment-related deaths.
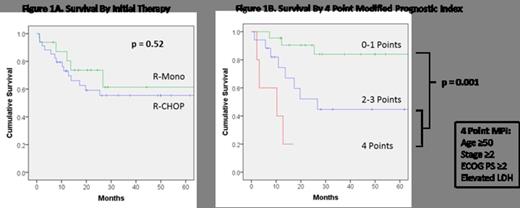
The overall response rate to R-Mono was 81% (10 CR [complete remission], 3 PR [partial remission] and 3 NR [no remission]), similar to that of R-CHOP at 74% (19 CR, 6 PR, 5 NR and 4 undetermined; X2 p=0.67). With a median follow-up of 38 months, survival outcomes for R-Mono and R-CHOP were 2 year Event-Free Survival of 62% and 54% (p=0.77), 2 year Progression-Free Survival of 67% and 58% (p=0.48) and 2 year Overall Survival (OS) of 74% and 59% (p=0.52; Figure 1A) respectively.
Amongst all study patients, significant baseline predictors of (inferior) OS were age ≥50 years (HR 2.9, p=0.006), stage ≥2 disease (HR 4.9, p=0.003), ECOG performance status ≥2 (HR 2.1, p=0.05), and elevated LDH (HR 2.2, p=0.08 borderline significance). Extra-nodal disease, histology, EBV-association and time from transplant were not predictive. In multivariate analysis, age>50 (HR 3.2, p=0.01) and advanced stage (HR 4.0, p=0.02) retained significance. Importantly, amongst those treated with R-Mono or R-CHOP, response to initial therapy was highly predictive of OS (overall response, HR 0.2, p<0.0001; complete response, HR 0.1, p<0.0001).
Applying a 4 point modified prognostic index comprised of age>50, stage ≥2 disease, ECOG performance status ≥2 and elevated LDH, patients treated with R-Mono or R-CHOP with low risk disease (<2 points) had significantly improved survival compared to those with high risk disease (≥2 points), with 2 year OS of 90% versus 43% (p=0.001, Figure 1B). Notably, comparison of outcomes for R-Mono versus R-CHOP within high risk or low risk groups revealed no significant differences in survival. However, there was a trend towards inferior response amongst patients with high risk disease treated with R-Mono compared to R-CHOP (CR rate 1/6 [17%] versus 9/16 [56%]; X2 p=0.16), which was not observed for low risk disease.
We report outcomes for R-Mono versus R-CHOP as initial therapy for PTLD arising after adult solid organ transplantation. Whilst R-CHOP is associated with greater toxicity, R-Mono may deliver inferior response rates in patients with high risk disease. Survival outcomes were not significantly different between therapies. Importantly, using a modified prognostic index we identify a subset of patients with high risk disease who exhibit very poor outcome, irrespective of initial treatment, for whom novel therapeutic strategies are urgently required.
Chaganti:Roche: Honoraria, Membership on an entity’s Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract