Key Points
Epistasis between the haptoglobin (Hp) common variants and α+thalassemia predicts the risk of severe malaria in Kenyan children.
The inconsistent relationship between Hp type and malaria reported in previous studies may be explained by this epistatic interaction.
Abstract
Haptoglobin (Hp) scavenges free hemoglobin following malaria-induced hemolysis. Few studies have investigated the relationship between the common Hp variants and the risk of severe malaria, and their results are inconclusive. We conducted a case-control study of 996 children with severe Plasmodium falciparum malaria and 1220 community controls and genotyped for Hp, hemoglobin (Hb) S heterozygotes, and α+thalassemia. Hb S heterozygotes and α+thalassemia homozygotes were protected from severe malaria (odds ratio [OR], 0.12; 95% confidence interval [CI], 0.07-0.18 and OR, 0.69; 95% CI, 0.53-0.91, respectively). The risk of severe malaria also varied by Hp genotype: Hp2-1 was associated with the greatest protection against severe malaria and Hp2-2 with the greatest risk. Meta-analysis of the current and published studies suggests that Hp2-2 is associated with increased risk of severe malaria compared with Hp2-1. We found a significant interaction between Hp genotype and α+thalassemia in predicting risk of severe malaria: Hp2-1 in combination with heterozygous or homozygous α+thalassemia was associated with protection from severe malaria (OR, 0.73; 95% CI, 0.54-0.99 and OR, 0.48; 95% CI, 0.32-0.73, respectively), but α+thalassemia in combination with Hp2-2 was not protective. This epistatic interaction together with varying frequencies of α+thalassemia across Africa may explain the inconsistent relationship between Hp genotype and malaria reported in previous studies.
Introduction
Severe malaria ranks third among infectious causes of childhood death worldwide.1 Cell-free hemoglobin (Hb), released following intravascular hemolysis, is highly toxic and may contribute to the pathogenesis of severe malaria by increasing inflammation, vasoconstriction, and oxidant damage and by promoting adhesion of parasite-infected red blood cells to molecules such as intercellular adhesion molecule-1.2,3 Haptoglobin (Hp) is an acute-phase plasma protein that binds rapidly and irreversibly with cell-free Hb and the resultant Hp-Hb complexes are cleared via CD163 receptors on monocytes and tissue macrophages.4,5 Hp exists in 3 common variants in humans: the Hp1-1 dimer, the Hp2-1 linear polymer, and the large Hp2-2 circular multimer.4 Hb binding to the various Hp proteins may vary, as seen in the Hp2-2-Hb complex, which has an unstable heme moiety and is itself redox active.6 Moreover, the Hp2-2 type is associated with Hb-mediated oxidant damage,6-9 inflammation,10 endothelial cell dysfunction,11,12 and vasospasm following hemorrhage.13,14
Whether the risk of severe malaria is altered by Hp type remains unclear. Four studies that have investigated this question have produced conflicting results.15-18 Early studies, conducted in Sudan and Ghana using plasma electrophoresis to determine Hp phenotype, suggested that the Hp1-1 type was associated with an increased risk of severe malaria.15,16 However, malaria-induced hemolysis depletes plasma Hp, and in the Ghanaian study, 45% of children had an unknown or Hp0 phenotype,16 whereas the prevalence of Hp0 was not reported in the Sudanese study.15 More recent studies, conducted in The Gambia and Northern Ghana using polymerase chain reaction (PCR)-based genotyping methods, found no association between Hp genotype and severe malaria and an increased risk of severe malaria in children with the Hp2-2 genotype, respectively.17,18 Recent studies investigating the relationship between Hp genotype and the risk of uncomplicated malaria are similarly inconclusive, finding variously an increased risk of symptomatic malaria in Hp2-2 individuals,19 a reduced incidence among older children with the Hp2-2 genotype,20,21 and an increased placental parasite density among pregnant mothers with the Hp1-1 genotype.22 The effect of Hp concentration on the risk of severe malaria is also not known. Hp was toxic to malaria parasites in vitro,23 and increased parasite burden was demonstrated in an Hp knockout mouse.24 The A-61C single nucleotide polymorphism (SNP) in the Hp promoter region, which causes very low Hp concentrations,25,26 was associated with a reduced risk of uncomplicated malaria.21
Because the common HP2 allele arises from a large gene duplication27 and cannot be uniquely identified by a SNP, it has not been included in recent genome-wide association studies of severe malaria.28,29 Here we report the results of the largest case-control study conducted to date (n = 996 severe malaria cases and 1220 controls) that has investigated the association between Hp genotype and susceptibility to severe Plasmodium falciparum malaria. We further considered for the first time possible interactions between Hp and two other malaria resistance genes: Hb S heterozygotes (HbAS) and α+thalassemia.
Methods
Study population
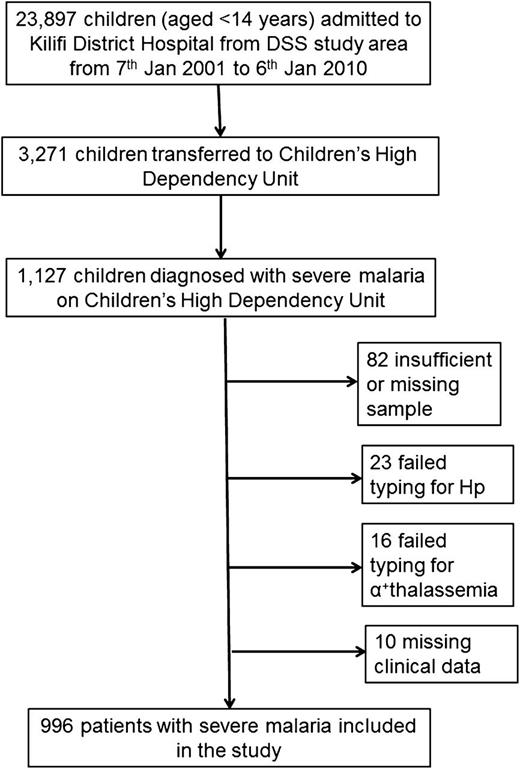
The study was conducted in the Kilifi district on the coast of Kenya, where the majority of the population are rural dwellers of the Mijikenda ethno-linguistic group. The clinical characteristics and epidemiology of malaria in the study area have been described in detail previously.30,31 Case patients were children (<14 years of age) who were residents of the study area served by the Kilifi Health and Demographic Surveillance System32 and who were admitted to the High Dependency Unit at Kilifi District Hospital between January 7, 2001 and January 6, 2010 with severe malaria. Severe malaria was defined as a positive blood film for P falciparum parasites in association with ≥1 of the following: prostration (Blantyre Coma Score 3-4), coma (Blantyre Coma Score ≤ 2), or respiratory distress (intercostal recession or deep or labored breathing).30 Children with uncomplicated severe malarial anemia (ie, Hb <5 g/dL, but with no signs of respiratory distress, prostration, or any other complications) are not routinely admitted to our High Dependency Unit and were not included in our study, because uncomplicated severe malarial anemia (SMA), when treated with transfusion, does not require intensive supportive care and is associated with a mortality of <1%.30 All case patients were treated according to standard guidelines as described in detail previously.33 The collection of case samples is summarized in Figure 1.
Study construction. Between January 7, 2001 and January 6, 2010, 23 897 children were admitted to Kilifi District Hospital from the study area served by the Kilifi Health and Demographic Surveillance System (DSS), and of these, 3271 were admitted to the Children’s High Dependency Unit. Severe life-threatening malaria was diagnosed in 1127 patients on the High Dependency Unit. Eighty-two samples were missing or had insufficient DNA for genotyping, 23 samples could not be typed for Hp, 16 samples could not be typed for α+thalassemia, and 10 samples were missing clinical data. A total of 996 severe malaria cases had complete genotyping and clinical data and were included in the study.
Study construction. Between January 7, 2001 and January 6, 2010, 23 897 children were admitted to Kilifi District Hospital from the study area served by the Kilifi Health and Demographic Surveillance System (DSS), and of these, 3271 were admitted to the Children’s High Dependency Unit. Severe life-threatening malaria was diagnosed in 1127 patients on the High Dependency Unit. Eighty-two samples were missing or had insufficient DNA for genotyping, 23 samples could not be typed for Hp, 16 samples could not be typed for α+thalassemia, and 10 samples were missing clinical data. A total of 996 severe malaria cases had complete genotyping and clinical data and were included in the study.
Controls were children born within the same study area as cases between August 14, 2006 and August 20, 2010 and were sampled as part of a cohort study of genetic susceptibility to infectious diseases during home visits at 3 to 11 months of age.34 Individual written informed consent was provided by all study participants or their parents/guardians. The study was approved by the Kenya Medical Research Institute (KEMRI)/National Ethical Review Committee in Nairobi. The study was conducted in accordance with the Declaration of Helsinki.
Laboratory methods
Routine hematologic, biochemical, and malaria parasite data were collected for all case children using standard methods as described previously.33 DNA was extracted by standard methods using proprietary kits (Qiagen DNA Blood Mini Kit; Qiagen, West Sussex, United Kingdom; or Puregene; Gentra Systems, Minneapolis, MN), and Hp genotypes were determined by allele-specific PCR as previously described.35 Hb typing for HbAA, HbAS, and HbSS was conducted by either electrophoresis using cellulose acetate gels (Helena) or by high-performance liquid chromatography (Variant analyzer; BioRad, Hercules, CA) using the β-thalassemia short program, whereas the α−3.7 deletion in the α-globin gene, the common form of α+thalassemia in Africa, was typed by PCR as described previously.36 The Hp promoter polymorphism, A-61C (rs 5471), was typed at the Wellcome Trust Centre for Human Genetics, Oxford, United Kingdom, by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry using the SEQUENOM system (San Diego, CA).37
Statistical analyses
All analyses were conducted using Stata V12.0 (StataCorp, College Station, TX). Non-normally distributed variables were log-transformed prior to analysis. Categorical data were analyzed using the χ2 test, whereas the distribution of continuous variables by Hp genotype was investigated using linear regression. The association between Hp genotype and severe malaria was determined by analysis of variance. Logistic regression was used to derive odds ratios (ORs) for risk of severe malaria overall, severe malaria subgroups, and in-patient death according to Hp genotype in univariable and multivariable models adjusted for potential confounders including gender, ethnicity, Hb type (HbAS), and α+thalassemia genotype. Interactions between Hp genotype and other explanatory variables were assessed using the likelihood-ratio test.
Meta-analysis of studies of Hp type and severe malaria
The following criteria were applied to potential studies for inclusion in the meta-analysis: (1) indexed in PubMed (National Center for Biotechnology Information) under the search terms “severe malaria” and “Hp phenotype” or “Hp genotype”; (2) original studies in which both case patients and controls were children; and (3) a case-control study design with clear comparative groups of cases with severe malaria and controls without severe malaria. Four studies were identified,15-18 of which 2 were excluded: one because the study also included adult cases and a control group that consisted only of adults recruited among the staff, technicians, workers, and students at the institute15 and a second because 45% of cases and controls were of unknown (Hp0) phenotype.16 Data from the 2 remaining studies17,18 were extracted and summarized, and meta-analysis was performed using STATA V.12.0.
