Abstract

About 70-80% of adult patients (pts) with acute myeloid leukemia (AML) achieve complete remission (CR); however, around a half of them experience a relapse. For the purpose of creating accurate decision-making process of post-consolidation strategy, stratification system using karyotype and recurrent gene mutations have been widely utilized. As is confirmed in childhood acute lymphocytic leukemia, however, the information of minimal residual disease (MRD) status would substantially improve the reliance of decision-making process of adult AML pts. Unfortunately, approximately a half of AML patients lack molecular targets suitable for MRD monitoring. The aims of this study are to evaluate the applicability of MRD detection using multiparametric flow cytometry (MPFC) and to estimate the impact of MRD measured with MPFC at the end of consolidation therapy in improving decision-making process.
We retrospectively studied 81 consecutive pts with newly diagnosed AML who received induction therapies and achieved CR in our institute between January 2007 and March 2013. Pts with acute promyelocytic leukemia were excluded. We routinely analyzed the bone marrow specimens with MPFC for the detection of leukemia-associated immunophenotypes (LAIPs) at diagnosis. Since April 2010, RT-PCR assay examined FLT3-ITD mutation in the same specimens. In pts who had traceable LAIPs, the relationships of the levels of MRD at the end of consolidation therapy with relapse free survival were analyzed. Positive MRD was defined as the detection of 0.2% and more LAIPs-positive cells with MPFC. We compared two patient groups: those with MRD at the end of consolidation (MRDp group) and those without (MRDn group). Relapse-free survival (RFS) was analyzed using the Kaplan-Meier method and the log-rank test was used for comparison between each group. A multivariate Cox regression analysis for RFS was fit to assess the effect of the followings: age at diagnosis (≥ vs. < 65 years old), the number of induction regimens required for achieving CR (≥ vs. < 2 times), cytogenetic risk groups of SWOG (unfavorable vs. favorable/intermediate).
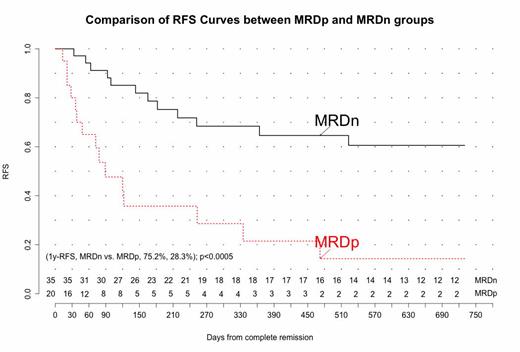
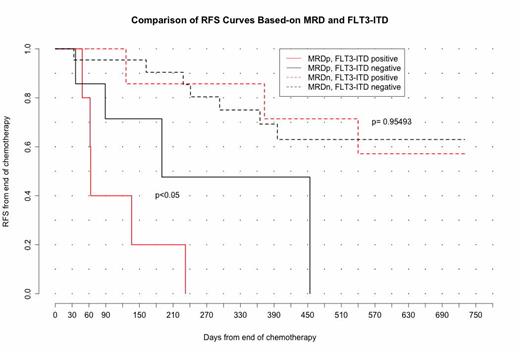
In 57 / 81 pts, MPFC could detect LAIPs in the bone marrow specimens at diagnosis (70.4% of all subjects; 15-82 years-old; follow-up time [median] 98-2211[517] days). FLT-ITD mutations were found in 13 pts, but not in 39 pts (the remaining 5 pts were not examined). The rate of detection of LAIPs with 6-color MPFC was significantly superior to 3-color MPFC (82.1% vs. 61.0%, p<0.05). Induction chemotherapies the pts received were anthracyclin-containing regimens, such as idarubicin and cytarabin (3+7), in 52 pts (91.2%), low-dose cytarabin-based regimen in 4 pts (7.0%) and azacitidine in 1 pt. (1.8%). The MRDp and the MRDn groups were comprised of 20 and 37 pts (35.1% and 64.9%) , respectively. One-year RFS of the MRDp group was significantly inferior to the MRDn group (28.3% vs. 75.2%; log-rank p<0.0005). In the multivariable analysis using the model above, MRD positivity at the end of consolidation remains a significant predictor (HR, 2.93, 95% CI 1.16-7.45, p<0.05). In addition, the 1-year RFS in the MRDp group with FLT-ITD was significantly shorter than that in the MRDp group without FLT3-ITD (0% vs. 47.6% with positive and negative FLT3-ITD, log-rank p<0.05). In the MRDn group, however, the negative impact of FLT3-ITD was not documented (85.7% vs. 69.3% with positive and negative FLT3-ITD, log-rank p=0.954).
Our retrospective study confirmed that LAIPs as MRD targets were applicable to the majority of pts with AML; MRD positivity measured with LAIPs was a promising predictor for early relapses at the end of consolidation, as was previously reported. When combined with FLT-ITD status, it might become a more sensitive prognostic factor.
Takahashi:celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract