Key Points
DLBCL patients carrying the HLA-B44 supertype have a worse progression-free and overall survival after R-CHOP-like treatment.
The HLA-DRB1*01 allele increases the risk of DLBCL development.
Abstract
Diffuse large B-cell lymphoma (DLBCL) is an aggressive disease influenced by genetic and environmental factors. The role of the HLA system in tumor antigen presentation could be involved in susceptibility and disease control. We analyzed the phenotypic frequencies of HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1 in 250 DLBCLs, comparing them with 1940 healthy individuals. We also evaluated the influence of HLA polymorphisms on survival in those patients treated with curative intention using cyclophosphamide, doxorubicin, vincristine, and prednisolone (CHOP)-like regimen without (n = 64, 26%) or with (n = 153, 61%) rituximab. DLBCL patients have a higher phenotypic frequency of HLA-DRB1*01 (29% vs 19.5%, P = .0008, Pc = .0104) and a lower frequency of HLA-C*03 (6.4% vs 17.9%, P < .0005, Pc = .007) compared with healthy individuals. Irrespective of the age-adjusted International Prognostic Index, those patients receiving a CHOP-like plus rituximab regimen and carrying the HLA-B44 supertype had worse 5-year progression-free (54% vs 71%, P = .019) and 5-year overall (71% vs 92%, P = .001) survival compared with patients without this supertype. Our data suggest that some HLA polymorphisms influence the development and outcome of DLBCL, allowing the identification of an extremely good-risk prognostic subgroup. However, these results are preliminary and need to be validated in order to exclude a possible population effect.
Introduction
Several genetic polymorphisms have been associated with susceptibility or prognosis in various B-cell non-Hodgkin lymphoma (B-NHL) subtypes.1,2 In recent years, genome-wide association studies have identified 6p21.3 as a risk region for susceptibility of different lymphomas, such as follicular lymphoma3-5 or Hodgkin lymphoma.6,7 The HLA system, located in this region, plays a key role in antitumor immune responses and lymphoma-cell apoptosis8 and so may be essential for neoplasia control. Previous studies have shown a relationship between HLA polymorphisms and susceptibility to certain hematologic malignancies such as chronic lymphocytic leukemia, multiple myeloma, and acute lymphoblastic leukemia.9-11 However, there is little information about the relationship between HLA polymorphisms and susceptibility to developing B-NHL or their outcomes.12-16 Focusing on diffuse large B-cell lymphoma (DLBCL), some associations between HLA specificities and this B-NHL subtype have been described, as well as with other genetic polymorphisms. Shorter progression-free survival (PFS) and overall survival (OS) have been observed in DLBCL patients lacking the HLA-DR2 or carrying TNF-308A.13 In addition, OS is shorter in those patients carrying the C*07-B*08-LTA+252G-TNF-308A haplotype14 or the HLA-C*07:01.16 However, these studies considered patients treated before the introduction of the anti-CD20 monoclonal antibody, rituximab. Because, at present, almost all patients with DLBCL receive rituximab combinations as first-line therapy, the current influence of HLA polymorphisms on DLBCL susceptibility or outcome remains to be elucidated.
In the present study, we have evaluated whether HLA class I (A, B, and C) and class II (DRB1 and DQB1) polymorphisms are associated with lymphoma incidence or outcome in a large series of DLBCL patients, including 153 cases treated with cyclophosphamide, doxorubicin, vincristine, and prednisolone (CHOP)-like regimens plus rituximab as first-line therapy. We report new findings that provide further evidence of this association, supporting the hypothesis of an important role for the HLA system in DLBCL risk and prognosis, especially when patients are treated in the rituximab era.
