Abstract
The International Prognostic Scoring System (IPSS) was recently revised (IPSS-R). IPSS-R was developed using a large cohort of patients received supportive therapy, so we validated the new prognostic score system in Korean patients. IPSS-R emphasizes initial cytogenetic abnormalities, but the risk of clonal evolution is not well identified in follow up of MDS patients.
Data of 88 MDS patients were collected retrospectively and verified by chart review. And we also collected cytogenetic analysis results performed with bone marrow study.
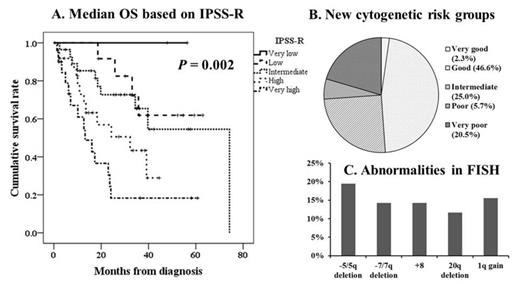
By IPSS-R cytogenetic scoring system, 2 (2.3%), 41 (46.6%), 22 (25.0%), 5 (5.7%), and 18 (20.5%) patients were classified as very good, good, intermediate, poor, and very poor, respectively. According IPSS, 5 (5.7%), 50 (56.8%), 19 (21.6%), and 14 (15.9%) patients were classified as low, intermediate-1, intermediate-2, and high, respectively. According to IPSS-R, 2 (2.3%), 13 (14.8%), 28 (31.8%), 25(28.4%), and 20 (22.7%) patients were reclassified as very low, low, intermediate, high, and very high, respectively. Median 3 years overall survival of patients intermediate, high and very high IPSS-R are 36 (95%CI 34-39), 32 (95%CI 8 – 56), and 13 (95%CI 6-21), respectively (P = 0.004). Clonal evolutions were occurred in 22 patients and they were classified by IPSS-R cytogenetic scoring system: 11 (50.0%) good, 8 (36.4%) intermediate, 1 (4.5%) poor, 2 (9.1%) very poor. Prior clonal evolution was considered as except concurrent occurrence of clonal evolution and acute myeloid leukemia (AML) transformation. These 17 patients have significant correlation with AML transformation (P = 0.010) and mortality (P = 0.021).
IPSS-R gives more refined prognostic discrimination and can be applicable in Korean MDS patients. In addition, the clonal evolution occurring during follow up should be considered as a risk factor of AML transformation and mortality.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.