Results
Characteristics of severe malaria patients
Our study included 996 case patients with severe malaria and 1220 controls. The median age of patients was 27.2 months (range, 0-147 months), 49.8% were boys, and 97.2% were of the Mijikenda ethnic group. The characteristics of case patients, stratified by Hp genotype, are summarized in Table 1. Overall, the geometric mean P falciparum parasite density and Hb concentrations were 57 435/μL (95% CI, 49 405-66 770) and 6.6 g/dL (95% CI, 6.5-6.8), respectively, whereas the proportions of severe malaria patients with HbAS, −α/αα thalassemia, −α/−α thalassemia, and Hp-61C were 2.2%, 48.3%, 11.8%, and 20.2%, respectively. The demographic characteristics of severe malaria patients did not vary according to Hp genotype (Table 1). Cerebral malaria was diagnosed in 528 children (53.1%), severe anemia in 224 children (22.6%), and 104 children (10.5%) had both cerebral malaria and severe anemia. Other nonexclusive categorizations of severe malaria, stratified by Hp genotype, are summarized in Table 2. Ninety-four severe malaria patients (9.4%) died.
Hp genotype and risk of severe malaria
Hp genotype was associated with risk of severe malaria by analysis of variance (P = .01 before and after adjustment for gender, ethnicity, Hb type [HbAS], and α+thalassemia genotype). We therefore used logistic regression models to determine which of the 3 2-way comparisons between Hp genotypes accounted for this statistically significant variation in risk (Table 3).
Hp2-2 was associated with the greatest risk and Hp2-1 with the least risk of severe malaria. The risk of severe malaria did not differ significantly between Hp1-1 and Hp2-2 genotypes (P = .32) and varied with marginal significance between Hp1-1 and Hp2-1 genotypes (P = .06; Table 3). However, the risk of severe malaria was significantly increased in the Hp2-2 genotype compared with the Hp2-1 genotype (OR, 1.35; 95% CI, 1.10-1.67; P = .005) or compared with Hp2-1 and Hp1-1 genotypes combined (OR, 1.26; 95% CI, 1.03-1.53; P = .02). Conversely, the Hp2-1 genotype was associated with 26% protection against severe malaria compared with Hp2-2 (OR, 0.74; 95% CI, 0.60-0.91; P = .005) or 21% protection compared with the Hp2-2 and Hp1-1 genotypes combined (OR, 0.79; 95% CI, 0.67-0.93; P = .006), indicating a heterozygote advantage.
ORs were significantly raised in the Hp2-2 genotype compared with the Hp2-1 genotype for all categories of severe malaria except for symptomatic SMA, in which there was a nonsignificantly increased risk (P = .10; Table 3). Hp2-2 was also associated with a marginally significant increased OR for death compared with Hp1-1. Compared with children of the Hp2-1 genotype, those of the Hp1-1 genotype were at significantly increased risk of deep breathing and metabolic acidosis (Table 3). Parasite densities did not differ significantly between the Hp genotypes.
Hp A-61C promoter polymorphism
To investigate the effect of Hp concentration on the risk of severe malaria, we typed the Hp A-61C promoter SNP, which is known to be associated with very low Hp concentrations,25 in a subset of 519 case patients and 876 controls for whom DNA samples were available in the United Kingdom. The characteristics of the subset typed did not differ from the nontyped group in any respect except with regard to subgroups within the Mijikenda ethnic group (the typed subset included more of the Kambe group and the nontyped group more of the Kauma group; P < .05). The −61C SNP, present in 104 severe malaria cases (20.2%) and in 167 controls (19.1%), was significantly associated with the HP2 allele as previously reported,21 and no −61CC homozygotes were identified. We found no association between the −61C allele and the risk of severe malaria (OR, 1.05; 95% CI, 0.80-1.38; P = .75 unadjusted and OR, 0.91; 95% CI, 0.54-1.52; P = .71 adjusted) or any evidence for an interaction between the −61C SNP and the common Hp variants in predicting risk of severe malaria (P = .66 in likelihood-ratio testing).