Patients and methods
Patient characteristics and immunohistochemistry
We analyzed 250 consecutive patients diagnosed with de novo DLBCL according to the 2008 World Health Organization classification.17 The clinical characteristics of the patients are described in Table 1. Their median age was 56 years, ranging from 13 to 87 years. Fifty-two percent of the patients were male. The age-adjusted International Prognostic Index (aaIPI)18 score was ≥2 in 58% of the patients. In 116 samples, immunostaining with antibodies to BCL-6, CD10, and MUM1 could be performed, which allowed patients to be classified into 2 biological subtypes according to the Hans criteria19 : germinal center B-cell–like (45%) and nongerminal center B-cell–like (55%) DLBCL. Complete clinical and therapeutic information data were available for 233 patients, 224 of whom received a treatment with curative intention. Most of the patients received a CHOP or CHOP-like regimen as first-line treatment (97%), 153 of them (68%) with rituximab (see Table 1). A total of 107 of these patients (48%) were included in Spanish Lymphoma/Autologous Bone Marrow Transplant Study Group (GELTAMO) protocols for de novo DLBCL.20-22
The control population for HLA-A, HLA-B, and HLA-DRB1 loci consisted of 1940 healthy donor individuals from our geographical region,23 matched with the cases by gender, age, and ethnicity. In addition, HLA typing was extended to HLA-C and HLA-DQB1 in 200 of these donors.
This study was approved by the local ethics review committee in accordance with Spanish law. Prior informed consent was obtained from all participants in accordance with the Declaration of Helsinki.
DNA extraction and HLA typing
DNA from peripheral blood samples was isolated using the DNAzol reagent (MRC, Cincinnati, OH)24 or MagNA Pure LC system (Roche Diagnostics GmbH, Mannheim, Germany). HLA class I (A, B, and C) and class II (DRB1 and DQB1) typing at low-resolution level (2 digits) was carried out using the polymerase chain reaction reverse sequence-specific oligonucleotide and Luminex XYP technology (Tepnel Lifecodes Corporation, Stamford, CT), according to the standards of the European Federation of Immunogenetics (http://www.efiweb.org). Polymerase chain reaction sequence-specific primer methods (Dynal Biotech, Oslo, Norway) were also used as necessary for HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1 loci. Homozygosis was confirmed by familial studies or by using 2 alternative methods. Many HLA alleles have overlapping structural and functional features through shared peptide-binding pockets and thus can be clustered into distinct functional groups, known as supertypes. In addition to phenotype frequencies, the HLA polymorphisms were categorized into previously defined supertypes.25,26
Definitions and statistical analyses
Allele frequencies were estimated by an expectation-maximization algorithm using the Arlequin software package (version 3.5.1.2).27 The Hardy-Weinberg equilibrium was tested by applying a modified hidden Markov chain with the 100 000 step-length approach and 10 000 dememorization steps, as implemented in the Arlequin program. Allele and phenotype frequencies between populations were compared with the 2-sided Fisher’s exact test using GraphPad Prism 4.0 (GraphPad Software, San Diego, CA). The strength of associations was estimated by odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated by the Cornfield methods (values of P < .05 were considered statistically significant). P values were Bonferroni corrected (Pc) to take into account multiple testing.
End points were assessed on the date of the last patient contact; the most recent follow-up was in November 2012. The PFS was calculated from diagnosis until lymphoma relapse or progression or death for any cause, according to International Working Group criteria.28 OS was calculated from diagnosis until death from any cause. For both PFS and OS, surviving patients were censored at last follow-up.
The following variables were included in the survival analysis: treatment, sex, β2 microglobulin, C-reactive protein, aaIPI and International Prognostic Index (IPI) scores and their respective individual factors (performance status Eastern Cooperative Oncology Group ≥2, high lactate dehydrogenase levels, Ann Arbor status, age >60 years, >1 extranodal sites), cell of origin according Hans’ classification, and presence of the various HLA polymorphisms. For this purpose, the 2-sided log-rank test was used to test the univariate association between variables. Survival curves were plotted according to the Kaplan-Meier method using SPSS (version 15.0; SPSS, Chicago, IL). Subsequently, all variables for which there was some indication of a significant association with DLBCL in univariate tests (P < .1) were examined in the multivariate analysis using the stepwise Cox regression (enter) model to estimate hazard ratios (HRs) and 95% CIs. Differences were considered to be statistically significant for values of P < .05. Survival analysis was performed only in the patients for whom clinical data were available and who were treated with curative intention (n = 224). Because rituximab combinations are the current standard first-line treatment of DLBCL patients, univariate and multivariate analyses were focused on rituximab-treated patients (n = 153).
Results
HLA association with DLBCL development
HLA polymorphism frequencies in DLBCL patients appeared to be in Hardy-Weinberg equilibrium in all cases. The HLA-A, B, and DRB1 allele frequencies of the control population from our geographic region have been described elsewhere.23 The HLA-C and DQB1 polymorphism frequencies were similar to those of other Iberian populations (data not shown).
Phenotypic frequencies differed significantly between DLBCL patients and healthy control individuals (supplemental Table 1). The phenotypic frequency of HLA-DRB1*01 was significantly higher in DLBCL patients than in the control population (29% vs 19.5%, P = .0008, OR = 1.69, 95% CI = 1.25-2.28). This difference remained statistically significant even when adjusted for multiple testing (Pc = .0104). In addition, we observed a lower incidence of the HLA-C*03 phenotype in DLBCL patients compared with controls (6.4% vs 17.9%, P = .0005, Pc = .007, OR = 0.31, 95% CI = 0.16-0.62). Finally, HLA-DRB1*15 (13.7% vs 19.8%, P = .03) and HLA-B*51 (20.9% vs 15.9%, P = .07) polymorphisms slightly differed between DLBCL patients and controls, although statistical significances were lost after Bonferroni correction. No other phenotypic frequencies significantly differed between the patient and control groups.
HLA and clinical outcome in the whole series
With a median follow-up of 81 months (range, 11-255 months), the actuarial 5-year PFS and 5-year OS in the whole series were 61% and 78%, respectively.
With respect to HLA polymorphisms, patients with HLA-B*18 specificity showed a shorter PFS (35% vs 63% at 5 years, P = .002) and OS (53% vs 82% at 5 years, P = .0005) compared with the other DLBCL patients (supplemental Figure 1). Differences in OS observed for HLA-B*44 (69% vs 81% at 5 years, P = .08) and HLA-DRB1*04 (88% vs 75% at 5 years, P = .07) were not statistically significant.
Our data reveal that HLA-B*18 and HLA-B*44 seem to influence the clinical outcome of DLBCL. Interestingly, these 2 specificities are members of the HLA-B44 supertype, which includes the HLA-B*18, HLA-B*37, HLA-B*40, HLA-B*41, HLA-B*44, HLA-B*45, and HLA-B*50 alleles.25,26 Consequently, we wanted to analyze the role of the HLA-B44 supertype in DLBCL prognosis. Patients carrying any HLA allele of the HLA-B44 supertype showed a shorter OS (69% vs 86% at 5 years, P = .004) than those without the supertype (supplemental Figure 1).
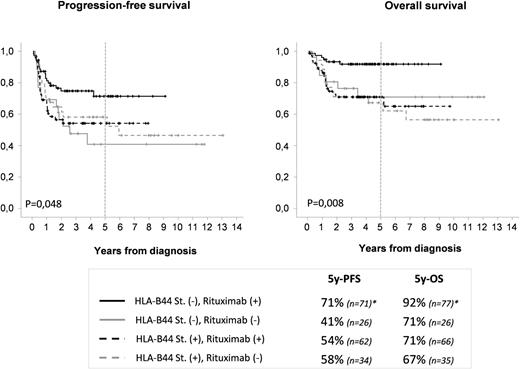
We analyzed the effect of the treatment considering the HLA phenotype. First, we analyzed the observed frequencies of the HLA phenotypes by treatment or by the inclusion in a clinical trial, and no significant differences between groups were observed (data not shown). We then analyzed the effect of the treatment by HLA-B44 supertype. Patients carrying the HLA-B44 supertype, independent of the treatment with or without rituximab, did not show significant differences in PFS (54% vs 58% at 5 years, P > .05) and OS (71% vs 67% at 5 years, P > .05; Figure 1). By contrast, those patients carrying other HLA alleles who did not receive rituximab-based regimens showed a shorter PFS (41% vs 71% at 5 years, P = .013) and OS (71% vs 92% at 5 years, P = .012) than those receiving rituximab (Figure 1).
Progression-free survival and OS in the whole series by treatment and HLA-B44 supertype. Asterisk indicates a significant difference compared with other combinations (P < .05 for PFS at 5 years and P < .05 for OS at 5 years). St, supertype.
Progression-free survival and OS in the whole series by treatment and HLA-B44 supertype. Asterisk indicates a significant difference compared with other combinations (P < .05 for PFS at 5 years and P < .05 for OS at 5 years). St, supertype.
We checked the potential interaction of HLA phenotypes in PFS and OS considering dose-effect (heterozygosity/homozygosity) of HLA-B*18 or HLA-B*44 as well as the simultaneous presence of 2 specificities of the HLA-B44 supertype. Our results do not seem to detect any interaction between these specificities in DLBCL outcome.
HLA and clinical outcome in the rituximab group
With a median follow-up of 56 months (range, 11-136 months), the actuarial 5-year PFS and 5-year OS of rituximab-treated patients were 65% and 83%, respectively.
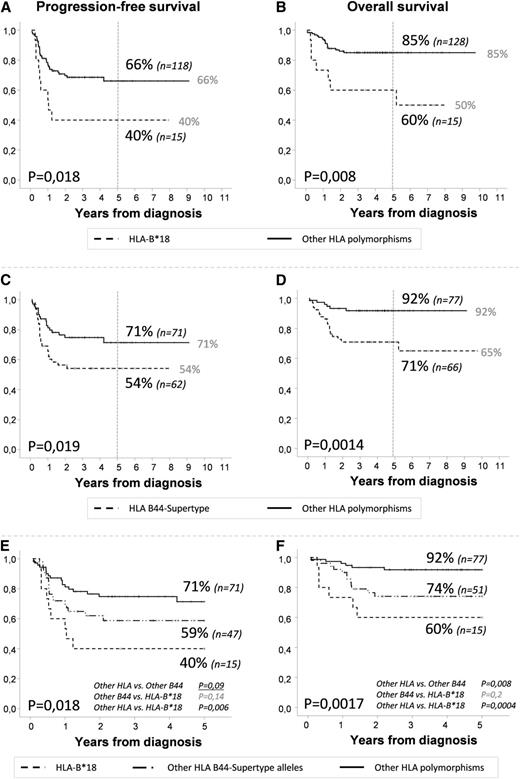
As in the whole series, patients with the HLA-B*18 specificity had a poor outcome: a PFS of 40% vs 66% at 5 years (P = .018) and an OS of 60% vs 85% at 5 years (P = .008) for patients with and without this specificity, respectively (Figure 2; Table 2). Similarly, the HLA-B*44 specificity was associated with shorter PFS (52% vs 67% at 5 years, P = .06) and OS (69% vs 87% at 5 years, P = .02). Finally, differences in HLA-DRB1*04 (93% vs 79% at 5 years, P = .09) were not statistically significant. We have analyzed different biological and clinical variables in the subgroup of patients bearing the HLA-B*18 allele and the HLA-B44 supertype, including cell of origin and β2 microglobulin. No major differences were found (see supplemental Table 2).
Progression-free survival and OS in patients receiving CHOP or CHOP-like plus rituximab by the HLA. (A,B) Presence of HLA-B*18 vs other polymorphisms. (C,D) Presence of HLA-B44 supertype vs other polymorphisms. (E,F) Presence of HLA-B*18 vs other HLA-B44 supertype polymorphisms vs other HLA polymorphisms.
Progression-free survival and OS in patients receiving CHOP or CHOP-like plus rituximab by the HLA. (A,B) Presence of HLA-B*18 vs other polymorphisms. (C,D) Presence of HLA-B44 supertype vs other polymorphisms. (E,F) Presence of HLA-B*18 vs other HLA-B44 supertype polymorphisms vs other HLA polymorphisms.
When we analyzed the outcome of the patients by HLA-B44 supertype we found a shorter PFS (54% vs 71% at 5 years, P = .019) and OS (71% vs 92% at 5 years, P = .001) in those patients carrying any allele of the HLA-B44 supertype (Figure 2; Table 2).
