Key Points
The CXCR4 mutations in WHIM syndrome impair the stability of the T cell–antigen–presenting cell immunologic synapse.
Abstract
WHIM (warts, hypogammaglobulinemia, infections, myelokathexis) syndrome is a rare disease characterized by diverse symptoms indicative of aberrantly functioning immunity. It is caused by mutations in the chemokine receptor CXCR4, which impair its intracellular trafficking, leading to increased responsiveness to chemokine ligand and retention of neutrophils in bone marrow. Yet WHIM symptoms related to adaptive immunity, such as delayed IgG switching and impaired memory B-cell function, remain largely unexplained. We hypothesized that the WHIM-associated mutations in CXCR4 may affect the formation of immunologic synapses between T cells and antigen-presenting cells (APCs). We show that, in the presence of competing external chemokine signals, the stability of T-APC conjugates from patients with WHIM-mutant CXCR4 is disrupted as a result of impaired recruitment of the mutant receptor to the immunologic synapse. Using retrogenic mice that develop WHIM-mutant T cells, we show that WHIM-mutant CXCR4 inhibits the formation of long-lasting T-APC interactions in ex vivo lymph node slice time-lapse microscopy. These findings demonstrate that chemokine receptors can affect T-APC synapse stability and allow us to propose a novel mechanism that contributes to the adaptive immune response defects in WHIM patients.
Introduction
The rare human WHIM (warts, hypogammaglobulinemia, infections, myelokathexis) syndrome is characterized by neutropenia, myelokathexis, delayed antibody class switching to immunoglobulin G (IgG),1 long-term hypogammaglobulinemia and memory B-cell lymphopenia,2 recurring infections, and human papillomavirus–induced warts.3 WHIM is associated with C-terminal, dominant mutations in the chemokine receptor CXCR4, resulting in truncation of the receptor.4 This leads to defective recycling upon binding of the CXCR4 ligand, CXCL12, and thus increased responsiveness to CXCL12 stimulation.2,5,6 The hyperfunctional CXCR4 mutations may thus explain neutrophil retention in the bone marrow (BM; myelokathexis), where CXCL12 is expressed,7 and the consequent neutropenia in the periphery.8 However, the mechanism of pathogenesis of the remaining WHIM symptoms is less clear.3
Recurrent infections, the delay in production of IgG-switched antibodies found in one study,1 as well as the impaired memory B-cell function and lack of long-term antibody titers after immunization,2 are indicative of defects involving the adaptive immune response required for effective and lasting defense against invading pathogens. The initiation of the adaptive response involves antigen-specific activation of T cells in the secondary lymphoid organs, where antigen-presenting cells (APCs) flock to after taking up antigen in the periphery. After successful activation via a T-APC immunologic synapse formation, antigen-activated CD4+ T cells can then provide costimulatory signals to B cells, which enable the B cells to undergo immunoglobulin class switch recombination and thus synthesize IgG, IgA, and IgE.9 The resultant memory B cells and plasma cells subsequently migrate to their niches.1 It has been proposed that, in a manner analogous to the effect on neutrophils, WHIM-mutant CXCR4 on B cells may account for both the initial delay in mounting an IgG antibody response and the long-term memory B-cell dysfunction, by affecting the homing of the B cells.1
We have previously demonstrated that chemokine receptors, in addition to controlling leukocyte homing and migration, may increase the stability of the T-APC immunologic synapses,10 the specialized junctions that form at the initiation of adaptive immune responses and that are necessary for successful T-cell activation.11,12 Indeed, in vitro studies have led to the hypothesis that chemokines in lymph nodes may either enhance the stability of the synapse by reinforcing the “stop” signal transduced by the antigen-triggered T-cell receptor (TCR) or inhibit T-APC interactions by providing “go” signals overcoming the TCR.13-15 Whether this regulates T-cell activation in vivo is still unknown.
Given the hyperfunctional nature of WHIM-mutant CXCR4,2,5 we hypothesized that the WHIM-associated mutations in CXCR4 may interfere with the robustness of the T-APC synapses. This would be expected to affect T-cell activation, as well as the B-cell functions that are dependent on T-cell activation, such as immunoglobulin class switching. Here we show that the WHIM-associated mutations of CXCR4 impair T-APC synapse stability and may affect T-cell priming while causing a delay in IgG responses. These findings identify a novel mechanistic explanation for the defects in the early stages of adaptive immune responses in WHIM syndrome, while also offering a novel and natural demonstration of the role of chemokines in the regulation of the immunologic synapse stability.
Methods
Retrogenic mice
Animals were kept in an specific pathogen-free facility and treated according to institutional and national guidelines and regulations. Retrogenic mice were created as described in Holst et al16 : BM was harvested from donor OT-II ovalbumin (OVA)-specific TCR-transgenic CD45.1 mice, which had been pretreated with 5-fluoracil at 5.5 mg per 25 g body weight, 4 days before harvesting. Harvested BM cells were grown in 20 ng/mL rmIL-3, 50 ng/mL rmIL-6, and 50 ng/mL rmSCF (all R&D Systems) for 48 hours and then transduced with retroviral vectors for enhanced green fluorescent protein (EGFP)-wild-type (WT)-CXCR4 or EGFP-WHIM-CXCR4 and pCLEco (Imgenex) on days 2, 3, and 4 post-BM harvesting using fresh viral supernatants.17 The transduced BM cells were kept in culture for a further 2 days before intravenous injection into irradiated (2 × 475 Rad) C57BL/6 recipients. These recipients were used as retrogenic mice, 7 weeks post intravenous injection.
T-cell purification
Patient and healthy donor samples were obtained after informed consent at Clinica Pediatrica and Humanitas, according to the institutional ethical committee guidelines and the Declaration of Helsinki. Primary human CD4+ T cells from peripheral blood were isolated using RosetteSep (StemCell Technologies), at a typical purity of >90%. CD4+ T cells were transduced with CXCR4 constructs using Amaxa human T-cell nucleofector (Lonza). For experiments with patient samples, peripheral blood mononuclear cells from WHIM patients and healthy age- and gender-matched donors were expanded for 2 weeks after activation with 2.5 μg/mL phytohemagglutinin (Biochrom AG), 400 U/mL IL-2 (Chiron), and irradiated feeders; CD4+ T cells were then isolated using fluorescence-activated cell sorting (FACS) (FACSAria; BD) cell sorter. Mouse CD4+ T cells from retrogenic mice were harvested at 7 weeks after BM transfer, purified using a MACS CD4+ kit (Miltenyi Biotec), and then sorted for EGFP expression on FACSAria. For lymph node slice time-lapse 2-photon imaging experiments, the CD4+ EGFP+ WT or WHIM-mutant CXCR4-expressing retrogenic cells were labeled with 2 µM CFDA-SE (carboxyfluorescein diacetate succinimidyl ester; Invitrogen). EGFP– nonretrogenic T cells were labeled with 10 µM Blue-CMAC (7-amino-4-chloromethylcoumarin; Invitrogen) and used as a control population. Changing the dye used in the experimental populations did not modify the result. Nonetheless, as an additional measure, we chose to use the same dye for the 2 experimental populations to ensure that no differential toxic effects of the 2 dyes could affect measurements. Because this necessitated imaging of the 2 populations in consecutive slices, the same blue-CMAC–labeled nonretrogenic control population was used as an internal control in both cases.
T-APC conjugates
The conjugate stability assay by transwell migration and the analysis of receptor recruitment to the synapse were adapted10 with the following modifications: conjugates were formed between WT or WHIM-mutant CXCR4-expressing CD4+ T and primary B cells obtained via RosetteSep (StemCell Technologies). B cells had been pulsed with superantigen (1 μg/mL staphylococcal enterotoxin A/B/E; Toxin Technology) and labeled with PKH26 dye (Sigma-Aldrich) and were used at a 1:1 ratio with T cells. Cells were then allowed to migrate through 3-μm pores to 2.5 nM CXCL12 (R&D Systems) for 2 hours before analysis by FACS. Conjugates prepared for confocal microscopic analysis of receptor recruitment were made using EBV-B as APC and allowed to form in the presence or absence of CXCL12 (5-100 nM) and AMD3100 (Sigma-Aldrich; 12.6 μM). The relative recruitment index (RRI) for EGFP-CXCR4 was calculated.10
Two-photon microscopy imaging
Lymph-node slice preparation was adapted.18 BM-derived dendritic cells (DCs) were pulsed with 10 μg/mL OVA (323-339)(Anaspec), labeled with 5 μM CMTMR (5-(and-6)-(((4-chloromethyl)benzoyl)amino)tetramethylrhodamine) dye (Invitrogen), and injected along with 40 ng LPS (Sigma-Aldrich) at 4 × 106 cells/mouse subcutaneously into C57BL/6 mice. The following day, the recipients were sacrificed and the inguinal lymph nodes extracted and then enclosed in agarose and sliced using a vibratome (Leica VT 1000S). Labeled T cells from retrogenic mice were allowed to enter the lymph node for 1 hour before 3-color time-lapse imaging for 30 minutes with a 30-second interframe interval on a LaVision TrimScope 2-photon microscope. As described in Asperti-Boursin et al,18 the lymph node slices were placed in AMD3100 (12.6 μM; Sigma-Aldrich); to avoid the reported inhibition of entry into the lymph node slice, T cells were allowed 30 minutes in AMD3100-free medium to enter to the lymph node, followed by 30 minutes’ incubation in the presence of the inhibitor. AMD3100 was also present in the perfusion medium. Image analysis was performed on Imaris (Bitplane) using manually corrected automatic tracking and manual calculation of T-DC interaction times.
Activation experiments
T-cell priming was performed by injecting 500 ng OVA peptide in CFA into each hind footpad of WT or WHIM retrogenic mice. Draining lymph nodes and spleen were analyzed by FACS 12 hours after injection for the expression of EGFP and staining for CD45.1 (A20; eBiosciences), CD4 (GK1.5; BioLegend), and CD69 (H1.2F3; BD).
Immunizations for IgG production experiments were performed as in Hikida et al19 using 100 μg/mouse of NP(4-hydroxy-3-nitrophenylacetyl)-OVA (Biosearch) in Imject Alum (Pierce). Enzyme-linked immunosorbent assay (ELISA) for the detection of anti-NP IgG were adapted from Roes et al,20 coating plates with 10μg/mL NP-BSA (Biosearch, ratio >20) and detecting with anti-mouse IgG-peroxidase (Sigma). Human primary T-cell activation by anti-CD3/anti-CD28 and IFNγ detection by ELISA were performed as in Molon et al.10 For mouse in vitro APC-free T-cell activation, 2 μg/mL anti-CD3e (145-2C11; BD) and 1 μg/mL anti-CD28 (37.51; BD) were used for coating flat-bottom 96-well plates. The activation of rgWT and rgWHIM T cells by DC (at a 2:1 ratio) in the presence or absence of 25 nM CXCL12 in the lower chamber of transwell assay plates was analyzed by FACS after staining for CD25 (PC61.5; eBiosciences).
Results
WHIM-mutant CXCR4 disrupts the stability of T-APC conjugates in WHIM patients
Given the association of the WHIM-mutant CXCR4 with enhanced chemotactic properties,2,5 we decided to assess whether the mutant chemokine receptor could impair the stability of the T-APC interaction in WHIM patients. Peripheral blood CD4+ T cells purified from a WHIM patient (G336X) or a healthy age- and gender-matched donor were used in conjugate stability experiments.10 T cells were allowed to form conjugates with labeled, superantigen-pulsed primary B cells. Nonpulsed B cells, which cannot form successful T-B conjugates, were used as controls. The conjugates were then allowed to migrate in a transwell assay toward CXCL12, using a transwell filter pore size that allowed only single cells to pass through. The number of migrated CD4+ T cells is thus an indication of lack of conjugate stability.10 As expected, T cells from healthy donors were significantly impaired from migrating to CXCL12 when superantigen-pulsed B cells were used for conjugate formation, suggesting that “go” signals delivered by WT CXCR4 are subordinate to the “stop” signal delivered by the antigen-triggered TCRs (Figure 1A, left panel), in agreement with previous in vitro studies.13 However, under the same conditions, the chemotactic response of T cells from WHIM patients was strong and undiminished by the presence of antigen-loaded APCs (Figure 1A, right panel). The values shown are normalized to enable comparison between different donors. Thus, WHIM patient CD4+ T cells exhibit impaired conjugate stability in the presence of competing external CXCL12 signals.
WHIM-mutant CXCR4 impairs T cell–B cell conjugate stability. (A) Primary CD4+ T cells from healthy WT donor or WHIM-patient peripheral blood formed conjugates for 15′ with superantigen (sAg)-pulsed, labeled primary B cells from a healthy allogenic donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. The migrated T cells were analyzed by FACS and the number of T cells migrated for each condition is shown. *P < .05 (1-way analysis of variance [ANOVA] and Tukey’s posttest). Experiment performed twice, summary of results (mean ± SEM) shown. (B) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) formed conjugates for 15′ with sAg-pulsed primary B cells from the same donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. Migrated EGFP+ T cells were analyzed as described in (A). **P < .01 (1-way ANOVA and Tukey’s posttest). The experiment was performed twice, and results (mean ± SEM) from representative experiments are shown.
WHIM-mutant CXCR4 impairs T cell–B cell conjugate stability. (A) Primary CD4+ T cells from healthy WT donor or WHIM-patient peripheral blood formed conjugates for 15′ with superantigen (sAg)-pulsed, labeled primary B cells from a healthy allogenic donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. The migrated T cells were analyzed by FACS and the number of T cells migrated for each condition is shown. *P < .05 (1-way analysis of variance [ANOVA] and Tukey’s posttest). Experiment performed twice, summary of results (mean ± SEM) shown. (B) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) formed conjugates for 15′ with sAg-pulsed primary B cells from the same donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. Migrated EGFP+ T cells were analyzed as described in (A). **P < .01 (1-way ANOVA and Tukey’s posttest). The experiment was performed twice, and results (mean ± SEM) from representative experiments are shown.
Expression of WHIM-mutant CXCR4 disrupts the stability of T-APC conjugates in healthy donor cells
To prove that this is indeed caused by the mutant CXCR4, we cloned the WT and WHIM-mutant (R334X) versions of CXCR4 fused with EGFP. The ectopically expressed receptor was functional, because it could lead to phosphorylation of mitogen-activated protein kinases after CXCL12 administration (data not shown). Importantly, the WHIM-mutant CXCR4 was refractive to ligand-induced internalization (supplemental Figure 1, available on the Blood Web site), which is a hallmark of WHIM syndrome.5,6 We expressed WT or WHIM-mutant CXCR4 in primary CD4+ T cells from healthy donors and used them in conjugate stability experiments, as described before. Because the WHIM mutation is dominant,3 endogenous WT CXCR4 expression in transfected cells is unlikely to interfere with the experimental outcome. CXCL12 was able to break conjugates formed with T cells expressing the WHIM-mutant but not with WT CXCR4 (Figure 1B). This demonstrates that the WHIM-mutant CXCR4 per se has destabilizing effects on the immunologic synapse when exposed to competing cognate chemokine. Because CXCL12 is present in the lymph node environment,21 this “distracting” effect could affect physiological T-cell activation.
WHIM-mutant CXCR4 affects T-APC long-lasting interactions
To assess the physiological relevance of our findings, we tested our hypothesis utilizing ex vivo organ cultures of mouse lymph node slices.18,22 Because human CXCR4 is functional in mice,8 we created retroviral versions of the CXCR4 constructs described before and used them to make retrogenic mice16 for WT or WHIM-mutant CXCR4. These mice generate mature, unactivated OVA-antigen–specific T cells expressing WT or WHIM-mutant CXCR4, 6 weeks after reconstitution of irradiated recipients with transduced BM cells16,23 (see Methods).
The WHIM retrogenic mice showed a fourfold increase in BM retention of WHIM-mutant CXCR4-expressing leukocytes in sentinel animals (data not shown), similar to previously reported models.8 Nonetheless, the mice should be considered “retrogenic cell generators” rather than disease models. Indeed, our intention was to analyze the effects of the WHIM mutations on T cell–mediated responses to antigenic stimulation in a physiological environment but in the absence of additional complicating variables that may be affected by WHIM-mutant CXCR4 expression on other tissues.
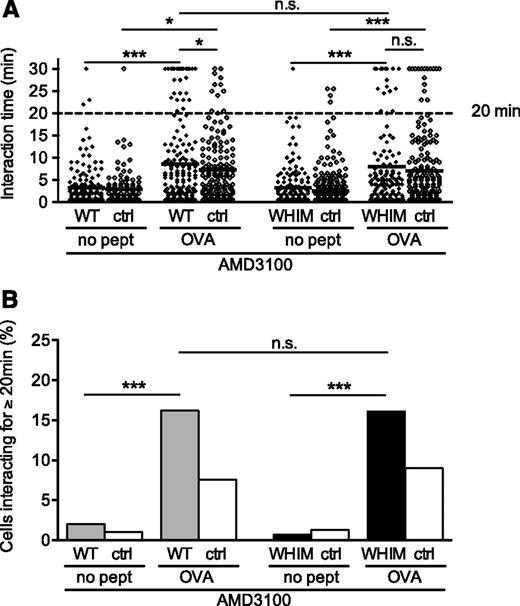
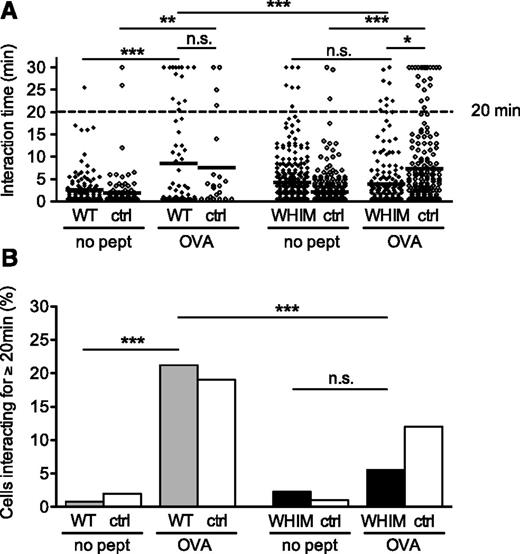
From the retrogenic mice, we purified CD4+ T cells expressing retrogenic WT (rgWT) or WHIM-mutant (rgWHIM) CXCR4. OVA-specific T cells with no retrogenic expression were used as a control population. The T cells were labeled and allowed to enter into ex vivo organ cultures of lymph node slices,18,22 which had been extracted from mice that had received OVA antigen-pulsed, CMTMR-labeled DCs on the previous day. The slices were imaged using 2-photon time-lapse video microscopy starting 1 hour after administration of the T-cell populations onto the lymph node slices. We analyzed all T cells that interacted with DCs during the 30 minutes of each video. Control T cells, with no retrogene expression, formed more long-lasting interactions (clustering at ≥20 minutes) in the presence of OVA-pulsed as opposed to unpulsed DCs (supplemental Figure 2), in agreement with previous reports.24 The difference in the number of long versus short interactions was significant (Figure 2A). T cells expressing rgWT CXCR4 exhibited an identical behavior (Figure 2A; supplemental Videos 1-3), indicating that, in this assay, the retrogenic expression per se does not distort the physiological function of the cells. Interestingly, rgWHIM T cells did not show any significant increase in the number of long-lasting interactions (Figure 2A; also plotted as % in Figure 2B, black bars; supplemental Videos 4-5) with antigen presence, thus confirming that the WHIM mutation impairs the ability of T cells to form long-lasting interactions with antigen-pulsed DCs. In the presence of cognate antigen-pulsed DCs, the mean 3-dimensional speed of the WT cells was 1.7 μm/min vs 2.3 μm/min for the WHIM T cells, which is consistent with the more frequent interactions of the latter with DCs.
WHIM-mutant CXCR4 impairs T-DC interactions in ex vivo lymph node slice cultures. DCs were either cognate antigen-pulsed (OVA) or unpulsed (no pept). (A) Duration of T-DC interactions within ex vivo lymph node slices imaged by 2-photon microscopy. The summary results of 2 videos per condition are shown. Each dot represents a single T-DC interaction (from left to right, n = 125, 101, 66, 21, 298, 291, 197, and 183). An independent experiment with the T-cell populations labeled with different dyes yielded the same result. A Fisher’s exact test was applied to the number of interactions ≥20 minutes versus the number of interactions <20 minutes. *P < .05; **P < .01; ***P < .001. (B) The percentage of T-DC interactions ≥20 minutes, out of all analyzed interactions. White bars indicate nonretrogenic OVA-specific control T cells; gray bars indicate OVA-specific T cells retrogenically expressing WT CXCR4; black bars indicate OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. The statistical analysis refers to the Fisher’s exact test, as in (A). ctrl, nonretrogenic OVA-specific T cells; WT, OVA-specific T cells retrogenically expressing WT CXCR4; WHIM, OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. See also supplemental Videos 1-5. n.s., not significant.
WHIM-mutant CXCR4 impairs T-DC interactions in ex vivo lymph node slice cultures. DCs were either cognate antigen-pulsed (OVA) or unpulsed (no pept). (A) Duration of T-DC interactions within ex vivo lymph node slices imaged by 2-photon microscopy. The summary results of 2 videos per condition are shown. Each dot represents a single T-DC interaction (from left to right, n = 125, 101, 66, 21, 298, 291, 197, and 183). An independent experiment with the T-cell populations labeled with different dyes yielded the same result. A Fisher’s exact test was applied to the number of interactions ≥20 minutes versus the number of interactions <20 minutes. *P < .05; **P < .01; ***P < .001. (B) The percentage of T-DC interactions ≥20 minutes, out of all analyzed interactions. White bars indicate nonretrogenic OVA-specific control T cells; gray bars indicate OVA-specific T cells retrogenically expressing WT CXCR4; black bars indicate OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. The statistical analysis refers to the Fisher’s exact test, as in (A). ctrl, nonretrogenic OVA-specific T cells; WT, OVA-specific T cells retrogenically expressing WT CXCR4; WHIM, OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. See also supplemental Videos 1-5. n.s., not significant.
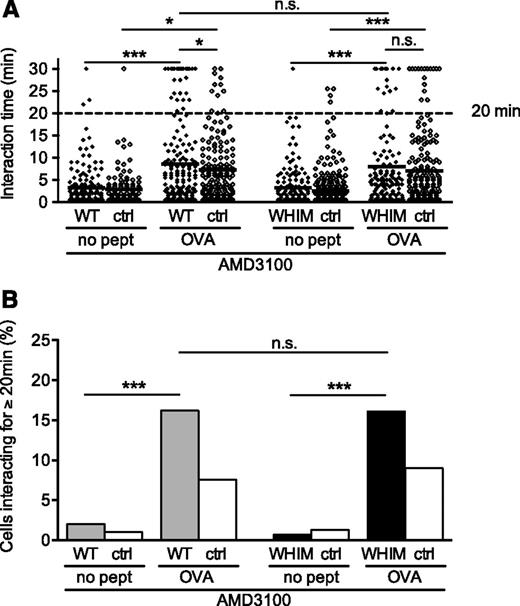
Because the observed impairment could be caused by defective development of the rgWHIM T cells, we repeated the aforementioned experiments in the presence of AMD3100, a CXCR4 inhibitor that is identical to the Food and Drug Administration– and European Medicines Agency–approved drug, plerixafor.25 In the presence of AMD3100, rgWHIM cells no longer differed from rgWT cells in the proportion of long-lasting interactions (Figure 3A; also plotted as % in Figure 3B; supplemental Video 6). Thus, the defective T-DC conjugate stability of rgWHIM cells was reversible within the lymph node slice and is therefore unlikely to be caused by upstream developmental defects. Although at very high concentrations not achievable in vivo with the maximum Food and Drug Adminstration–approved dose, AMD3100 may act as a CXCR7 agonist,26 the complete reversal of the phenotype caused by the mutant CXCR4 suggests that, in this context, AMD3100 does indeed act as a CXCR4 inhibitor. Cells expressing WT CXCR4 were expectedly unaffected, as it has been shown that WT CXCR4 signaling within the lymph node microenvironment is inconsequential for T-cell activation.18,27
WHIM-mutant CXCR4-mediated impairment of T-DC interactions in ex vivo lymph node slice cultures is reversed by the CXCR4 inhibitor AMD3100. DCs were either cognate antigen-pulsed (OVA) or unpulsed (no pept). (A) Duration of T-DC interactions within ex vivo lymph node slices imaged by 2-photon microscopy in the presence of 12.6 μM AMD3100. The summary results of 2 videos per condition are shown. Each dot represents a single T-DC interaction (from left to right, n = 150, 103, 167, 158, 152, 301, 137, and 178). A Fisher’s exact test was applied to the number of interactions ≥20 minutes versus the number of interactions <20 minutes. *P < .05; ***P < .001. (B) The percentage of T-DC interactions ≥20 minutes, out of all analyzed interactions. White bars indicate nonretrogenic OVA-specific control T cells; gray bars indicate OVA-specific T cells retrogenically expressing WT CXCR4; black bars indicate OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. The statistical analysis refers to the Fisher’s exact test, as in (A). ctrl, nonretrogenic control OVA-specific T cells; WT, OVA-specific T cells retrogenically expressing WT CXCR4; WHIM, OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. See also supplemental Video 6. n.s., not significant.
WHIM-mutant CXCR4-mediated impairment of T-DC interactions in ex vivo lymph node slice cultures is reversed by the CXCR4 inhibitor AMD3100. DCs were either cognate antigen-pulsed (OVA) or unpulsed (no pept). (A) Duration of T-DC interactions within ex vivo lymph node slices imaged by 2-photon microscopy in the presence of 12.6 μM AMD3100. The summary results of 2 videos per condition are shown. Each dot represents a single T-DC interaction (from left to right, n = 150, 103, 167, 158, 152, 301, 137, and 178). A Fisher’s exact test was applied to the number of interactions ≥20 minutes versus the number of interactions <20 minutes. *P < .05; ***P < .001. (B) The percentage of T-DC interactions ≥20 minutes, out of all analyzed interactions. White bars indicate nonretrogenic OVA-specific control T cells; gray bars indicate OVA-specific T cells retrogenically expressing WT CXCR4; black bars indicate OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. The statistical analysis refers to the Fisher’s exact test, as in (A). ctrl, nonretrogenic control OVA-specific T cells; WT, OVA-specific T cells retrogenically expressing WT CXCR4; WHIM, OVA-specific T cells retrogenically expressing WHIM-mutant CXCR4. See also supplemental Video 6. n.s., not significant.
The recruitment of WHIM-mutant CXCR4 to the immunologic synapse is disrupted by competing chemokine signals
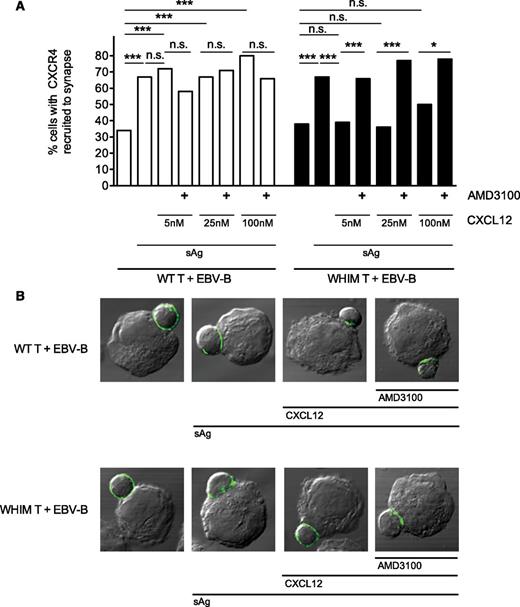
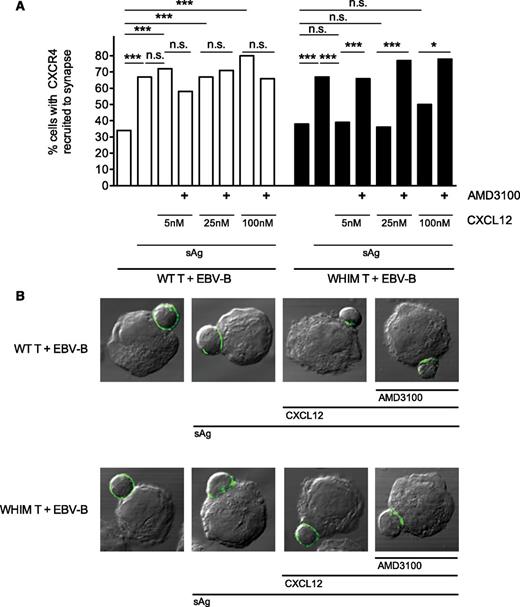
To gain insight on the mechanism that underlies the disruption of synapse stability by WHIM-mutant CXCR4, we examined the cellular distribution of the receptor during T-APC conjugate formation. We expressed the EGFP-fused WT or WHIM-mutant CXCR4 in primary CD4+ T cells from healthy donors that were allowed to form conjugates with superantigen-pulsed EBV-B cells, in the presence of competing external chemokine ligand at a wide range of concentrations. We then analyzed the recruitment of the fluorescent CXCR4 molecules to the T-APC synapse by confocal microscopy. WT CXCR4 (Figure 4A, white bars) was significantly recruited to the synapse when superantigen-pulsed EBV-B cells were used, as was previously shown.10 This recruitment was not significantly reduced by the presence of competing external CXCL12 ligand in the culture medium, a finding compatible with the attribution of lack of “dominance” over TCR signals to WT CXCR4-CXCL12 interactions.14 Interestingly, although WHIM-mutant CXCR4 (Figure 4A, black bars) was also significantly recruited to the synapse in the presence of superantigen, this recruitment was significantly reduced in the presence of competing CXCL12, suggesting a possible mechanistic explanation for the disruptive effect of the mutant receptor on immunologic synapse stability. Furthermore, mirroring our ex vivo findings, the concurrent presence of AMD3100 and CXCL12 in the culture medium was able to fully reverse the loss of mutant receptor recruitment to the synapse.
WHIM-mutant CXCR4 recruitment to the T-APC synapse is impaired by competing external CXCL12 and restored by AMD3100. (A) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM)–formed conjugates for 15′ with unpulsed or superantigen (sAg)-pulsed EBV-B cells, in the presence or absence of 5 nM to 100 nM CXCL12 and 12.6 μM AMD3100. The cells were fixed, imaged in confocal microscopy, and the RRI to the T-APC synapse for EGFP-CXCR4 was calculated. The graph displays the percentage of cells with CXCR4 recruited to the synapse (ie, with RRI above the mean RRI of control WT T cells incubated with unpulsed EBV-B). The RRI data set for all analyzed cells (n ≥40 per condition) is shown in supplemental Figure 3. Statistical analysis was performed on the proportion of cells displaying recruitment versus nonrecruitment of CXCR4 to the synapse. *P < .05; ***P < .001 (Fisher’s exact test). (B) Representative confocal microscopy images showing the recruitment of EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) to the T-APC synapse. n.s., not significant.
WHIM-mutant CXCR4 recruitment to the T-APC synapse is impaired by competing external CXCL12 and restored by AMD3100. (A) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM)–formed conjugates for 15′ with unpulsed or superantigen (sAg)-pulsed EBV-B cells, in the presence or absence of 5 nM to 100 nM CXCL12 and 12.6 μM AMD3100. The cells were fixed, imaged in confocal microscopy, and the RRI to the T-APC synapse for EGFP-CXCR4 was calculated. The graph displays the percentage of cells with CXCR4 recruited to the synapse (ie, with RRI above the mean RRI of control WT T cells incubated with unpulsed EBV-B). The RRI data set for all analyzed cells (n ≥40 per condition) is shown in supplemental Figure 3. Statistical analysis was performed on the proportion of cells displaying recruitment versus nonrecruitment of CXCR4 to the synapse. *P < .05; ***P < .001 (Fisher’s exact test). (B) Representative confocal microscopy images showing the recruitment of EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) to the T-APC synapse. n.s., not significant.
WHIM-mutant CXCR4 leads to aberrant in vivo T-cell priming and a delayed IgG response
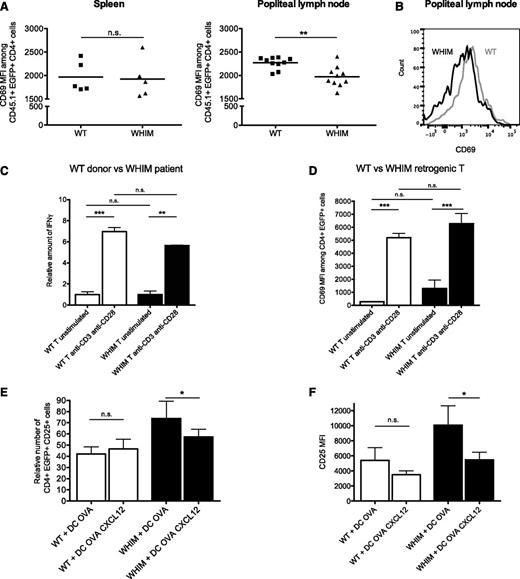
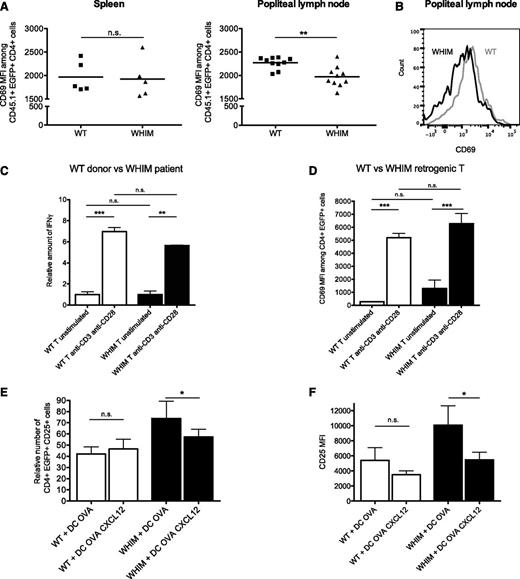
Even though not all stable T-APC conjugates would be expected to lead to the initiation of an immune response, a significant impairment in the stability of immunologic synapses is likely to cause aberrant T-cell activation in vivo.11,12 To test this in our system, we injected OVA peptide into the footpads of WHIM-mutant or WT CXCR4 retrogenic mice and examined their EGFP-expressing, retrogenic T cells in draining lymph nodes 12 hours after antigen administration. rgWT T cells displayed moderately, yet significantly, higher expression of the early T-cell activation marker CD6928 than rgWHIM T cells (Figure 5A, right panel and Figure 5B). In nondraining lymphoid compartments, such as the spleen (Figure 5A, left panel), no difference was observed. These results suggest that WHIM-mutant CXCR4-expressing T cells exhibit aberrant T-cell priming. To understand whether this result may depend on intrinsic defects of the TCR/CD3 complex of rgWHIM T cells, we performed in vitro activation experiments using anti-CD3 and anti-CD28 antibodies. T cells from WHIM-mutant retrogenic mice, as well as WHIM patient (G336X) T cells, displayed fully functional TCR signaling (Figure 5C-D). Next, we tried to reproduce in vitro the conditions present during T-cell activation in lymph nodes that may affect the stability of the synapse. T cells were stimulated with peptide-pulsed DCs in a transwell chamber (upper well), in the presence or in the absence of the “distracting” effects of CXCL12 (lower well). When CXCL12 was present in the lower chamber, rgWHIM, but not rgWT, T cells displayed a modest, although significant, reduction in activation (Figure 5E-F).
Aberrant responses of WHIM-CXCR4 T cells caused by reduced synapse stability. (A) WT or WHIM-CXCR4 retrogenic mice were immunized with OVA peptide in their hind footpads. Expression of early activation marker CD69 (anti-CD69 antibody mean fluorescence intensity) on retrogenic CD4+ T cells from the spleen or draining lymph nodes (popliteal) of immunized animals (n = 5) at 12 hours post immunization is shown. A normality test was performed followed by an unpaired Student t test: Popliteal, P = .0015; spleen, P = .9. (B) Representative histograms of CD69 expression by EGFP+ CD4+CD45.1+ rgWT or rgWHIM T cells in the popliteal lymph nodes of the animals analyzed. (C) Healthy donor or WHIM patient (G336X) CD4+ T cells were activated by anti-CD3– and anti-CD28–coated beads. IFNγ production was measured by ELISA at 48 hours. Normalized results are shown to enable comparison of different donors. (D) rgWT or rgWHIM T cells were activated in tissue culture plates by anti-CD3 and anti-CD28. CD69 expression was measured at 12 hours. Anti-CD69 antibody mean fluorescence intensity on CD4+EGFP+ rgWT or rgWHIM T cells is shown. **P < .01; ***P < .001 (1-way ANOVA and Tukey’s posttest). A representative experiment of 2 experiments is shown. (E) rgWT or rgWHIM T cells were placed with cognate antigen-pulsed (OVA) DC in the upper chamber of a transwell assay plate, and 25 nM CXCL12 was added or not to the lower chamber. The cells were incubated for 2 hours in the transwell plates before being transferred to serum-containing wells for 12 hours. The number of CD25+ cells among EGFP+CD4+ T cells in the pooled upper and lower chamber cells at the end of the incubation is shown in (E), normalized for differences in the transduction efficiency between the rgWT and rgWHIM donor mice. CD25 expression (anti-CD25 antibody mean fluorescence intensity) on EGFP+CD4+ T cells of the pooled upper and lower chamber cells at the end of the incubation is shown in (F). Both values are *P < .05 (repeated measures 1-way ANOVA). The experiment was performed twice, and the summary of results (mean ± SEM) is shown. It is noteworthy that, in the absence of antigen, the rgWHIM T cells displayed a higher baseline CD25 expression. n.s., not significant.
Aberrant responses of WHIM-CXCR4 T cells caused by reduced synapse stability. (A) WT or WHIM-CXCR4 retrogenic mice were immunized with OVA peptide in their hind footpads. Expression of early activation marker CD69 (anti-CD69 antibody mean fluorescence intensity) on retrogenic CD4+ T cells from the spleen or draining lymph nodes (popliteal) of immunized animals (n = 5) at 12 hours post immunization is shown. A normality test was performed followed by an unpaired Student t test: Popliteal, P = .0015; spleen, P = .9. (B) Representative histograms of CD69 expression by EGFP+ CD4+CD45.1+ rgWT or rgWHIM T cells in the popliteal lymph nodes of the animals analyzed. (C) Healthy donor or WHIM patient (G336X) CD4+ T cells were activated by anti-CD3– and anti-CD28–coated beads. IFNγ production was measured by ELISA at 48 hours. Normalized results are shown to enable comparison of different donors. (D) rgWT or rgWHIM T cells were activated in tissue culture plates by anti-CD3 and anti-CD28. CD69 expression was measured at 12 hours. Anti-CD69 antibody mean fluorescence intensity on CD4+EGFP+ rgWT or rgWHIM T cells is shown. **P < .01; ***P < .001 (1-way ANOVA and Tukey’s posttest). A representative experiment of 2 experiments is shown. (E) rgWT or rgWHIM T cells were placed with cognate antigen-pulsed (OVA) DC in the upper chamber of a transwell assay plate, and 25 nM CXCL12 was added or not to the lower chamber. The cells were incubated for 2 hours in the transwell plates before being transferred to serum-containing wells for 12 hours. The number of CD25+ cells among EGFP+CD4+ T cells in the pooled upper and lower chamber cells at the end of the incubation is shown in (E), normalized for differences in the transduction efficiency between the rgWT and rgWHIM donor mice. CD25 expression (anti-CD25 antibody mean fluorescence intensity) on EGFP+CD4+ T cells of the pooled upper and lower chamber cells at the end of the incubation is shown in (F). Both values are *P < .05 (repeated measures 1-way ANOVA). The experiment was performed twice, and the summary of results (mean ± SEM) is shown. It is noteworthy that, in the absence of antigen, the rgWHIM T cells displayed a higher baseline CD25 expression. n.s., not significant.
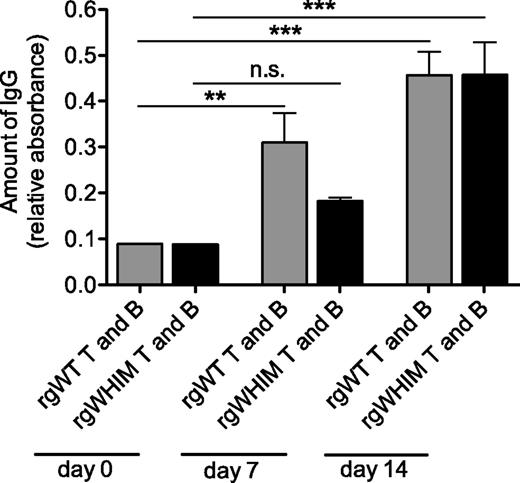
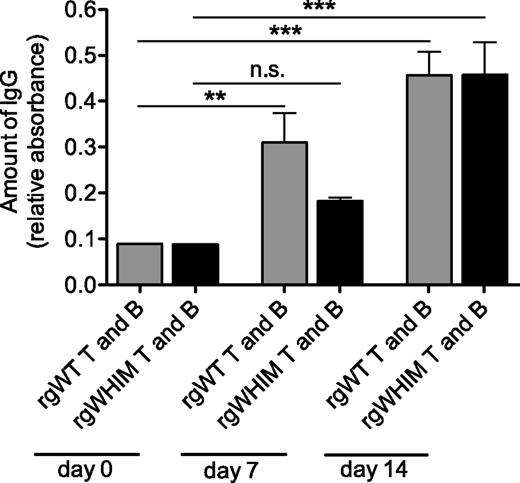
To confirm the physiologic relevance of our findings, we assessed whether the aberrant T-cell priming could lead to T cell–dependent early activation defects that characterize patients with WHIM syndrome, such as the delay in IgG responses found in one study.1 To this end, we transferred 25 × 103 OVA-specific rgWT or rgWHIM CD4+ T cells into RAG1−/− mice, which are devoid of functional T and B cells. To provide antibody-producing cells, we cotransferred 6 × 106 T-depleted lymphocytes from WT syngenic donors. The recipient mice were immunized intraperitoneally with OVA coupled to the hapten NP. WT B cells that can recognize NP29 will take up NP-OVA and present peptides from both NP and OVA to T cells. Costimulation of the B cells by the transferred OVA-specific retrogenic T cells, which will represent the vast majority of the T cells present, will enable B cells to undergo class-switch recombination and produce IgG antibodies against NP. As expected from previous studies,29 by day 7 after immunization, recipients of rgWT T cells displayed a significant increase of anti-NP IgG in their sera (Figure 6, gray bars). However, this failed to occur in recipients of rgWHIM T cells, which did not result in a significant IgG response (Figure 6, black bars), remaining at levels found in T cell–depleted controls (data not shown). However, by day 14, both groups of recipients displayed high IgG titers (Figure 6, day 14) and remained not significantly different in subsequent time points up to 6 months (data not shown). Thus the expression of WHIM-mutant CXCR4 on T cells leads to a delay in IgG responses, mirroring the delayed IgG switching observed in WHIM.1
WHIM-CXCR4–expressing retrogenic T cells led to a delay in IgG antisera production. RAG1−/− recipient mice (n = 5 per group) were reconstituted with retrogenic WT (rgWT) or WHIM (rgWHIM) T cells specific for OVA, as well as T-depleted splenocytes, and immunized with NP-OVA. The bars indicate anti-NP IgG titers in the sera at various time points after immunization. **P < .01; ***P < .001 (2-way ANOVA and Bonferroni posttests). n.s., not significant.
WHIM-CXCR4–expressing retrogenic T cells led to a delay in IgG antisera production. RAG1−/− recipient mice (n = 5 per group) were reconstituted with retrogenic WT (rgWT) or WHIM (rgWHIM) T cells specific for OVA, as well as T-depleted splenocytes, and immunized with NP-OVA. The bars indicate anti-NP IgG titers in the sera at various time points after immunization. **P < .01; ***P < .001 (2-way ANOVA and Bonferroni posttests). n.s., not significant.
Discussion
WHIM syndrome is characterized by symptoms affecting different stages of the adaptive immune response, the etiology of which is not clearly understood. Deficiencies in the late stages of adaptive responses include memory B-cell lymphopenia, an inability to maintain long-term IgG antibody titers after immunization,2 and recurring infections.3 It has been proposed1 that these defects may be caused, in similarity to the aberrant neutrophil homing, by impaired memory lymphocyte homing, a hypothesis supported by the panleukopenia in the peripheral blood of WHIM patients.2,25 Conversely, the delay in mounting IgG antibody responses observed in a patient studied by Mc Guire and colleagues1 involved a T cell–dependent, B cell–mediated process that occurred at the early stages of the adaptive response. Our study offers a novel mechanistic explanation, at the heart of adaptive immune response initiation, for this observation. We demonstrate that immunologic synapse stability is impaired in the presence of WHIM-mutant CXCR4. It is tempting to speculate that this is caused by the lack of mutant receptor recruitment to the synapse, which, combined with the hyperfunctional nature2,5 of WHIM-mutant CXCR4 and the presence of CXCL12 in the lymph node,21 disrupts the TCR-mediated, synapse-promoting signals. This does not preclude the parallel existence of additional mechanisms, such as the proposed CXCR4-mediated aberrations in lymph node architecture,1 which are in agreement with recent data from a mouse model of WHIM,30 even though studies of hypogammaglobulinemia have yet to be performed in the latter.31 Given the wide expression range of CXCR4, it is likely that the combined effect of the aforementioned mechanisms, including the defect in synapse stability described here, contribute to the complex symptoms of the WHIM syndrome.
