Key Points
Endothelial S1PR2 plays a critical role in the induction of vascular permeability and vascular inflammation during endotoxemia.
S1PR2 could be a novel therapeutic target to promote vascular integrity in inflammatory vascular disorders.
Abstract
The endothelium, as the interface between blood and all tissues, plays a critical role in inflammation. Sphingosine-1-phosphate (S1P) is a bioactive sphingolipid, highly abundant in plasma, that potently regulates endothelial responses through interaction with its receptors (S1PRs). Here, we studied the role of S1PR2 in the regulation of the proadhesion and proinflammatory phenotype of the endothelium. By using genetic approaches and a S1PR2-specific antagonist (JTE013), we found that S1PR2 plays a key role in the permeability and inflammatory responses of the vascular endothelium during endotoxemia. Experiments with bone marrow chimeras (S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+) indicate the critical role of S1PR2 in the stromal compartment, in the regulation of vascular permeability and vascular inflammation. In vitro, JTE013 potently inhibited tumor necrosis factor α–induced endothelial inflammation. Finally, we provide detailed mechanisms on the downstream signaling of S1PR2 in vascular inflammation that include the activation of the stress-activated protein kinase pathway that, together with the Rho-kinase nuclear factor kappa B pathway (NF-kB), are required for S1PR2-mediated endothelial inflammatory responses. Taken together, our data indicate that S1PR2 is a key regulator of the proinflammatory phenotype of the endothelium and identify S1PR2 as a novel therapeutic target for vascular disorders.
Introduction
Sphingosine-1-phosphate (S1P), a bioactive sphingolipid present at high levels (within the range of several hundred nanomolar) in plasma and lymph, is generated from the metabolism of sphingomyelin through the actions of sphingomyelinase, ceramidase, and sphingosine kinase (SPHK).1 Although platelets store high amounts of S1P, it has recently been shown that the main sources of plasma S1P are erythrocytes2 and endothelial cells.3 Both cell types exhibit high levels of SPHK activity. S1P mediates multiple cellular responses in many different cell types by activating the endothelial differentiation gene family of G protein-coupled receptors renamed S1PR1-5.4,5 Since endothelial cells express S1PR1, S1PR2, and S1PR3, plasma S1P can bind and activate these receptors in the endothelium. In addition, the fact that endothelial cells are one of the main sources of plasma S1P suggests that cell-autonomous S1P signaling may play a role in vascular homeostasis. The role of S1P in vascular development is well illustrated by SphK-1 and -2 null mice, which lack S1P and exhibit severely disturbed angiogenesis resulting in embryonic lethality6 and by S1pr1 null mice, which exhibit a defect in vascular maturation.7 In adult mice and humans, S1PR1 is critical for the regulation of vascular permeability8,9 and lymphocyte trafficking.10 In fact, fingolimod, recently approved by the US Food and Drug Administration, is a potent immunosuppressant that targets S1PR1. In contrast to S1PR1, S1PR2 is not required for embryonic vascular development, and S1pr2−/− mice are viable and develop normally.11-14
S1PRs activate different intracellular signaling pathways and differentially regulate endothelial cell function. S1PR1 couples to Gi and activates the phosphatidylinositol 3-kinase (PI3K) pathway,15 Rac, cortical actin assembly, and cell migration.16 This pathway is essential for vascular stabilization7 and inhibition of vascular permeability.8,9 In sharp contrast, we recently found that S1PR2 antagonizes S1PR1-Gi-PI3K signaling in the endothelium through activation of the G12/13-Rho-Rho kinase (ROCK)-PTEN pathway.17,18 Indeed, the Rho-ROCK-PTEN pathway is critical for the inhibition of endothelial cell migration and the induction of vascular permeability by S1PR2.17 These studies indicate that the balance between S1PR1 and S1PR2 signaling in a specific vascular bed will determine the endothelial responses to S1P. Therefore, a better understanding of how S1PR signaling is regulated in health and disease should provide an important foundation for developing novel therapies for vascular disorders.
During inflammation, the endothelium becomes activated with an increase in endothelial permeability and acquires a proadhesion and procoagulant phenotype that promotes the innate immune response.19,20 Sustained activation results in endothelial dysfunction, which plays a critical role in the pathophysiology of sepsis, diabetic vasculopathy, atherosclerosis, ischemia-reperfusion injury, and allograft rejection.19-21
Our previous work demonstrates that S1PRs play a critical role in the regulation of the permeability responses of the endothelium.8,17 In this study, we investigated the role of S1PR2 in acute vascular inflammation. We characterize S1PR2 as a novel regulator of vascular inflammation that is critical for the induction of the permeability and proadhesion phenotypes of the endothelium during endotoxemia. Our findings emphasize the critical role of S1PR2 in endothelial responses to injury and highlight the potential utility of pharmacologic targeting of S1PR2 in the therapy of vascular inflammatory disorders.
Materials and methods
Materials and methods are described in detail in the supplemental Data. All animal studies were approved by the Beth Israel Deaconess Medical Center Institutional Animal Care and Use Committee.
Results
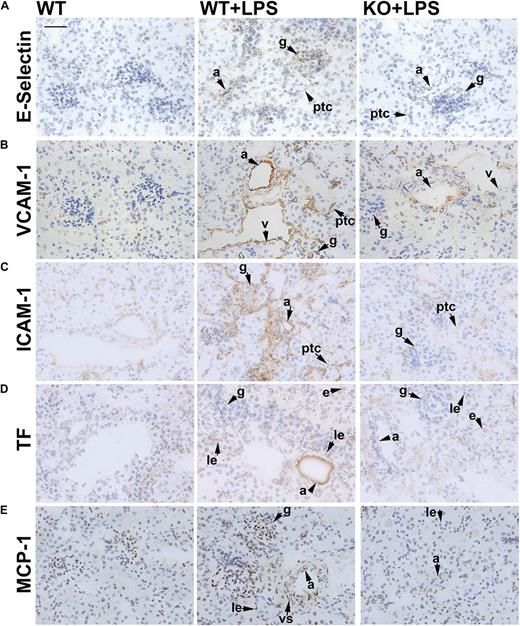
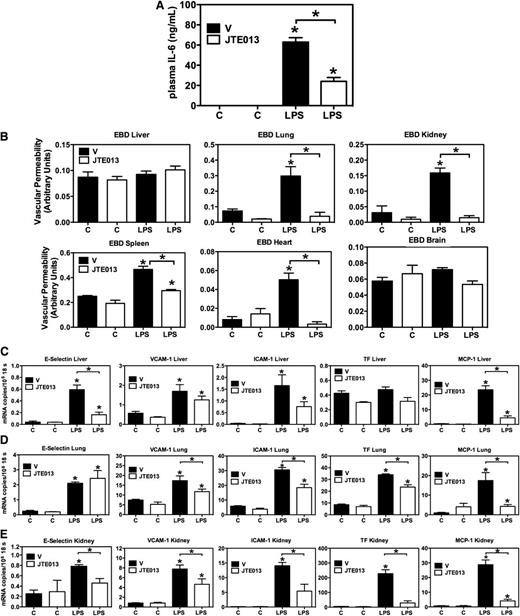
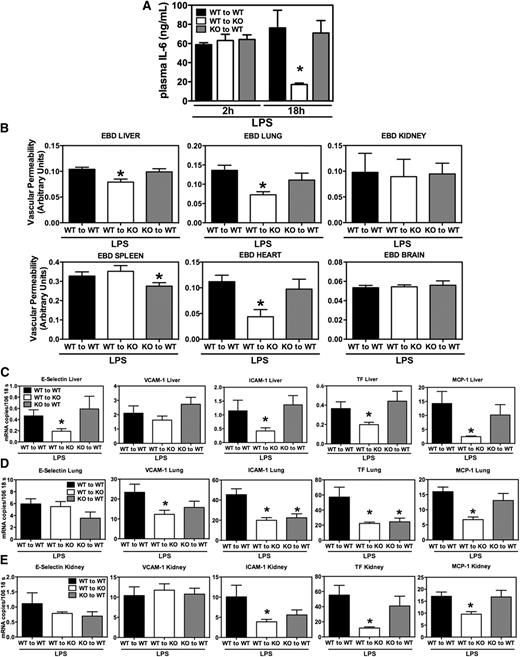
S1PR2 deficiency results in lower expression of inflammatory and coagulation mediators during endotoxemia
To study the role of S1PR2 in vascular inflammation, we used a mouse model of severe, sublethal lipopolysaccharide (LPS) challenge. S1pr2+/+ and S1pr2−/− mice were administered LPS intraperitoneally to induce endotoxemia and systemic inflammation. Plasma was collected 2, 6, and 18 hours after LPS injection. Lack of S1PR2 had no effect on LPS-mediated induction of plasma levels of the inflammatory cytokine interleukin-6 (IL-6) at early time points (Figure 1A). However, cytokine levels fell more rapidly in S1pr2−/− mice compared with their wild-type (WT) littermates (12.9 ± 2.5 and 47.2 ± 8.6 ng/mL in S1pr2−/− and S1pr2+/+ mice, respectively, at 18 hours). Interestingly, lack of S1PR2 blunted the induction of vascular permeability by LPS in the lung, kidney, spleen, and heart vascular beds, as assessed by the Evans blue dye extravasation assay (6 hours after LPS injection; Figure 1B).
S1pr2 null mice display decreased inflammation during endotoxemia. (A) Reduced late-stage inflammation in S1pr2−/− mice (knockout [KO]) compared with WT mice documented by plasma IL-6 levels at various time points following LPS administration. Data are mean ± standard error of the mean (SEM) (n = 4 to 14). (B) LPS-induced vascular permeability is abrogated in mice lacking S1PR2. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by the Evans blue dye extravasation (EBD) assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between WT and S1pr2−/− mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in S1pr2+/+ (WT) and S1pr2−/− (KO) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time polymerase chain reaction (PCR) analyses (mRNA copy number per 106 copies of 18s ribosomal RNA [rRNA]) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between WT and S1pr2−/− mice.
S1pr2 null mice display decreased inflammation during endotoxemia. (A) Reduced late-stage inflammation in S1pr2−/− mice (knockout [KO]) compared with WT mice documented by plasma IL-6 levels at various time points following LPS administration. Data are mean ± standard error of the mean (SEM) (n = 4 to 14). (B) LPS-induced vascular permeability is abrogated in mice lacking S1PR2. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by the Evans blue dye extravasation (EBD) assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between WT and S1pr2−/− mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in S1pr2+/+ (WT) and S1pr2−/− (KO) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time polymerase chain reaction (PCR) analyses (mRNA copy number per 106 copies of 18s ribosomal RNA [rRNA]) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between WT and S1pr2−/− mice.
Peripheral blood cell counts were also determined under basal conditions 4 hours and 18 hours after LPS injection in WT and S1PR2 null mice (supplemental Figure 1). In WT mice, total leukocyte, neutrophil, monocyte, and lymphocyte counts decreased 4 hours after LPS injection because of the recruitment of leukocytes to sites of inflammation. Eighteen hours after LPS injection, peripheral neutrophil and monocyte numbers increased because of mobilization of cells from the bone marrow, while lymphocyte numbers remained low. In S1pr2−/− mice, no differences from S1pr2+/+ mice were observed under basal conditions and 4 hours after LPS injection. However, 18 hours after LPS injection, total leukocyte, neutrophil, and monocyte counts were lower in S1pr2 null mice compared with WT mice, consistent with the faster resolution of the inflammatory response observed in mice lacking S1PR2. Flow cytometry analysis of minced and digested organs showed that the composition of the leukocyte infiltrate was altered 16 hours post-LPS injection, with significant increases in neutrophils in liver, lung, and kidney in both S1pr2+/+ and S1pr2−/− animals (supplemental Figure 2A). No differences in F4/80+CD11b+ macrophages/monocytes were observed between S1pr2+/+ and S1pr2−/− livers and kidneys after LPS injection, while lungs of WT animals treated with LPS displayed a decrease in F4/80+CD11b+CD11c− macrophages/monocytes (supplemental Figure 2B). Altogether, these data indicate that circulating leukocytes from both WT and S1pr2 null mice similarly respond to the LPS challenge by infiltrating into the tissues. However, rebound neutrophilia and monocytosis in peripheral blood were significantly decreased in S1pr2−/− mice 18 hours after LPS injection.
Intraperitoneal injection of LPS resulted in increased mRNA levels of proinflammatory (E-selectin, vascular cell adhesion molecule 1 [VCAM-1], intercellular adhesion molecule 1 [ICAM-1], and monocyte chemotactic protein 1 [MCP-1]) and procoagulation (tissue factor [TF]) mediators in several organs, including the liver, lung, and kidney, 18 hours after LPS injection (Figure 1C-E). Compared with WT mice, S1pr2 null mice exhibited significantly lower messenger RNA (mRNA) levels of adhesion molecules and coagulation and inflammatory markers. In the liver, knockout of S1pr2 significantly attenuated the effect of endotoxemia on mRNA expression of E-selectin, VCAM-1, and MCP-1 (66.1%, 40.9%, and 62.5% inhibition, respectively; Figure 1C). In the lungs, LPS-mediated induction of VCAM-1, ICAM-1, TF, and MCP-1 expression was significantly decreased in S1pr2−/− compared with WT mice (63.6%, 55.4%, 42.1%, and 79.6% inhibition, respectively; Figure 1D). In the kidney, lack of S1PR2 resulted in decreased mRNA levels of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 compared with their WT littermates (45.6%, 56.2%, 61.6%, 59.5%, and 76.2% inhibition, respectively; Figure 1E). Altogether, these data indicate that lack of S1PR2 results in a dramatic decrease in vascular permeability, a faster drop in cytokine levels, and lower expression of adhesion molecules and proinflammatory and procoagulant mediators in several organs during systemic inflammation.
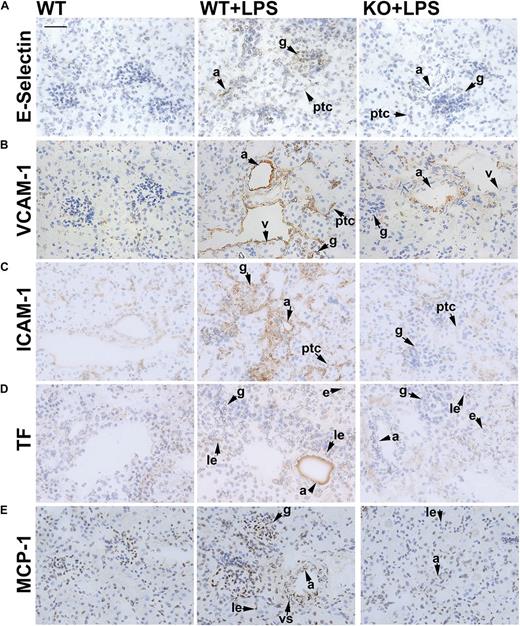
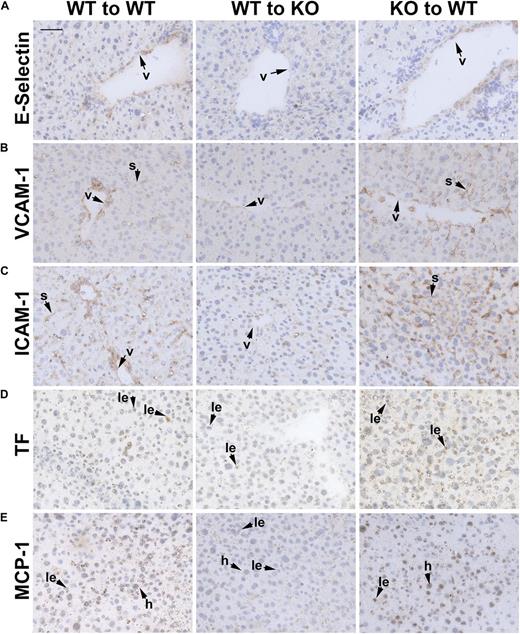
Immunohistochemical analysis of these proinflammatory markers revealed similar findings. In WT kidneys, upregulation of adhesion molecules was observed 18 hours after LPS injection (Figure 2A-C). More specifically, we observed E-selectin immunoreactivity in arteriolar, glomerular, and peritubular capillary endothelium. However, in kidneys from LPS-treated S1pr2−/− mice, levels of E-selectin were much lower than in LPS-treated WT mice (Figure 2A). Likewise, VCAM-1 expression was induced in arterioles, glomeruli, peritubular capillaries, and venules in WT kidneys after LPS treatment, while much lower VCAM-1 immunoreactivity was found in S1pr2−/− kidneys, especially in the peritubular capillaries and glomeruli (Figure 2B). Additionally, ICAM-1 was upregulated in arterioles, glomeruli, peritubular capillaries, and venules in WT kidneys 18 hours after LPS injection. However, much less intense ICAM-1 immunoreactivity was found in glomeruli and peritubular capillaries of S1pr2−/− kidneys (Figure 2C). Consistent with previous reports, increased TF immunoreactivity was observed in tubular epithelial cells,22,23 infiltrating leukocytes, and arteriolar endothelium in WT kidneys 18 hours after LPS injection; however, much lower TF staining was detected in S1pr2−/− kidneys (Figure 2D). MCP-1 immunoreactivity was detected in glomeruli, infiltrating leukocytes, and endothelial and vascular smooth muscle cells from arterioles upon LPS injection in WT mice (Figure 2E). In contrast, in S1pr2−/− kidneys, MCP-1 immunoreactivity was markedly reduced in all these cellular compartments.