To determine whether the results obtained with the HLA-B44 supertype directly depended on the HLA-B*18 polymorphism, we assessed the effect of HLA in 3 groups: group a, patients bearing the HLA-B*18 polymorphism (n = 15); group b, patients bearing any allele of the HLA-B44 supertype except HLA-B*18 (n = 51); and group c, patients bearing “other HLA alleles” (n = 77). The 3 groups had different 5-year PFS (40%, 59%, and 71%, respectively, P = .018) and OS at 5 years (60%, 74%, and 92%, respectively, P = .0017), as shown in Figure 2.
We then evaluated the prognostic value of the IPI in our series. Patients with high IPI showed a worse PFS (56% vs 74%, P = .08) and OS (88% vs 82%, P = .2), although the differences were not statistically significant. Since most of the patients in our series are <60 years, we analyzed the aaIPI. We found that those patients with aaIPI ≥ 2 showed a worse PFS (60% vs 78%, P = .018) and OS (81% vs 91%, P = .09).
In the multivariate analysis, the presence of HLA-B*18 (P = .002, OR = 4.0; 95% CI = 1.67-9.57), the presence of any allele of the HLA-B44 supertype except HLA-B*18 (P = .052, OR = 2.0; 95% CI = 0.99-4.03), and aaIPI ≥ 2 (P = .006, OR = 2.7; 95% CI = 1.32-5.52) were the only independent variables with a significant influence on PFS. The same 3 variables were of independent prognostic value for OS (P = .001, OR = 7.6; 95% CI = 2.18-26.66; P = .017, OR = 3.7; 95% CI = 1.27-10.97; P = .049, OR = 2.8; 95% CI = 1.01-7.74, respectively), as shown in Table 2.
Discussion
The HLA system plays an essential role in immunologic surveillance.29 The different abilities of certain alleles to efficiently present tumor antigens or the deregulation of allelic expression could result in the tumor cells escaping T-cell and natural killer cell recognition.8,30-35
In the present study, we analyzed the influence of the HLA-A, B, C, DRB1, and DQB1 polymorphisms on the development of 250 DLBCL patients, the largest series reported to date. In addition, we describe for the first time the role of HLA polymorphisms in the prognosis of DLBCL patients receiving rituximab-based regimens as first-line treatment. Our results show that the presence of the HLA-DRB1*01 and the absence of HLA-C*03 polymorphism are associated with susceptibility to DLBCL, while the HLA-B44 supertype, especially the presence of HLA-B*18 and HLA-B*44 polymorphisms, have an independent influence on survival.
The HLA system has been related to susceptibility to several hematologic and nonhematologic diseases,9-11,36 including a variety of HLA polymorphisms associated with B-NHL development and outcome.12-16 However, this feature has not been extensively studied specifically in DLBCL, although some data suggest an association between HLA subtypes and disease susceptibility (ie, a higher incidence of HLA-DRB1*04:01 allele in this lymphoma subgroup). Moreover, previous studies including survival analyses were limited and performed before the rituximab era, and therefore their conclusions cannot be applied to the current standard of care.14,16
Our findings indicate a higher HLA-DRB1*01 frequency in DLBCL patients. Interestingly, a higher incidence of HLA-DRB1*01 has been described in other B-cell lymphoproliferative disorders such as follicular lymphoma4,15 and smoldering multiple myeloma,10 indicating a possible role for HLA-DRB1*01 in controlling the tumor B-cell clone. In this way, a higher incidence of this specificity was also found in some autoimmune disorders such as rheumatoid arthritis37,38 and Crohn disease,37,39 which have also been linked to higher susceptibility to DLBCL.40
We also found a lower frequency of HLA-C*03 in DLBCL. The HLA-C*03 belongs to the HLA-C group 1 (HLA-C1) and is a ligand of the activating natural killer immunoglobulin-like receptor (KIR) KIR2DS2 gene and the inhibitory KIR2DL2 and KIR2DL3 genes.41 Some studies have related the combination of HLA and KIR genes to susceptibility to or outcome of various infectious and autoimmune disorders.42-45 For example, homozygosity for both HLA-C1 and KIR2DL3 is related to the spontaneous clearance of hepatitis C virus infection.45 Considering these data, we hypothesize that those patients carrying HLA-C*03 could develop more efficient antitumor activity by natural killer cells, probably influenced by their combination with KIR genes. Further analysis of the KIR genotypes combined with HLA typing of DLBCL patients should be done to address this question.