In the physiological milieu where T-APC immunologic synapses form, “dominant” chemokine signaling has been proposed to inhibit stable synapse formation, based on results of in vitro experimentation.14,15 CXCL12 interacting with T cells expressing WT CXCR4 was found not to be a “dominant” chemokine.13 Rather, CXCR4 is recruited to the immunologic synapse itself, where it enhances the activation of the T cell after receiving chemokine ligand produced by the APC.10 Exogenous chemokine signals that are not derived from the APC but from the surrounding lymph node microenvironment, where the chemokine is present,21 did not affect T-APC synapse formation in WT CXCR4-expressing cells in our studies, in agreement with results showing the lack of a role for WT CXCR4-CXCL12 on T-cell activation.18,27 Yet our in vitro and ex vivo results show that WHIM-mutant CXCR4 enables CXCL12 to act as a distracting, “dominant” chemokine. This appears to occur via the disruption of the recruitment of WHIM-mutant CXCR4 to the synapse. Both the disruption of the receptor recruitment to the synapse and the “distracting” of stable synapse formation appear to be reversible by AMD3100 treatment, which has recently been proposed as a therapeutic agent for the WHIM syndrome.25 Importantly, our findings also provide the first physiological, ex vivo evidence that chemokines and their receptors may control the stability of T-DC interactions in lymph nodes. The data suggest the existence of a delicate equilibrium between adhesive and chemoattractant forces operating in lymph nodes during T-cell priming, allowing enough motility for T-cell repertoire scanning while ensuring the formation of long-lasting conjugates once a cognate T-APC pair is formed. Variations in this equilibrium, such as those caused by the hyperfunctional mutant CXCR4 of patients with WHIM,3 may lead to impaired stability of the immunologic synapse and consequently contribute to an aberrant adaptive immune response.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The retroviral system m5p was kindly provided by Dr Randow (Medical Research Council Laboratory of Molecular Biology, Cambridge, United Kingdom). The authors thank the WHIM patients and healthy volunteers for their participation in the study, J. Stein for essential technical advice, R. Bonecchi and E. M. Borroni for help with validation of the CXCR4 constructs, C. Tadokoro for advice on data analysis, A. Anselmo and C. Buracchi for assistance with FACS sorting and analysis, and S. Casola and A. Mantovani for helpful suggestions.
M.K. was supported by a Federation of the Societies of Biochemistry and Molecular Biology long-term post-doctoral fellowship. The work was supported by grants from Telethon (GGP07134 and 10170) (A.V. and R.B.), the E-rare (WHIMPath) and SYBILLA European Commission project (A.V.), CARIPLO 2008/2279 (M.K. and R.B.) and Fondo per gli Investimenti della Ricerca di Base RBFR10HP97 (M.K.), and Fondazione Cassa di Risparmio delle Provincie Lombarde grant 5808/2007 (A.S. and F.A.).
Authorship
Contribution: M.K., A.S., and A.V. designed the experiments; M.K., A.E.T. and G.R. performed the experiments and analyzed the data; F.A. performed the 2PM imaging; L.T. and R.B. prepared the initial constructs and provided patient samples; and M.K. and A.V. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marinos Kallikourdis, Humanitas Clinical and Research Center, Via Manzoni 56, Rozzano (Milano) 20089, Italy; e-mail: marinos.kallikourdis@humanitasresearch.it.
References
Author notes
M.K. and A.E.T. contributed equally to this study.

![Figure 1. WHIM-mutant CXCR4 impairs T cell–B cell conjugate stability. (A) Primary CD4+ T cells from healthy WT donor or WHIM-patient peripheral blood formed conjugates for 15′ with superantigen (sAg)-pulsed, labeled primary B cells from a healthy allogenic donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. The migrated T cells were analyzed by FACS and the number of T cells migrated for each condition is shown. *P < .05 (1-way analysis of variance [ANOVA] and Tukey’s posttest). Experiment performed twice, summary of results (mean ± SEM) shown. (B) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) formed conjugates for 15′ with sAg-pulsed primary B cells from the same donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. Migrated EGFP+ T cells were analyzed as described in (A). **P < .01 (1-way ANOVA and Tukey’s posttest). The experiment was performed twice, and results (mean ± SEM) from representative experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/5/10.1182_blood-2012-10-461830/4/m_666f1.jpeg?Expires=1769209123&Signature=UFRZvXFb4Bb3Odn2lXg171-tjQAEktBZlPlmNGMHRtICKfFd3g1T3mEcoqTnIDCX7pOS6YQDjcM6Xe-meXq7TWRMOQA9mqUrmYeOmNj0uE6WBf9HHSP-pECg0QtWwsADLiN-IMkG0GdGLM6iXBwvHLYRzOXood-1rSrJ10Hk~SsPhrEuno~I09rwEzEI4Fo7fv4v0vEBBtW3mrk5XjF2fjDdWaTgAVfEff8058j3Zc63DCt9hzqxP2mayL0pIHQTonPoFf8HD4lQrXOaHLDugy8ucS2d61cpbZA5GNC2UT~aYyxcvB~9o0BJ63Zz0AP4233ljXopHJy82-vqdFbiBQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 1. WHIM-mutant CXCR4 impairs T cell–B cell conjugate stability. (A) Primary CD4+ T cells from healthy WT donor or WHIM-patient peripheral blood formed conjugates for 15′ with superantigen (sAg)-pulsed, labeled primary B cells from a healthy allogenic donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. The migrated T cells were analyzed by FACS and the number of T cells migrated for each condition is shown. *P < .05 (1-way analysis of variance [ANOVA] and Tukey’s posttest). Experiment performed twice, summary of results (mean ± SEM) shown. (B) Primary CD4+ T cells from healthy donor peripheral blood transfected with EGFP-CXCR4 (WT) or EGFP-CXCR4 (WHIM) formed conjugates for 15′ with sAg-pulsed primary B cells from the same donor. The conjugates were allowed to migrate toward CXCL12 in a transwell filter, allowing the migration of single cells only. Migrated EGFP+ T cells were analyzed as described in (A). **P < .01 (1-way ANOVA and Tukey’s posttest). The experiment was performed twice, and results (mean ± SEM) from representative experiments are shown.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/5/10.1182_blood-2012-10-461830/4/m_666f1.jpeg?Expires=1770003109&Signature=DwOeKXaN08RrUyBdYXR~EHisRDRLjNmLETG8ViDmOIPWEyL3cNmoYhN7OVxt6xq7CN7yWT0pQFkou~n3xQJIQzjvaWsrOL2-IPUaMLuxq4hhN1uCyfntoYDQI2hgh9xyXKZFr0hF3WfDisHpv2bpW-bxTh9cHkxxWH9YyqveyPrURqEMjMNEwO9pfH~RlHJl15QM3gLvAJ0vmK3roMozaglbRW3orL50se0gCG9h30pHFWB~XirwI44CzpLfMOKbg1I6FS-6Mjecji0kWPbeSH0Ge-bj3eyws2t1nsHfyGRTu6odAVesOvwj4-HL-9Pm2wJKK6SQv74aech81Wpjlg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)