S1pr2 null mice exhibit less vascular inflammation in the kidney during endotoxemia. Expression of adhesion molecules and procoagulant and proinflammatory markers in kidneys from control WT, LPS-treated WT (WT + LPS), and LPS-treated S1pr2−/− (KO + LPS) mice 18 hours after administration of vehicle or LPS. Immunostaining for (A) E-selectin, (B) VCAM-1, (C) ICAM-1, (D) TF, and (E) MCP-1. Scale bar, 50 μm. Representative fields from 3 to 5 mice are shown. Images were captured with the Axio Imager A1 microscope, using AxioCam MRc camera and the AxioVision 4.8 program (Carl Zeiss Inc.) (original magnification ×40). a, arteriolar endothelium; e, epithelial cell; g, glomerulus; le, leukocyte; ptc, peritubular capillary; v, venule; vs, vascular smooth muscle cell.
S1pr2 null mice exhibit less vascular inflammation in the kidney during endotoxemia. Expression of adhesion molecules and procoagulant and proinflammatory markers in kidneys from control WT, LPS-treated WT (WT + LPS), and LPS-treated S1pr2−/− (KO + LPS) mice 18 hours after administration of vehicle or LPS. Immunostaining for (A) E-selectin, (B) VCAM-1, (C) ICAM-1, (D) TF, and (E) MCP-1. Scale bar, 50 μm. Representative fields from 3 to 5 mice are shown. Images were captured with the Axio Imager A1 microscope, using AxioCam MRc camera and the AxioVision 4.8 program (Carl Zeiss Inc.) (original magnification ×40). a, arteriolar endothelium; e, epithelial cell; g, glomerulus; le, leukocyte; ptc, peritubular capillary; v, venule; vs, vascular smooth muscle cell.
In the liver, 18 hours after LPS injection in WT mice, E-selectin immunoreactivity was found mainly in venules, while VCAM-1 and ICAM-1 were detected in venules and liver sinusoids (supplemental Figure 3). Immunoreactivity for these three markers was markedly reduced in S1pr2−/− livers compared with WT livers. Consistent with previous findings,23 TF-positive cells in livers from LPS-treated WT mice were mainly leukocytes, and immunoreactivity was reduced in S1pr2−/− compared with WT mice. MCP-1 immunoreactivity was increased in hepatocytes, some venules, and infiltrating leukocytes in WT mice after LPS treatment, while much lower levels were detected in S1pr2−/− mice. Altogether, our immunohistochemical data, consistent with our mRNA findings, indicate that the levels of proinflammatory and procoagulant markers in the vascular endothelium, parenchymal cells, and leukocytes are significantly lower in S1pr2 null mice 18 hours after LPS injection.
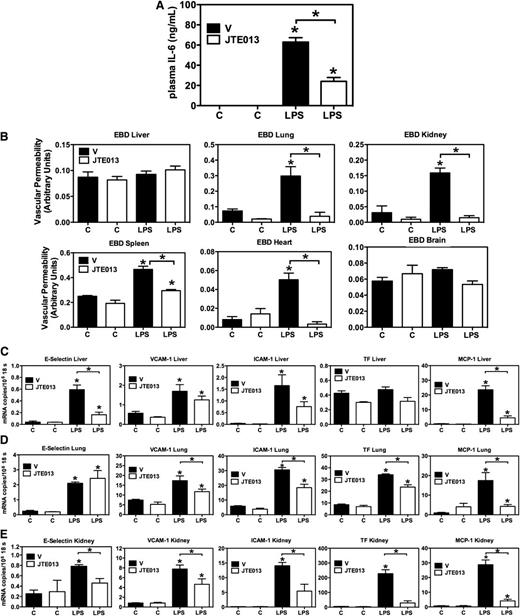
Pharmacologic inhibition of S1PR2 signaling by JTE013 results in lower expression of inflammatory and coagulation mediators during endotoxemia
Next, we tested the effects of pharmacologic inhibition of S1PR2 on vascular inflammation during endotoxemia. WT C57BL/6 mice were administered (by gavage) 30 mg/kg of the S1PR2 antagonist JTE01317,24 just before intraperitoneal administration of LPS. Eighteen hours after LPS administration, plasma was collected for assessment of IL-6 levels. In agreement with our data in S1pr2 null mice, JTE013 administration resulted in more rapid recovery of plasma IL-6 levels (24.02 ± 3.84 ng/mL and 62.96 ± 4.32 ng/mL in JTE013-treated and vehicle-treated mice, respectively, at 18 hours; Figure 3A). In addition, JTE013-treated mice exhibited decreased vascular permeability (Figure 3B) and lower mRNA (Figure 3C-E) and protein levels (supplemental Figures 4 and 5) of proinflammatory markers, similar to S1pr2−/− mice.
Pharmacologic inhibition of S1PR2 by JTE013 results in decreased inflammation during endotoxemia. (A) Reduced plasma IL-6 levels in LPS- and JTE013-treated mice (30 mg/kg) (LPS, open bars) compared with LPS- and vehicle-treated mice (LPS, solid bars). Data are mean ± SEM (n = 18). (B) LPS-induced vascular permeability is abrogated in JTE013-treated mice. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by EBD extravasation assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between vehicle-treated (V) and JTE013-treated (JTE013) mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in vehicle-treated (V) control and JTE013-treated (JTE013) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time PCR analyses (mRNA copy number per 106 copies of 18s rRNA) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between V and JTE013.
Pharmacologic inhibition of S1PR2 by JTE013 results in decreased inflammation during endotoxemia. (A) Reduced plasma IL-6 levels in LPS- and JTE013-treated mice (30 mg/kg) (LPS, open bars) compared with LPS- and vehicle-treated mice (LPS, solid bars). Data are mean ± SEM (n = 18). (B) LPS-induced vascular permeability is abrogated in JTE013-treated mice. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by EBD extravasation assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between vehicle-treated (V) and JTE013-treated (JTE013) mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in vehicle-treated (V) control and JTE013-treated (JTE013) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time PCR analyses (mRNA copy number per 106 copies of 18s rRNA) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between V and JTE013.
Altogether our data indicate that genetic deletion or pharmacologic inhibition of S1PR2 abrogates the permeability responses of the vascular endothelium and results in a significant decrease in endothelial adhesion molecule expression as well as proinflammatory and procoagulation markers 18 hours after LPS injection.
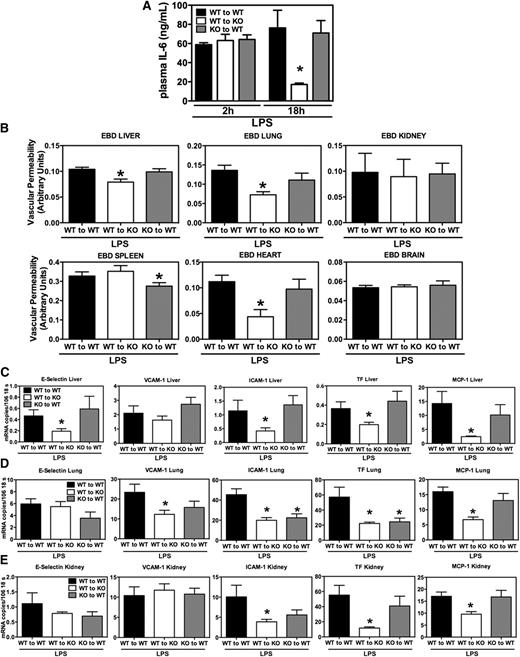
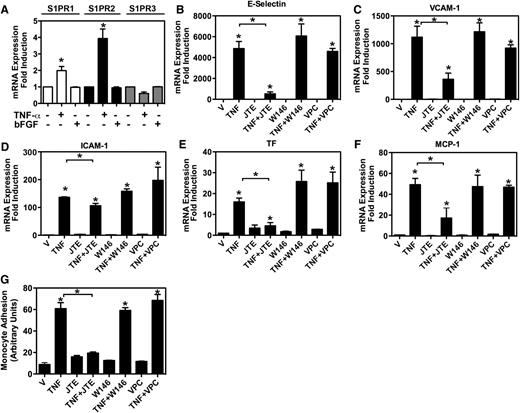
Critical role of S1PR2 in the stromal compartment in the permeability and inflammatory phenotype of the endothelium during endotoxemia
To elucidate the contribution of S1PR2 in the hematopoietic and stromal compartments to acute vascular inflammation, we reconstituted irradiated S1pr2−/− mice with WT bone marrow (S1pr2+/+ → S1pr2−/−) and WT mice with S1pr2−/− bone marrow (S1pr2−/− → S1pr2+/+). S1pr2+/+ mice reconstituted with S1pr2+/+ bone marrow (S1pr2+/+ → S1pr2+/+) were used as controls. S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+ chimeras equally developed systemic inflammation 2 hours after LPS injection, as assessed by the levels of IL-6 in plasma (Figure 4A). Similar to S1pr2−/− mice, in the S1pr2+/+ → S1pr2−/− chimeric mice, inflammation resolved faster compared with S1pr2+/+ → S1pr2+/+ or to S1pr2−/− → S1pr2+/+ chimeras (18 hours after LPS injection; Figure 4A). Despite high plasma IL-6 levels in all three groups of mice 2 hours after LPS injection (Figure 4A), vascular permeability was significantly lower (20% to 60% reduction) in liver, lung, and heart only in the S1pr2+/+ → S1pr2−/− chimeric mice compared with the control chimeras (S1pr2+/+ → S1pr2+/+) (Figure 4B). No differences in vascular permeability were found in kidneys among these three groups, possibly because of the lack of involvement of S1PR2 in radiation-induced nephropathy, which progressively develops after total body irradiation.25 Together, these data indicate the critical role of S1PR2 signaling in the stromal compartment in the regulation of vascular permeability and resolution of systemic inflammation during endotoxemia.
Critical role of stromal S1PR2 in the permeability and inflammatory phenotype of the endothelium during endotoxemia. (A) Reduced late-stage inflammation in S1pr2+/+ → S1pr2−/− chimeric mice (open bars) compared with S1pr2+/+ → S1pr2+/+ (solid bars) and with S1pr2−/− → S1pr2+/+ (shaded bars). Plasma IL-6 levels were measured 2 and 18 hours after LPS injection. Data are mean ± SEM (n = 4 to 7). (B) LPS-induced vascular permeability is inhibited in liver, lung, and heart of mice lacking S1PR2 in stromal cells (S1pr2+/+ → S1pr2−/−) compared with S1pr2+/+ → S1pr2+/+, but not in mice lacking S1PR2 in the hematopoietic compartment (S1pr2−/− → S1pr2+/+). Three hours after injection of LPS, vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by EBD extravasation assay. Values are mean ± SEM (n = 4 to 5). *P < .05 compared with S1pr2+/+ → S1pr2+/+. (C-E) Tissue mRNA levels of proinflammatory and procoagulant molecules in S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+ mice 18 hours after LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time PCR analyses (mRNA copy number per 106 copies of 18s rRNA) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 6 to 7). *P < .05 compared with S1pr2+/+ → S1pr2+/+.
Critical role of stromal S1PR2 in the permeability and inflammatory phenotype of the endothelium during endotoxemia. (A) Reduced late-stage inflammation in S1pr2+/+ → S1pr2−/− chimeric mice (open bars) compared with S1pr2+/+ → S1pr2+/+ (solid bars) and with S1pr2−/− → S1pr2+/+ (shaded bars). Plasma IL-6 levels were measured 2 and 18 hours after LPS injection. Data are mean ± SEM (n = 4 to 7). (B) LPS-induced vascular permeability is inhibited in liver, lung, and heart of mice lacking S1PR2 in stromal cells (S1pr2+/+ → S1pr2−/−) compared with S1pr2+/+ → S1pr2+/+, but not in mice lacking S1PR2 in the hematopoietic compartment (S1pr2−/− → S1pr2+/+). Three hours after injection of LPS, vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by EBD extravasation assay. Values are mean ± SEM (n = 4 to 5). *P < .05 compared with S1pr2+/+ → S1pr2+/+. (C-E) Tissue mRNA levels of proinflammatory and procoagulant molecules in S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+ mice 18 hours after LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time PCR analyses (mRNA copy number per 106 copies of 18s rRNA) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 6 to 7). *P < .05 compared with S1pr2+/+ → S1pr2+/+.
Next, we measured the mRNA levels of proinflammatory and procoagulation mediators in liver, lung, and kidney. In the liver, the S1pr2+/+ → S1pr2−/− chimeric mice exhibited significantly lower expression of E-selectin, ICAM-1, TF, and MCP-1 compared with S1pr2+/+ → S1pr2+/+ (Figure 4C). On the contrary, the levels of these proinflammatory markers were similar in the livers of S1pr2−/− → S1pr2+/+ mice compared with livers of S1pr2+/+ → S1pr2+/+ mice. In the lungs, similar to what we observed in S1pr2−/− mice, lower levels of VCAM-1, ICAM-1, TF, and MCP-1 were observed in the S1pr2+/+ → S1pr2−/− chimeras compared with S1pr2+/+ → S1pr2+/+ chimeras (Figure 4D). In contrast, lower levels of ICAM-1 and TF were observed only in the S1pr2−/− → S1pr2+/+ chimeric lungs. Finally, in the kidneys, we found significantly lower expression of ICAM-1, TF, and MCP-1 in the S1pr2+/+ → S1pr2−/− chimeras, while in the S1pr2−/− → S1pr2+/+ cohort, the levels of all these proinflammatory markers were similar to levels in the S1pr2+/+ → S1pr2+/+ group (Figure 4E).
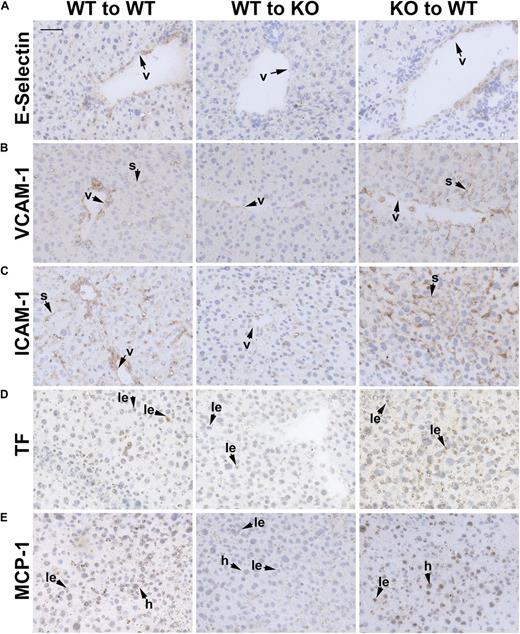
Immunohistochemical analysis of livers (Figure 5A-E) and kidneys (supplemental Figure 6A-E) from chimeric mice revealed markedly less immunoreactivity for adhesion molecules, TF, and MCP-1 only in S1pr2+/+ → S1pr2−/− mice compared with S1pr2+/+ → S1pr2+/+ mice, consistent with our mRNA findings.
Immunohistochemical analysis of proinflammatory markers in livers from chimeric mice. Immunostaining for (A) E-selectin, (B) VCAM-1, (C) ICAM-1, (D) TF, and (E) MCP-1 in livers from LPS-treated S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+ mice 18 hours after LPS injection. (A-C) Note that immunoreactivity for adhesion molecules was markedly decreased in venules and liver sinusoids only in the S1pr2+/+ → S1pr2−/− mice compared with S1pr2+/+ → S1pr2+/+ mice. (D) TF immunoreactivity was also significantly lower in infiltrating leukocytes from the S1pr2+/+ → S1pr2−/− chimeras. (E) Significantly lower levels of MCP-1 were detected only in hepatocytes and leukocytes from S1pr2+/+ → S1pr2−/− mice compared with S1pr2+/+ → S1pr2+/+ mice. Scale bar, 50 μm. Representative fields from 3 to 5 mice are shown. Images were captured with the Axio Imager A1 microscope, using AxioCam MRc camera and the AxioVision 4.8 program (Carl Zeiss Inc.) (original magnification ×40). h, hepatocyte; le, leukocyte; s, sinusoid; v, venule.
Immunohistochemical analysis of proinflammatory markers in livers from chimeric mice. Immunostaining for (A) E-selectin, (B) VCAM-1, (C) ICAM-1, (D) TF, and (E) MCP-1 in livers from LPS-treated S1pr2+/+ → S1pr2+/+, S1pr2+/+ → S1pr2−/−, and S1pr2−/− → S1pr2+/+ mice 18 hours after LPS injection. (A-C) Note that immunoreactivity for adhesion molecules was markedly decreased in venules and liver sinusoids only in the S1pr2+/+ → S1pr2−/− mice compared with S1pr2+/+ → S1pr2+/+ mice. (D) TF immunoreactivity was also significantly lower in infiltrating leukocytes from the S1pr2+/+ → S1pr2−/− chimeras. (E) Significantly lower levels of MCP-1 were detected only in hepatocytes and leukocytes from S1pr2+/+ → S1pr2−/− mice compared with S1pr2+/+ → S1pr2+/+ mice. Scale bar, 50 μm. Representative fields from 3 to 5 mice are shown. Images were captured with the Axio Imager A1 microscope, using AxioCam MRc camera and the AxioVision 4.8 program (Carl Zeiss Inc.) (original magnification ×40). h, hepatocyte; le, leukocyte; s, sinusoid; v, venule.
Altogether, our data indicate that S1PR2 expression in the stromal/endothelial compartment is critical for the induction of vascular permeability and the sustained expression of proinflammatory and procoagulation markers in several vascular beds during endotoxemia.
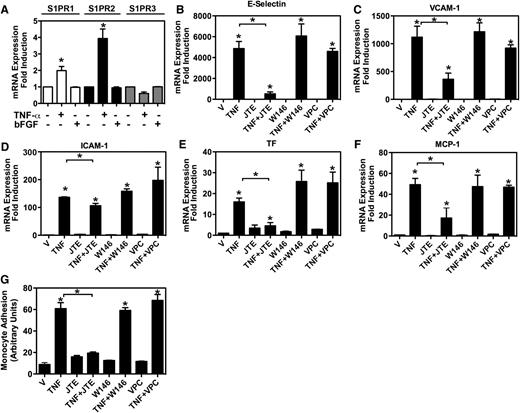
S1PR2 plays a critical role in the inflammatory responses of the endothelium in vitro
Given our in vivo findings, we next set out to establish an in vitro model to further assess the role of S1PR2 in the inflammatory responses of the vascular endothelium. Given that tumor necrosis factor-alpha (TNF-α) is a critical inflammatory mediator during endotoxemia, we tested the inflammatory responses of human umbilical vein endothelial cells (HUVEC) to TNF-α. We found that S1PR2 mRNA was induced upon stimulation with TNF-α (4.1-fold ± 0.5-fold) but not with basic fibroblast growth factor (Figure 6A). We also observed a modest increase in S1PR1 levels upon TNF-α stimulation (1.9-fold ± 0.2-fold) and no significant changes in S1PR3 mRNA levels (Figure 6A). In order to study the role of S1PRs in endothelial inflammation, we first analyzed the expression of adhesion molecules (E-selectin, VCAM-1, ICAM-1) and coagulation (TF) and proinflammatory (MCP-1) markers in endothelial cells 12 hours after TNF-α stimulation in the absence or the presence of specific S1PR antagonists. We used the specific S1PR2 antagonist JTE013,17,24 the S1PR1 and S1PR3 antagonist VPC 23019,26 and the S1PR1-specific antagonist W146.9 Inhibition of S1PR2 signaling during TNF-α stimulation by JTE013 potently inhibited the induction of E-selectin, VCAM-1, TF, and MCP-1 at 12 hours (89.3% ± 1%, 59.5% ± 5.3%, 73.4% ± 6.2%, and 70% ± 1.5% inhibition, respectively) (Figure 6B-C,E-F). A modest but significant inhibition of ICAM-1 expression was observed (15% ± 8.4%) (Figure 6D). In contrast, the specific S1PR1 antagonist W146 and the S1PR1 and S1PR3 antagonist VPC 23019 did not significantly affect the expression levels of these activation markers.
Critical role of S1PR2 in endothelial inflammation in vitro. (A) S1PR1, S1PR2, and S1PR3 mRNA levels in HUVEC. HUVEC were incubated with vehicle (–), TNF-α, or basic fibroblast growth factor (bFGF) in 0.5% fetal bovine serum endothelial basal media-2 for 12 hours. Shown are the results of quantitative real-time PCR analyses (fold induction TNF-α–treated vs non-treated cells). Data are mean ± SEM of three independent experiments. *P < .05 treated vs non-treated cells. (B-F) mRNA levels of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 in HUVEC. HUVEC were incubated with vehicle (V) or TNF-α (TNF) in the absence or presence of the S1PR2-specific antagonist JTE013 (JTE), the S1PR1-specific antagonist W146, or the S1PR1 and S1PR3 antagonist VPC 23019 (VPC). Shown are the results of quantitative real-time PCR analyses (fold induction TNF-α–treated vs non-treated cells). (B-G) All S1PR antagonists were used at 30 μM concentration. (G) Blockade of S1PR2 signaling in HUVEC inhibits U937 monocyte adhesion. HUVEC were treated with vehicle (V) or TNF-α (TNF) in the absence or presence of the S1PR2-specific antagonist JTE013 (JTE), the S1PR1-specific antagonist W146, or the S1PR1 and S1PR3 antagonist VPC 23019 (VPC). Results are mean ± SEM of quadruplets of 1 representative experiment of 3 experiments with similar results. *P < .05 TNF-α–treated vs non-treated cells and, where indicated, between TNF-α–treated and TNF-α+ antagonist–treated cells.
Critical role of S1PR2 in endothelial inflammation in vitro. (A) S1PR1, S1PR2, and S1PR3 mRNA levels in HUVEC. HUVEC were incubated with vehicle (–), TNF-α, or basic fibroblast growth factor (bFGF) in 0.5% fetal bovine serum endothelial basal media-2 for 12 hours. Shown are the results of quantitative real-time PCR analyses (fold induction TNF-α–treated vs non-treated cells). Data are mean ± SEM of three independent experiments. *P < .05 treated vs non-treated cells. (B-F) mRNA levels of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 in HUVEC. HUVEC were incubated with vehicle (V) or TNF-α (TNF) in the absence or presence of the S1PR2-specific antagonist JTE013 (JTE), the S1PR1-specific antagonist W146, or the S1PR1 and S1PR3 antagonist VPC 23019 (VPC). Shown are the results of quantitative real-time PCR analyses (fold induction TNF-α–treated vs non-treated cells). (B-G) All S1PR antagonists were used at 30 μM concentration. (G) Blockade of S1PR2 signaling in HUVEC inhibits U937 monocyte adhesion. HUVEC were treated with vehicle (V) or TNF-α (TNF) in the absence or presence of the S1PR2-specific antagonist JTE013 (JTE), the S1PR1-specific antagonist W146, or the S1PR1 and S1PR3 antagonist VPC 23019 (VPC). Results are mean ± SEM of quadruplets of 1 representative experiment of 3 experiments with similar results. *P < .05 TNF-α–treated vs non-treated cells and, where indicated, between TNF-α–treated and TNF-α+ antagonist–treated cells.
Given that our in vitro model demonstrated S1PR2-mediated inflammatory responses similar to those observed in vivo, we next investigated the functional role of endothelial S1PR2 in monocyte adhesion to endothelial monolayers, a critical step for the recruitment of leukocytes to sites of inflammation. In agreement with our gene expression data, we found that blockade of S1PR2 signaling by JTE013 during activation of HUVEC with TNF-α potently inhibited U937 monocyte adhesion to endothelial monolayers (60% ± 8.4% inhibition) (Figure 6G), consistent with the anticipated functional effects of the reductions seen in adhesion molecules and MCP-1 levels. In contrast, the specific S1PR1 antagonist W146 and the S1PR1 and S1PR3 antagonist VPC 23019 did not significantly affect TNF-α-induced adhesion. Altogether our gene expression data and monocyte adhesion functional data indicate a critical role for S1PR2 in mediating endothelial inflammatory responses.
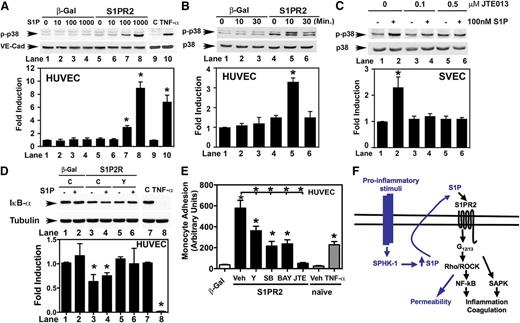
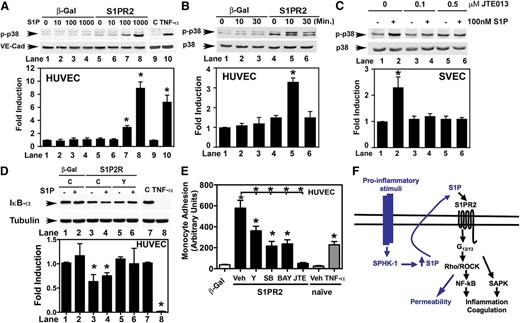
Activation of the p38 SAPK and NF-κB pathways by S1PR2 in endothelial cells
Given the critical role of S1PR2 in endothelial inflammation both in vivo and in vitro, we next set out to investigate the biochemical pathways downstream of S1PR2. We have previously shown the strong activation of the Rho GTPase by S1PR2 in endothelial cells.17 The Rho-ROCK pathway has been shown to play a critical role during vascular remodeling and inflammation27,28 through the activation of the stress activated protein kinase (SAPK)29,30 and the nuclear factor kappa B (NF-κB) pathways.31 Given these previously published results, we tested the activation of p38 SAPK32 by S1PR2 in endothelial cells. First, we upregulated S1PR2 levels in HUVEC by adenoviral transduction to achieve similar mRNA S1PR2 levels compared with S1PR1 to counteract S1PR1 signaling, as we have previously described.17,18 β-galactosidase (β-gal) adenovirus (Ad) was used as control. We found that S1P did not induce p38 phosphorylation in control adenovirus–transduced HUVEC. However, when S1PR2 was upregulated, S1P treatment induced dual phosphorylation of p38 SAPK (Thr180 and Tyr182), which is known to result in increased kinase activity33 (Figure 7A). We observed significant upregulation of phospho-p38 SAPK levels at physiological S1P concentrations34 (3-fold ± 0.2-fold induction at 100 nM S1P and 9-fold ± 0.8-fold at 1000 nM for 10 minutes) only in Ad-S1PR2 HUVEC. p38 SAPK phosphorylation peaked after 10 minutes of S1PR2 activation and diminished 30 minutes after ligand stimulation (Figure 7B), in agreement with G protein-coupled receptor internalization and desensitization dynamics.35,36 Consistent with previous findings,8,16,37,38 S1P did not activate p38 SAPK in HUVEC, even at high doses (up to 10 μM), unless S1PR2 was upregulated (supplemental Figure 7A).
Activation of the p38 SAPK and NF-κB pathways by S1PR2 in endothelial cells. (A) Western blot of phospho-p38 (p-p38) and total VE-cadherin (VE-cad) levels in adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) stimulated with S1P for 10 minutes (lanes 1 to 8), and naïve HUVEC treated with vehicle or 10 ng/mL TNF-α for 10 minutes (lanes 9 and 10). (B) Phospho-p38 SAPK (p-p38) and total p38 SAPK levels in adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) stimulated with 100 nM S1P for the times indicated. (C) Western blot of phospho-p38 SAPK and total p38 SAPK from SVEC cells stimulated with 100 nM S1P in the absence or the presence of JTE013. (D) The activation of the NF-κB pathway by S1PR2 is dependent on ROCK activity. Lanes 1 to 6: adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) were pretreated with vehicle (C) or 10 μM Y-27632 (Y) and treated with 100 nM S1P for 10 minutes when indicated (+). Lanes 7 to 8: naïve HUVEC were treated with vehicle (C) or 10 ng/mL TNF-α for 10 minutes. (A-D) Fold induction vs non-treated cells is plotted. Values are mean ± SEM of 3 to 5 independent experiments. One representative Western blot is shown. *P < .05 treated vs non-treated cells. (E) Upregulation of S1PR2 in HUVEC induces U937 monocyte adhesion in a ROCK-, p38-, and NF-κB–dependent way. Twenty hours after transduction, adenovirus control (β-gal) and Ad-S1PR2 HUVEC (S1PR2) were incubated with 10 μM Y-27632 (Y), 10 μM SB203580 (SB), 5 μM BAY 11-7085 (BAY), or 10 μM JTE013 (JTE) for 4 hours, and monocyte adhesion assays were conducted as described. Adhesion to naïve HUVEC stimulated with 2 ng/mL TNF-α is shown on the right. Results are mean ± SEM (n = 4) of 1 representative experiment of 3 experiments with similar results. *P < .05 β-gal vs S1PR2 and, when indicated, between vehicle-treated and inhibitor-treated Ad-S1PR2 HUVEC. (F) Diagram summarizing our findings (black) together with other data published by our laboratory and other groups (blue). Upon endothelial cell activation by proinflammatory stimuli, SPHK-1 is activated44,46 and S1P is released.45 Blockade of S1PR2 signaling results in inhibition of the expression of proinflammatory and procoagulant molecules by TNF-α. Upregulation of S1PR2 increases endothelial permeability, which is dependent on the Rho-ROCK pathway.17 In addition, S1PR2 induces endothelial inflammation and the activation of the Rho-ROCK-NF-κB and p38 SAPK pathways. Both pathways are activated in parallel by S1PR2 and play a critical role in the induction of proinflammatory molecules.
Activation of the p38 SAPK and NF-κB pathways by S1PR2 in endothelial cells. (A) Western blot of phospho-p38 (p-p38) and total VE-cadherin (VE-cad) levels in adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) stimulated with S1P for 10 minutes (lanes 1 to 8), and naïve HUVEC treated with vehicle or 10 ng/mL TNF-α for 10 minutes (lanes 9 and 10). (B) Phospho-p38 SAPK (p-p38) and total p38 SAPK levels in adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) stimulated with 100 nM S1P for the times indicated. (C) Western blot of phospho-p38 SAPK and total p38 SAPK from SVEC cells stimulated with 100 nM S1P in the absence or the presence of JTE013. (D) The activation of the NF-κB pathway by S1PR2 is dependent on ROCK activity. Lanes 1 to 6: adenovirus control (β-gal) and Ad-S1PR2–transduced HUVEC (S1PR2) were pretreated with vehicle (C) or 10 μM Y-27632 (Y) and treated with 100 nM S1P for 10 minutes when indicated (+). Lanes 7 to 8: naïve HUVEC were treated with vehicle (C) or 10 ng/mL TNF-α for 10 minutes. (A-D) Fold induction vs non-treated cells is plotted. Values are mean ± SEM of 3 to 5 independent experiments. One representative Western blot is shown. *P < .05 treated vs non-treated cells. (E) Upregulation of S1PR2 in HUVEC induces U937 monocyte adhesion in a ROCK-, p38-, and NF-κB–dependent way. Twenty hours after transduction, adenovirus control (β-gal) and Ad-S1PR2 HUVEC (S1PR2) were incubated with 10 μM Y-27632 (Y), 10 μM SB203580 (SB), 5 μM BAY 11-7085 (BAY), or 10 μM JTE013 (JTE) for 4 hours, and monocyte adhesion assays were conducted as described. Adhesion to naïve HUVEC stimulated with 2 ng/mL TNF-α is shown on the right. Results are mean ± SEM (n = 4) of 1 representative experiment of 3 experiments with similar results. *P < .05 β-gal vs S1PR2 and, when indicated, between vehicle-treated and inhibitor-treated Ad-S1PR2 HUVEC. (F) Diagram summarizing our findings (black) together with other data published by our laboratory and other groups (blue). Upon endothelial cell activation by proinflammatory stimuli, SPHK-1 is activated44,46 and S1P is released.45 Blockade of S1PR2 signaling results in inhibition of the expression of proinflammatory and procoagulant molecules by TNF-α. Upregulation of S1PR2 increases endothelial permeability, which is dependent on the Rho-ROCK pathway.17 In addition, S1PR2 induces endothelial inflammation and the activation of the Rho-ROCK-NF-κB and p38 SAPK pathways. Both pathways are activated in parallel by S1PR2 and play a critical role in the induction of proinflammatory molecules.
We also used the axillary lymph node vascular endothelial cell line SVEC.39 SVEC express high levels of endogenous S1PR2 transcript and much lower levels of S1PR1 and S1PR3 (supplemental Figure 8A). We found that S1P stimulation in the mouse SVEC endothelial cell line resulted in dual Thr180 and Tyr182 p38 phosphorylation (Figure 7C). Preincubation with JTE01317,24 abrogated the ability of S1P to induce p38 phosphorylation, indicating that the S1P-induced activation of the p38 SAPK signaling pathway in SVEC cells is mediated by S1PR2. Altogether, our data indicate that activation of S1PR2 in human and mouse endothelial cells results in activation of the p38 SAPK pathway.
Since several reports indicate the role of the GTPase Rho and its effector ROCK in the activation of SAPK,40 we investigated whether ROCK was involved in p38 activation by S1PR2 in endothelial cells. To study whether the activation of p38 SAPK is downstream of the Rho-ROCK pathway, we used the ROCK pharmacologic inhibitor Y-27632.41 As shown in supplemental Figure 8B-C, Y-27632 pretreatment did not inhibit S1P-induced p38 SAPK phosphorylation in S1PR2 transduced HUVEC or SVEC cells. Consistent with these findings, by using a functional assay, we also found that these two pathways are independent and are required for the induction of the proadhesion phenotype of endothelial cells by S1PR2 (supplemental Figure 8D).
To further investigate the role of endothelial S1PR2 in the activation of the SAPK pathway during endotoxemia, mouse heart and lung endothelial cells from WT and S1pr2−/− mice were isolated. In WT primary mouse heart endothelial cells, S1PR1 transcript was abundantly expressed (79.5 ± 7.8 copies per 106 18S, which is equivalent to approximately 79.5 ± 7.8 copies per cell.)42 In addition, lower levels of S1PR2 transcript were detected (2.25 ± 0.25 copies per cell) (supplemental Figure 9A). Stimulation with S1P did not significantly induce SAPK phosphorylation in mouse heart endothelial cells, which is consistent with the high levels of S1PR1 relative to S1PR2. On the contrary, stimulation with plasma from WT endotoxemic mice for 15 minutes potently induced activation of the p38 SAPK pathway in WT endothelial cells (supplemental Figure 9B). In agreement with our in vivo data, we observed a significant decrease in p38 SAPK phosphorylation in S1pr2−/− cells compared with S1pr2+/+ (∼25% inhibition). Altogether, our in vitro data indicate that S1PR2 is a critical modulator of the p38 SAPK pathway during inflammation in human and mouse endothelial cells.
Last, we investigated the activation of the NF-κB pathway by S1PR2. Activation of the NF-κB protein complex by inflammatory stimuli requires the degradation of the inhibitor of κB (IκB) proteins, which keep NF-κB proteins sequestered in the cytoplasm in an inactive state.43 In naïve (supplemental Figure 7B) or β-gal HUVEC (Figure 7D), S1P had no effect on IκB-α degradation. However, upregulation of S1PR2 resulted in a modest activation of the NF-κB pathway, assessed by degradation of IκB-α (Figure 7D). Interestingly, in contrast to p38 activation, activation of the NF-κB pathway by S1PR2 was dependent on ROCK activity, and it was inhibited by Y-27632 (Figure 7D). Upregulation of S1PR2 levels in HUVEC by adenoviral transduction also resulted in induced expression of proinflammatory molecules (supplemental Figure 10) and a dramatic increase in U937 monocyte adhesion to HUVEC monolayers (Figure 7E) in a ROCK-, NF-κB-, and p38-dependent way. Altogether, these data indicate that upregulation of S1PR2 in endothelial cells activates the p38 SAPK and the ROCK-NF-κB pathways. Both pathways are critical for the induction of vascular inflammation by S1PR2 (Figure 7F).
Discussion
The vascular endothelium, as the interface between blood and all tissues plays a critical role in inflammation. During inflammation, cytokines confer a permeability proadhesive and prothrombotic phenotype in the endothelium.19,20 These endothelial responses are carefully orchestrated to neutralize the source of injury. However, if the injury persists, these sustained responses may result in endothelial dysfunction, which plays a critical role in the pathophysiology of vascular disease.19-21 The role of the bioactive sphingolipid S1P and its receptor S1PR2 in the regulation of endothelial responses to injury is just beginning to be understood. In this article, we have described the critical role of S1PR2 in endothelial inflammation both in vivo and in vitro.
Using a mouse model of endotoxemia, we have shown by pharmacologic and genetic approaches that S1PR2 plays a critical role in acute vascular inflammation. WT and S1pr2−/− mice similarly responded to LPS injection by increasing plasma levels of proinflammatory cytokines and recruiting leukocytes into the tissues. However, during the early stages of the inflammatory response (3 to 6 hours after LPS injection), inhibition of S1PR2 signaling dramatically decreased vascular permeability in several vascular beds. This blunted permeability response could contribute to the faster resolution of vascular inflammation observed in the S1pr2−/− mice and WT mice treated with the S1PR2-specific antagonist JTE013. In addition, our in vivo data using bone marrow chimeras indicate the critical role of stromal S1PR2 in the regulation of vascular permeability and inflammation during endotoxemia, which is consistent with the role of endothelial S1PR2 in vascular inflammation. Our in vivo findings, together with our in vitro data, indicate the critical role of S1PR2 in the permeability and inflammatory responses of the endothelium to injury and warrant further investigations into the potential use of specific S1PR2 antagonists in a number of pathological conditions involving localized or systemic vascular permeability and inflammation, such as sepsis, ischemia-reperfusion injury, diabetic vasculopathy, or atherosclerosis.
Our in vitro data indicate that S1PR2 signaling is critical for TNF-α–induced expression of adhesion and procoagulant molecules and for monocyte adhesion to endothelial monolayers. Since TNF-α is known to activate SPHK in endothelial cells,44 our data are consistent with a model in which TNF-α stimulation of endothelial cells generates S1P, which activates S1PR2 in an autocrine or paracrine way, contributing to the TNF-α–induced proadhesion and proinflammatory phenotype (Figure 7F). In fact, endothelial cells exhibit high SPHK activity, and they are one of the main sources of plasma S1P.3,45 In addition, we have previously described the autocrine/paracrine activation of S1PR2 in HUVEC.17 Further studies are needed to understand the molecular mechanisms that control S1PR2 expression and signaling in the endothelium during inflammation, such as the characterization of the S1PR2 promoter, the posttranscriptional regulation of S1PR2 mRNA, and the posttranslational modifications of S1PR2 that could regulate receptor signaling, trafficking, and localization.
The role of S1P in endothelial inflammation has been controversial. The rate-limiting enzyme involved in S1P generation, SPHK-1, is activated in endothelial cells by both proinflammatory mediators, such as TNF-α,44 thrombin, or LPS,46 and anti-inflammatory molecules, such as activated protein C47 and angiopoietin-1,48 among others. Although early studies suggested the proinflammatory actions of S1P and SPHK-1 in endothelial cells,44 more recent studies highlight the role of the SPHK-1-S1P-S1PR1 axis in the maintenance of the integrity of the endothelium, which could serve as a negative feedback mechanism to limit the permeability responses of the endothelium to inflammatory stimuli.8,16,37,46 Our current data are consistent with these previous findings and indicate that S1PR2 plays a critical role in the induction of vascular permeability, which is the early response of the endothelium to injury, as well as in the proadhesion and procoagulant phenotype of the endothelium during inflammation.
Our in vitro data also shed light into the mechanisms whereby S1PR2 contributes to endothelial inflammation. We previously found that S1PR2 strongly activates the GTPase Rho in endothelial cells and increases endothelial permeability by inducing stress fiber formation and disassembly of adherens junctions, in a Rho-ROCK–dependent way.17 In addition to its role in actin cytoskeleton dynamics, the Rho-ROCK pathway has also been implicated in vascular remodeling and inflammation through the regulation of gene expression by transcriptional and posttranscriptional mechanisms. For instance, Rho kinases have been involved in transcriptional regulation of proinflammatory genes during hyperglycemia28 and activation of both SAPK and NF-κB pathways.29-31 Our current data describes the activation of the SAPK and ROCK-NF-κB pathways by S1PR2. Similar to TNF-α–induced expression of proinflammatory molecules in the endothelium, we found that the SAPK and NF-κB pathways play a critical role in the induction of endothelial inflammation by S1PR2. Therefore, the regulation of endothelial function by S1PR2 involves not only Rho-ROCK–mediated early changes in cytoskeleton dynamics and permeability but also the regulation of proinflammatory gene expression via the SAPK and ROCK-NF-κB pathways (Figure 7F).
Altogether, our current studies indicate that S1PR2 plays a critical role in the permeability, proadhesion and prothrombotic phenotype of the endothelium during systemic inflammation and identify S1PR2 as a novel and attractive therapeutic target for inflammatory vascular disorders.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dan Li and Dr Shou-ching Jaminet from the Multi-Gene Transcriptional Profiling Core Facility (Center for Vascular Biology Research, Beth Israel Deaconess Medical Center, Harvard Medical School) for the quantitative polymerase chain reaction analysis, Dr Richard Proia (National Institute of Diabetes and Digestive and Kidney Diseases) for providing the S1pr2−/− mice, Dr Timothy Hla (Cornell University) for the β-gal and S1PR2 adenoviruses, and Dr Paola Mina-Osorio (The Feinstein Institute for Medical Research) for technical help with the monocyte adhesion assays.
This work was supported by American Heart Association Scientist Development Grant grant 0630384N and National Institutes of Health grant HL094465 (T.S.).
National Institutes of Health
Authorship
Contribution: G.Z., K.R., and R.K.O. performed research, collected data, analyzed data, and wrote the manuscript; L.Y., S.L., and K.Y. performed research, collected data, and analyzed data; G.S.K. and K.S. performed research; N.S., W.C.A., M.J.K., and K.Y. designed experiments and interpreted data; W.C.A. and M.J.K. edited the manuscript; and T.S. designed experiments, performed research, analyzed data, interpreted data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for K.Y. is Cardiovascular-Metabolic Research Laboratories Daiichi-Sankyo, Tokyo 140-8710, Japan.
Correspondence: Teresa Sanchez, Beth Israel Deaconess Medical Center, 99 Brookline Ave, RN-227A, Boston, MA 02215; e-mail: tsanchez@bidmc.harvard.edu.

![Figure 1. S1pr2 null mice display decreased inflammation during endotoxemia. (A) Reduced late-stage inflammation in S1pr2−/− mice (knockout [KO]) compared with WT mice documented by plasma IL-6 levels at various time points following LPS administration. Data are mean ± standard error of the mean (SEM) (n = 4 to 14). (B) LPS-induced vascular permeability is abrogated in mice lacking S1PR2. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by the Evans blue dye extravasation (EBD) assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between WT and S1pr2−/− mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in S1pr2+/+ (WT) and S1pr2−/− (KO) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time polymerase chain reaction (PCR) analyses (mRNA copy number per 106 copies of 18s ribosomal RNA [rRNA]) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between WT and S1pr2−/− mice.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/3/10.1182_blood-2012-11-467191/4/m_443f1.jpeg?Expires=1769325735&Signature=M3zGaDp~0VY7OYxthXtg2m73C1tiPkYzte5NDfnhwzwZysdxL0Iei2Qgp6reTu3PFflXN1EdZlwSjjIO-~xVEB3WKIOeBa-c744ZxtOrFhAU7HNZ8r1j~1SsmSp2UjVjetYcZDxT4NzX3DirbN5ejaOdL6SdjLiUOfspd3IsHFnUstGpXdDGC8Jyre4LK1M1cB53hj483hj7rxijIJUIc1fIb1IFEuqgji3Dr3F59QB7Ltf9k-49YgYhmckN3kT9ZPrqupmlihVZfre9mYWMVQkebYs-8Bc8Fpn2b6Rcl6-7KABieA7RDPy9CeEqwjBLVrrXFWlwgmc8H7S8OuEkXA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 1. S1pr2 null mice display decreased inflammation during endotoxemia. (A) Reduced late-stage inflammation in S1pr2−/− mice (knockout [KO]) compared with WT mice documented by plasma IL-6 levels at various time points following LPS administration. Data are mean ± standard error of the mean (SEM) (n = 4 to 14). (B) LPS-induced vascular permeability is abrogated in mice lacking S1PR2. Six hours after injection of vehicle (–) or LPS (+), vascular permeability was measured in liver, lungs, kidneys, spleen, heart, and brain by the Evans blue dye extravasation (EBD) assay. Values are mean ± SEM (n = 4). *P < .05 compared with the respective untreated controls and, where indicated, between WT and S1pr2−/− mice. (C-E) Tissue mRNA expression levels of proinflammatory and procoagulant molecules in S1pr2+/+ (WT) and S1pr2−/− (KO) mice 18 hours after vehicle (C) or LPS challenge. (C) Liver, (D) lung, (E) kidney. The results of quantitative real-time polymerase chain reaction (PCR) analyses (mRNA copy number per 106 copies of 18s ribosomal RNA [rRNA]) of E-selectin, VCAM-1, ICAM-1, TF, and MCP-1 are shown. Data are mean ± SEM (n = 4 to 5) of one representative experiment of three with similar results. *P < .05 compared with the respective untreated controls (C vs LPS) and, where indicated, between WT and S1pr2−/− mice.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/3/10.1182_blood-2012-11-467191/4/m_443f1.jpeg?Expires=1769997558&Signature=FmkhzF1B3skxEpR8p94E1jYrUfh1YcZCOyDW38fs71hWC27TecBb07cKm5zeOM3-iIra34HVOHSZN92IgV8yhBHssA90DKGVZsNP20Od2Mg8tBfORpoHO0zPOjlZze2ma-j6MfdML4kTghbVZY~ClJGCJ4b0kbQnyiw8v0hy5GU4-K1UNZ7YKDIj0CPFbcXL-KvTVuLegL58jISpdQz14kyDibeFuJFCDCJ671qHXB-QHyRmWdnhTFZAz0UgB0YWqXQASfNZ9jV9dP9MYbX-7fC8v2~apH~uL25aIBB~tWBXATuDHHPujTCdwg-vLehYoRukl4lxCU0OnAKc2nKqjA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)