Abstract

The transportation of haemopoietic progenitor cells (HPC) from collection centre to transplant centre is a critical, but often overlooked process during allogeneic transplantation using voluntary unrelated donors (VUD). The policies of international donor registries support the rapid retrieval and infusion of HPC. However transplant centres are often challenged by transit times in excess of 24h when retrieving HPC from intercontinental collection centres. This single institutional retrospective study aimed to investigate if a prolonged transit time between collection and transplant centre impacted upon the rate of engraftment and overall survival of recipients of HPC collected from VUDs.
A retrospective analysis of outcomes following an initial allogeneic transplant performed at our institution between 1987 and 2013 was conducted using institutional databases. The time to neutrophil and platelet engraftment and overall survival was compared between recipients of VUD transplants with HPC retrieved from collection centres located overseas (transit time of > 24h) (n = 241; BM n = 50, PBPC n = 191), recipients of unrelated donor transplants with HPC retrieved from collection centres within Australia (transit time of <8h) (n = 334; BM n = 112, PBPC n = 222) and recipients of related HPC collected at the transplant centre (n = 807; BM n = 320, PBSC n = 487). All HPC retrieved from local and intercontinental VUD collection centres were transported in rigid coolers containing refrigerated gel packs prior to 2003 or isothermal cooling inserts post 2003. The temperature was monitored and maintained by the courier at between 2 and 8oC.
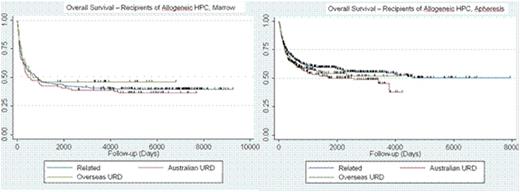
There was no significant difference in the days to neutrophil and platelet recovery (Table 1) between recipients of a VUD allogeneic transplant with HPC retrieved from a local collection centre compared with those recipients whose HPC was retrieved from an international collection centre. Retrieval and infusion of HPC from local collection centres is generally completed within 8h from collection whereas the interval from collection to infusion may vary between 24 to 90h when HPC are retrieved from intercontinental collection centres. Furthermore there was no significant difference in overall survival (Figure 1) of recipients of related donor allogeneic transplants performed without transportation of HPC and recipients of VUD allogeneic transplants whose HPC were retrieved from either a local collection centre or an intercontinental collection centre (Figure 1).
Neutrophil and platelet engraftment post VUD allogeneic transplantation
| . | Days to Neutrophil Count of 0.5 x 109/L (median) . | Days to Platelet Count of 20 x 109/L (median) . |
|---|---|---|
| Unrelated BM (transit < 8h) | 17 | 27 |
| Unrelated BM (transit > 24h) | 17 | 26 |
| Unrelated PBPC (transit < 8h) | 16 | 19 |
| Unrelated PBPC (transit > 24h) | 16 | 19 |
| . | Days to Neutrophil Count of 0.5 x 109/L (median) . | Days to Platelet Count of 20 x 109/L (median) . |
|---|---|---|
| Unrelated BM (transit < 8h) | 17 | 27 |
| Unrelated BM (transit > 24h) | 17 | 26 |
| Unrelated PBPC (transit < 8h) | 16 | 19 |
| Unrelated PBPC (transit > 24h) | 16 | 19 |
Overall survival of recipients following allogeneic related or VUD transplantation using HPC (BM or PBPC) retrieved from either a local or international donor between 1987 and 2013
Overall survival of recipients following allogeneic related or VUD transplantation using HPC (BM or PBPC) retrieved from either a local or international donor between 1987 and 2013
Our study demonstrated no adverse effect on neutrophil and platelet recovery, or overall survival resulting from retrieval of HPC (BM and PBPC) from collection centres with transit times in excess of 24h and with some international retrievals requiring up to 90h transit times. A previous study had reported higher mortality rates and delayed platelet engraftment following HLA matched unrelated donor BM transplants facilitated by the National Marrow Donor Program with an interval of greater than 24h between collection and infusion (Lazarus et. al, Biol Blood Marrow Transplant 15: 589-596, 2009). At our centre HPC (BM and PBPC) are retrieved by trained couriers that monitor and maintain the temperature between 2 and 8oC. This is in contrast to NMDP recommendations that BM is transported at ambient temperature. Our data suggest that all HPC should be refrigerated to between 2 and 8oC and the temperature monitored during transportation. In addition, the courier should be trained to re-establish the optimal temperature for transportation if the temperature deviates from the recommended range.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract