Abstract
Allogeneic stem cell transplantation (allo-SCT) remains the main therapeutic option for patients with high-risk hematologic malignancies, albeit with the requirement of a properly matched and timely available donor. Dual-unit umbilical cord blood transplantation (dUCBT) has become an alternative modality, which offers immediate access to allo-SCT for most adult patients who lack an appropriate volunteer donor.
We retrospectively analyzed the outcomes of consecutive dUCBT procedures that were undertaken by our center over a seven-year period, with focus on factors affecting engraftment and survival.
Between 2006 and 2013, 40 patients underwent dUCBT at a median age of 37 years (range, 16-60) for various hematologic malignancies (acute myeloid leukemia: 22, myelodysplastic syndrome: 5, chronic myelogenous leukemia: 2, acute lymphoblastic leukemia: 6, mixed-phenotype acute leukemia: 2, plasmacytoid dendritic cell neoplasm: 1, hepatosplenic T cell lymphoma: 1, chronic lymphocytic leukemia: 1). The majority of patients (73.7%) had advanced or intermediate-phase disease at the time of transplantation, with a median time from diagnosis to transplant of 17.7 months (range:3.1-92.3). Recipient body weight ranged from 48 to 110 kg (median, 73). The conditioning regimen was myeloablative in 33 (82.5%) patients (busulfan-based in 22, and total body irradiation-based in 11 cases). Antithymocyte globulin was not administered during conditioning, with the exception of one case.
Most units (55/80, 68.75%) were 4/6 antigen matched to recipient at HLA-A, -B, and -DRB1 loci, and the remaining were 5/6 matched. By retrospective high-resolution typing for class I HLA alleles, histocompatibility was demoted in 62.3% of units. By additional allele-level typing at HLA-C and -DQB1 loci, the degree of compatibility varied from 8/10 to 3/10, with 80.5% of the units being ≤6/10 matched to the patient. The median dose of cryopreserved total nucleated cells (TNC) per unit was 2.53 x 107/kg (range, 1.09-5.66). At infusion, patients received in total a median of 4.55 x 107 TNC/kg (range, 2.65-9.3) and 1.7 x 105 CD34+ cells/kg (range, 0.54-5.14) from both units.
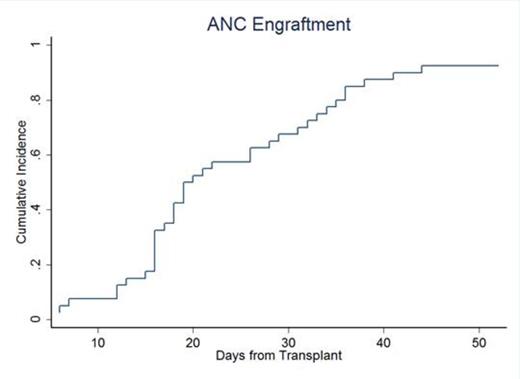
Cumulative Incidence curve of neutrophil (ANC>500/uL) engraftment.
Cumulative Incidence curve of neutrophil (ANC>500/uL) engraftment.
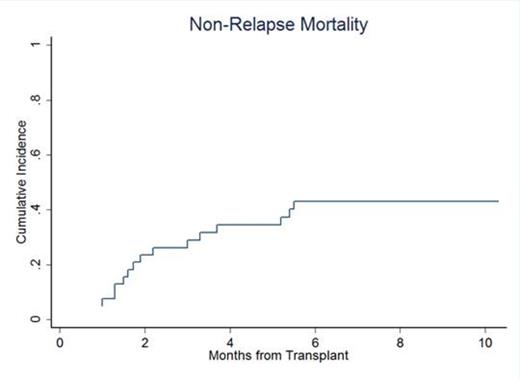
Cumulative Incidence curve of non-relapse mortality.
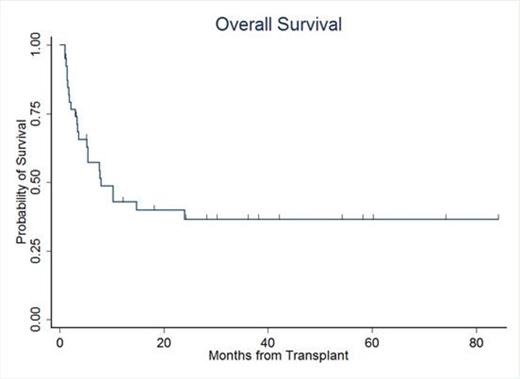
Overall Survival (Kaplan-Meier curve).
In conclusion, dUCBT can lead to stable donor engraftment even across multiple HLA disparities and can overcome the barrier of cell dose. Despite considerable early mortality, dUCBT offers the possibility of long-term survival in about one third of adult patients with poor-prognosis hematologic malignancies, for whom allo-SCT would not be otherwise feasible.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.