One of the important outcomes of our study is the description of the influence of the HLA-B44 supertype (and especially the HLA-B*18 polymorphism) on the prognosis of DLBCL patients. This influence is particularly evident in those patients receiving rituximab-based regimens and is independent of aaIPI, which is an important strength of this study. Although IPI is the standard prognostic index, we used aaIPI because most of the patients in our study are young and most of the elderly patients received an intensified treatment. Furthermore, age and number of extranodal sites (included in the IPI but not in the aaIPI) were not statistically significant in PFS and OS in our series. Moreover, several studies as in the present have previously shown the utility of aaIPI in patients >60 years in the rituximab era.46,47 It is interesting to note that the presence of the HLA-B44 supertype characterizes a group of patients who do not respond to rituximab in which novel strategies (ie, novel monoclonal antibodies) should be tested. On the other hand, the absence of the HLA-B44 supertype is capable of identifying an extremely good-risk prognostic subgroup that has a cure rate of >90% with current therapeutic strategies. This should be taken into account in the design of future trials with new drugs, because the goal with these patients should be more focused on toxicity improvement rather than on increasing efficacy.
In chronic myelogenous leukemia patients, the HLA-B*18 polymorphism has been associated with poor response and a trend toward shorter survival.48 Moreover, HLA-B*44 is more easily lost than other HLA polymorphisms in some types of solid tumor,49 which indicates that this allele may have a central role in the mechanisms of immune escape. An alternative explanation for these differences in prognosis is that the HLA-B44 supertype does not efficiently present common tumor peptides to the cytolytic T lymphocytes, leading to a poor response. Our data indicate that although patients carrying any HLA-B44 supertype allele are not more susceptible to developing DLBCL, tumor cells for patients with these HLA variants may easily escape the immune surveillance, resulting in poor disease control. However, although our study suggests that the HLA typing of patients with DLBCL could be of interest to stratify their risk of progression and survival, it must be taken into account that the present results are preliminary and need further validation. We have thus designed a study to evaluate prospectively HLA-B*18 and the HLA-B44 supertype as part of the trials currently conducted by the GELTAMO Spanish group.
In conclusion, our results suggest a role for HLA in DLBCL susceptibility and prognosis and are consistent with the increasing evidence of the influence of 6p21 on B-NHL development and, in particular, on DLBCL. These findings could be helpful in the future classification, treatment, and monitoring of DLBCL patients.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Alicia Antón, Felicitación García, Montserrat Hernández-Ruano, Rebeca Maldonado, Mercedes Jiménez, Alejandra Martín, and Isabel Sánchez (University Hospital of Salamanca, Spain) for their technical support. In addition, the authors are grateful to all the members of GELTAMO and the patients who participated in this study.
This work was supported in part by grants from the Health Council of Castilla y León (GRS265/A/08), Red Temática de Investigación Cooperativa en Cáncer (RD12/0036/0069-RTICC, ISCIII), and the Health Research Program (PS09/01382 and CM10/00078-Río Hortega, ISCIII).
Authorship
Contribution: M.A., E.S., L.M., R.G.-S., and M.G. conceived of and designed the research; M.A. and E.S. generated the molecular results, with help from A.B., C.J., and R.C.; M.A. analyzed the data, performed the statistical analyses, and wrote the first draft of the manuscript; M.E.S., M.C.C., and L.M. provided statistical support; N.P., E.P., C.G., J.L.B., C.A., F.d.C., C.P., A.M., E.G.B., and M.D.C. provided patient samples and/or clinical data; E.S., L.M., A.M., R.G.-S., J.F.S.M., and M.G. reviewed the final manuscript; M.G. and L.M. obtained the financial support for the study; J.F.S.M. was the head of the group; and M.G. produced the final revision of the manuscript and gave final approval for the version to be published.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marcos González Díaz, Molecular Biology Histocompatibility Unit, Department of Hematology, IBSAL University Hospital of Salamanca, Paseo de San Vicente, 58-182, 37007, Salamanca, Spain; e-mail: margondi@usal.es.
References
Author notes
M.A. and E.S. contributed equally to this study.