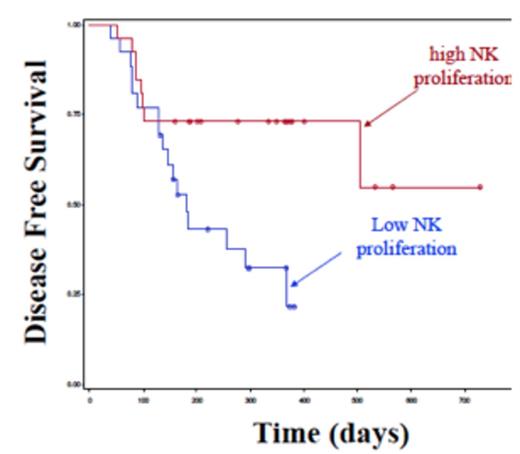
Compared to traditional chemotherapy, allogeneic hematopoietic cell transplantation (allo-HCT) has the potential of triggering graft vs. leukemia (GVL) reactions that make this procedure uniquely curative. Despite this, relapse remains the most common cause of treatment failure. Early after allo-HCT the donor immune system reconstitutes within the host and natural killer (NK) cells are the earliest lymphocyte population to recover. Previous studies by us and other investigators have linked rapid lymphocyte recovery and/or high NK cell numbers early after transplant with less relapse. Mechanistically, the reasons for this are unknown. We hypothesized that NK cell proliferation would be associated with allo-HCT outcomes. In a large data set with short-term follow-up we compared stem cell source to NK cell proliferation at Day 28 after transplantation (using Ki67+ staining). In patients undergoing autologous (n=117), sibling (n=57), single umbilical cord blood (sUCB) (n=62) or double umbilical cord blood (dUCB) (n=50) transplantation there were significant differences in the median NK cell proliferation (2.1%, 3.3%, 3.8%, and 19.2%, respectively, p<0.0001). These results suggest that NK cell proliferation is increased when patients are transplanted with stem cell sources that have an increased number of HLA mismatches (dUCB). We next examined factors extrinsic to the NK cells to determine whether differences in the four patient groups were due to these factors. Regulatory T cells (Tregs) are known to negatively regulate the proliferation and activation of a variety of cell types, including NK cells. We utilized the percentage and absolute number of Tregs (defined as CD4+CD25highFoxP3+CD127low) at Day 28 (available for a subset of the above patient samples) and correlated it with the percentage of proliferating NK cells at Day 28 after allogeneic transplant (n=212). The median percentage of Tregs within the lymphocyte fraction was 1.49%. In patients with higher than 1.49% Tregs, the mean NK cell proliferation was 10.8% +/-16.4. In contrast, patients with lower than 1.49% Tregs had a mean NK cell proliferation of 21.2% +/-24.3 (p=0.0004). A nearly identical trend was observed for the absolute numbers of Tregs, suggesting that Tregs may play an extrinsic role in NK cell proliferation after allo-HCT. To further address differences in lymphocyte proliferation and clinical outcomes, we used Ki67 staining to assess T cell (CD4+ and CD8+) and NK cell (CD3-CD56+) proliferation at Day 28 in a different subset of patients undergoing dUCB transplant with acute leukemia or MDS (80%) or other malignant disorders using either myeloablative (42%) or reduced intensity conditioning (58%) and a median of one year follow-up (n=53). There was no association of transplant outcomes with T cell (CD4 or CD8) proliferation. In the NK cell compartment there was a wide range in the percentage of proliferating NK cells (0-86%), with a median of 20%. Patients were segregated into high (>20%) and low (<20%) NK cell proliferating groups and assessed for cytokine levels and transplant outcomes. At Day 28 soluble IL15 levels were not different between high and low NK cell proliferating patients. There was no significant association between NK cell proliferation and the probability or time to neutrophil recovery (p=0.15) or treatment related mortality (p=0.88). Excluding the 14 patients who developed aGVHD prior to day of NK cell assessment (Day 28), the high NK proliferating group had a trend toward a higher cumulative incidence of aGVHD (46% vs. 25%, p=0.17). Using multivariable analysis to control for a variety of patient and disease-associated variables, patients with high NK cell proliferation had significantly better disease-free survival (HR=0.29, 95%CI=0.12-0.71, p=0.01) (Figure 1). Strikingly, patients with high NK cell proliferation were 4-times less likely to relapse (HR=0.24, 95%CI=0.08-0.77, p=0.02). Collectively, these studies show that early NK cell proliferation is associated with superior outcomes after dUCB transplantation, due to reduced relapse, and that this is partly modulated by Tregs. Prospective strategies to increase NK cell proliferation may be of therapeutic benefit to improve transplant outcomes. Close modal
Figure 1
Disease Free Survival for patients undergoing dUCB transplant (n=53) based on low (blue) vs high (red) NK cell proliferation at Day 28 post transplant.
Figure 1
Disease Free Survival for patients undergoing dUCB transplant (n=53) based on low (blue) vs high (red) NK cell proliferation at Day 28 post transplant.
Disclosures:
Wagner:Novartis: Research Funding. Miller:Coronado Biosciences: Scientific Advisory Board Other.
© 2013 by The American Society of Hematology
2013