Cardiac diastolic dysfunction plays a crucial role in the development of heart failure. The ratio of early diastolic mitral inflow velocity to early diastolic mitral annulus velocity (E/e') reflects left ventricular end-diastolic pressure and is used in the diagnosis of diastolic heart failure. Although cardiac complication is one of the most serious problems in hematopoietic stem cell transplantation (HSCT), the impact of diastolic dysfunction on clinical outcomes after allogeneic HSCT is unclear. Thus, we investigated the effects of diastolic dysfunction on HSCT using E/e'.
We retrospectively reviewed the records of 102 evaluable patients who underwent their first allogeneic HSCT at our hospital between November 2010 and July 2012, and investigated whether elevated E/e' would affect the clinical outcomes such as incidence of cardiac complications, overall survival (OS) and non-relapse mortality (NRM). Patients were classified into high- E/e' group if E/e' was ≥9 and classified into low- E/e' group if E/e' was <9. In multivariable analysis, the hazard ratio of E/e' was adjusted for variables with a P -value ≤ 0.2 in a univariable analysis, with stepwise deletions.
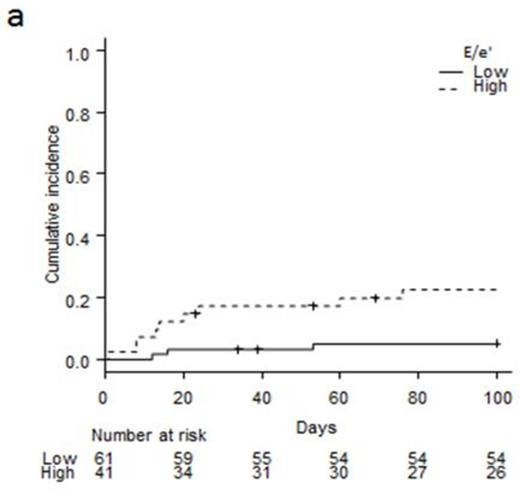
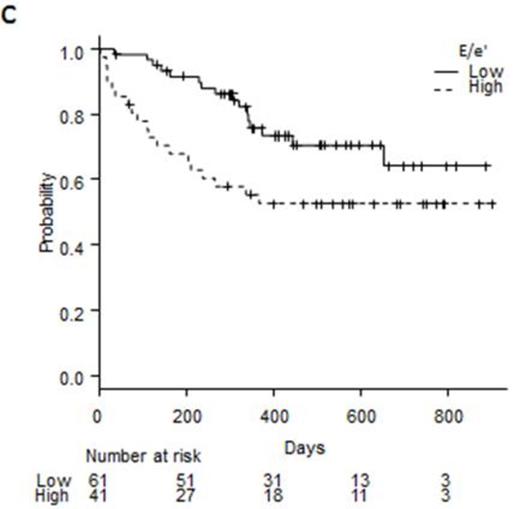
This study analyzed 58 males and 44 females with a median age of 47 years (range: 15-71). Forty one patients were classified into the high- E/e' group and 61 classified into the low- E/e' group. High- E/e' patients were older than low- E/e' patients (median: 57 years in E/e'-high vs. 41 years in E/e'-low, P=0.027). Reduced intensity regimen was more frequent in the high- E/e' group (39% vs. 16%, P=0.019) and there were also more men in the high- E/e' group compared with patients in the low- E/e' group (68% vs. 49%, P=0.07). Twelve patients developed cardiac complications during the first 100 days after HSCT (Day100) and its cumulative incidence was11.9%. Of them, 6 patients developed heart failure, 5 developed arrhythmia, and 1 developed both myocardial ischemia and heart failure. The cumulative incidence of cardiac complications at Day 100 was significantly higher in the high- E/e' group (22.4%) than that in the low- E/e' group (22.4% vs. 5%, P=0.0087, Figure 1a). Non-relapse death occurred in 17 patients within 1 year after HSCT. Nine patients died of infection, 3 died of hemorrhage, 2 died of graft-versus-host disease, 1 died of heart failure, 1 died of thrombotic microangiopathy, and 1 died of veno-occlusive disease/sinusoidal obstruction disease. NRM was higher in the high- E/e' group than in the low- E/e' group (28.8% vs. 10.5% at 1year, P=0.0165, Figure 1b). A multivariate analysis revealed that high- E/e' and high disease status were significant risk factors for high NRM (other co-variates were HLA compatibility and HCT-CI). Conversely, the relapse rate did not significantly differ in both groups (23% in the high- E/e' vs. 17% in the low- E/e' at 1 year, P=0.44). The OS was significantly poorer in the high- E/e' group than in the low- E/e' group (55.2% vs. 75.6% at 1 year, P=0.0085, Figure 1c). On multivariate analysis, E/e', disease status, and donor source were defined as independent prognostic factors for OS (other co-variates were HLA compatibility, preparative regimens, disease status, and QTc).
Diastolic dysfunction is associated with iron overload, anemia, diabetes, kidney disease, heart failure, cardiomyopathy, aging, and hypertension. Thus, pre-transplat E/e' value might reflect the potential risk of these diseases in transplant candidates and be associated with poor outcomes. Our results suggest that pre-transplant E/e' value would be an early predictor of cardiac complications and survival after HSCT.
Figure 1: Cardiac complication (a), non-relapse mortality (b), and overall survival (c) in high- E/e' group and low- E/e' group.
Figure 1: Cardiac complication (a), non-relapse mortality (b), and overall survival (c) in high- E/e' group and low- E/e' group.
No relevant conflicts of interest to declare.