Abstract
G-CSF in combination with either cyclophosphamide (G-Cy) or plerixafor (G-P) safely mobilizes hematopoietic stem cells of adequate quality and quantity for auto-SCT in patients with multiple myeloma. Few studies have examined the impact of mobilization regimen on post-transplant disease control, particularly since the availability of plerixafor.
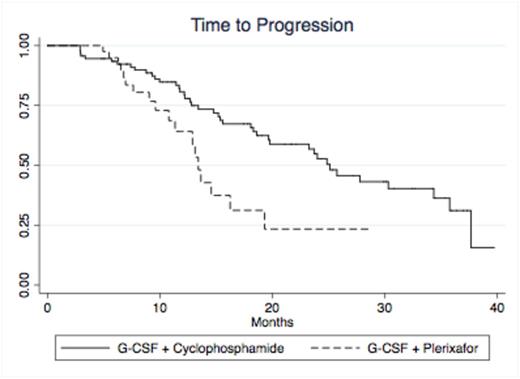
We retrospectively compared time-to-progression (TTP) after single melphalan-conditioned (140-200 mg/m2) auto-SCT in a single-institution cohort in which stem cells were mobilized with either cyclophosphamide 3 gm/m2 + G-CSF 10 mcg/kg/day x 10-14 days (G-Cy, n=93) or G-CSF 10 mcg/kg/day x 5-9 days with addition of plerixafor 240 mcg/kg/day starting on day 5 (G-P, n=55). Choice of mobilization regimen was according to physician preference. All patients had symptomatic multiple myeloma and had completed induction therapy with a regimen containing bortezomib and/or lenalidomide/thalidomide. Transplants conducted from January 2010 to May 2013, when commercially-available plerixafor was first used at our institution, were included in the analysis. Patients receiving tandem or salvage transplants and patients receiving investigational therapies in conjunction with transplant were excluded. Maintenance therapy was prescribed at the discretion of the treating physician. Progression was scored according to IMWG criteria.
The G-Cy and G-P cohorts were well matched for age, gender, and baseline multiple myeloma prognostic factors (see table). Cytogenetic data and beta-2-microglobulin measurements were not consistently available at baseline. Patients receiving G-P were more likely to have a >60 day interval between mobilization and transplant (P<0.0001) and >1 year interval between diagnosis and transplant (P=0.05). At time of transplant, hemoglobin was lower in the G-Cy group (P=0.0003), and platelet count was lower in the G-P group (P=0.035). Renal function at time of transplant was similar between the two groups. Patients in the G-P group were more likely to have received dose-reduced melphalan (<200 mg/m2) (p=0.03). The G-P group had higher ALC at day +15, which has been reported previously as a favorable prognostic factor for progression-free and overall survival. Median follow-up was 22 months. TTP was significantly different in the two groups (p=0.0095, log-rank test); median TTP was 25 months in the G-Cy group vs. 13 months in the G-P group (see figure). The difference in TTP remained significant when patients were excluded from the analysis who were transplanted more than 1 year after diagnosis (median TTP 26 vs. 13 months, P=0.0136 by log-rank test) or who were transplanted more than 60 days after mobilization (TTP 25 vs 13 months, P=0.0017 by log-rank test). Other variables that were significantly correlated with inferior TTP included IgA isotype (p=0.022) and receipt of >1 induction regimen (p=0.0077). In a univariate Cox regression, mobilization with G-P was associated with a hazard ratio of 2.1 (95% CI 1.2-3.9, p=0.011) for progression. In a multivariate Cox regression incorporating presence of IgA isotype, receipt of >1 induction regimen, mobilization regimen, age at transplant, time from diagnosis to transplant, time from mobilization to transplant, receipt of reduced melphalan dose, creatinine/hemoglobin/platelet count at time of transplant, ALC on day +15, and receipt of maintenance therapy, the association between G-P and inferior TTP was preserved (hazard ratio 2.8, 95% CI 1.3-6.0, p=0.007). The only other statistically significant variable was receipt of >1 induction regimen (hazard ratio 2.3, 95% CI 1.3-4.4, p=0.008). Receipt of maintenance therapy had a protective effect that approached statistical significance (hazard ratio 0.58, 95% CI 0.33-1.03, P=0.065). There were no significant differences in overall survival between the G-Cy and G-P groups.
GSTM1 polymorphism on Bu AUC
Hematopoietic stem cell mobilization with G-P was associated with significantly shorter post-transplant TTP compared to G-Cy in this single-institution cohort of multiple myeloma patients. We cannot conclude whether this association is due to effects of the mobilization regimen or confounding variables not accounted for in our analysis. This association warrants examination in a larger, multi-institution cohort.
Stadtmauer:Sanofi: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.