HbS
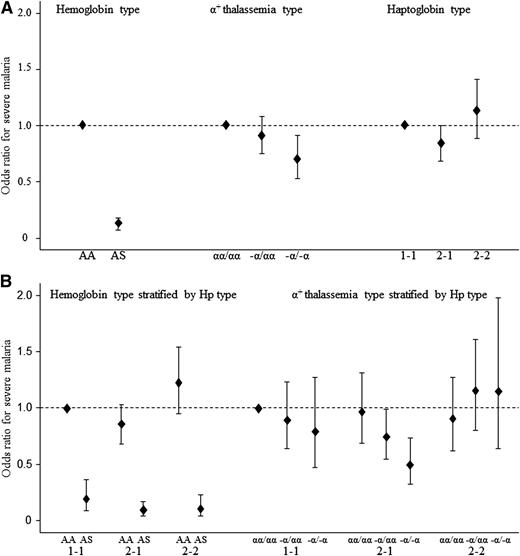
Hb typing was successful in 990 cases (99%) and 1220 controls (100%). HbAS, carried by 22 cases (2.2%) and 200 controls (16.4%), was associated with 88% protection against severe malaria (OR, 0.12; 95% CI, 0.07-0.18; P < .0005). We found no evidence for an interaction between Hp genotype and hemoglobin type (HbAA, HbAS) in predicting the risk of severe malaria (P = .28 in likelihood-ratio testing); however, given the small number of children with HbAS among our severe malaria cases (n = 22/990), our study was underpowered to find such an effect.
α+thalassemia
The heterozygous α+thalassemia (−α/αα) was carried by 481 cases (48.3%) and 591 controls (48.4%), whereas homozygous α+thalassemia (−α/−α) was carried by 117 cases (11.8%) and 187 controls (15.3%). The −α/−α genotype was associated with 31% protection against severe malaria (OR, 0.69; 95% CI, 0.53-0.91; P = .008), whereas the −α/αα thalassemia type was not significantly associated with protection (P = .27). However, we found statistically significant evidence for an interaction between α+thalassemia and Hp type in predicting the risk of severe malaria (P = .02 in likelihood-ratio testing). The risk of severe malaria was lowest for −α/−α thalassemia inherited in combination with Hp2-1, but α+thalassemia was not protective when inherited in combination with Hp2-2. Hp1-1 was associated with a nonsignificant trend toward protection against severe malaria when inherited with α+thalassemia (Figure 2). ORs for the risk of severe malaria stratified by α+thalassemia are shown in Table 4, illustrating the effect of α+thalassemia in modifying risk associated with Hp genotype.
ORs for severe malaria by HbAS, α+thalassemia, and Hp genotypes. Logistic regression models were used to determine ORs for risk of severe malaria by (A) Hb type (HbAS), α+thalassemia type, and Hp genotype. HbAA, αα/αα and Hp1-1 were the respective reference types with an OR for severe malaria of 1.0. (B) Hb type (HbAS) and α+thalassemia type stratified by Hp genotype. HbAA and Hp1-1 and αα/αα and Hp1-1 were the respective reference types with an OR for severe malaria of 1.0.
ORs for severe malaria by HbAS, α+thalassemia, and Hp genotypes. Logistic regression models were used to determine ORs for risk of severe malaria by (A) Hb type (HbAS), α+thalassemia type, and Hp genotype. HbAA, αα/αα and Hp1-1 were the respective reference types with an OR for severe malaria of 1.0. (B) Hb type (HbAS) and α+thalassemia type stratified by Hp genotype. HbAA and Hp1-1 and αα/αα and Hp1-1 were the respective reference types with an OR for severe malaria of 1.0.
Meta-analysis
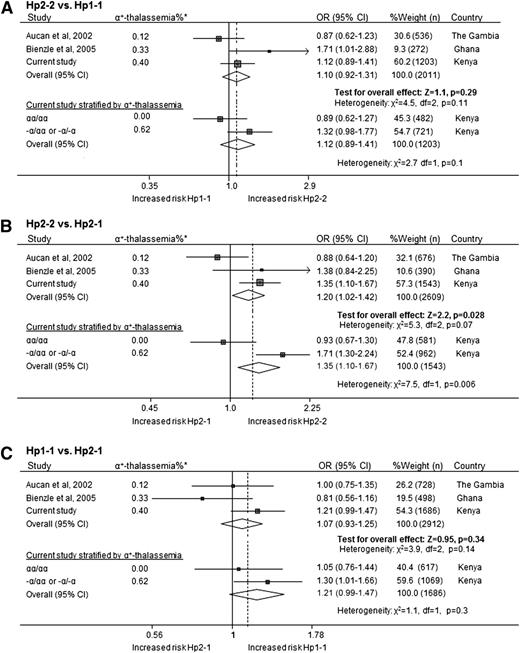
In addition to our current study, we identified 2 eligible additional studies relating to Hp type and the risk of severe malaria17,18 for inclusion in a meta-analysis. Our analysis suggested that the Hp2-2 genotype is associated with an increased risk of severe malaria compared with the Hp2-1 genotype (OR, 1.20; 95% CI, 1.02-1.42; P = .028; Figure 3) but that there is no significant variation in risk of severe malaria between Hp2-2 and Hp1-1 or between Hp1-1 and Hp2-1. We further stratified the current study by α+thalassemia and showed significant heterogeneity between these groups in predicting risk of severe malaria for Hp2-2 vs Hp2-1 (P = .006); the OR for severe malaria was 0.93 (95% CI, 0.67-1.30) in the group without α+thalassemia and 1.71 (95% CI, 1.30-2.24) in the group with α+thalassemia (Figure 3).
Meta-analysis of studies examining the relationship between Hp type and severe malaria. Forest plots showing a meta-analysis of eligible case-control studies that have examined the relationship between Hp type and the risk of severe malaria for (A) Hp2-2 vs Hp1-1; (B) Hp2-2 vs Hp2-1; and (C) Hp1-1 vs Hp2-1. Individual estimates and the relative contribution of the individual studies to the overall estimates (percentage weight and numbers in each group) are shown. *The frequency of the –α/ allele in the relevant country. The studies by Aucan et al17 and Bienzle et al18 do not report the prevalence of α+thalassemia in their study populations, and the prevalences shown (0.12 in The Gambia39 and 0.33 in Ghana40 ) are from other studies within the same country. Further Forest plots show the results of the current study stratified by α+thalassemia status.
Meta-analysis of studies examining the relationship between Hp type and severe malaria. Forest plots showing a meta-analysis of eligible case-control studies that have examined the relationship between Hp type and the risk of severe malaria for (A) Hp2-2 vs Hp1-1; (B) Hp2-2 vs Hp2-1; and (C) Hp1-1 vs Hp2-1. Individual estimates and the relative contribution of the individual studies to the overall estimates (percentage weight and numbers in each group) are shown. *The frequency of the –α/ allele in the relevant country. The studies by Aucan et al17 and Bienzle et al18 do not report the prevalence of α+thalassemia in their study populations, and the prevalences shown (0.12 in The Gambia39 and 0.33 in Ghana40 ) are from other studies within the same country. Further Forest plots show the results of the current study stratified by α+thalassemia status.
Discussion
In a large case-control study of 996 severe malaria case children and 1220 controls, we found that in Kilifi, Kenya, the risk of severe malaria is clearly associated with the common Hp variants. The highest risk for severe malaria was found in the Hp2-2 genotype and the lowest risk in the Hp2-1 genotype. This finding was supported by a meta-analysis of this and 2 earlier studies that suggested an increased risk of severe malaria in Hp2-2 compared with Hp2-1 individuals. Hp1-1 individuals may have had an increased risk of severe malaria compared with Hp2-1 individuals, but this was not supported on meta-analysis. In subgroup analyses, we found that the increased risk of severe malaria among Hp2-2 subjects was seen in all the severe malaria syndromes, although this did not reach statistical significance in the symptomatic SMA group. Finally, we found evidence to suggest that the effect of Hp on the risk of severe malaria is modified by α+thalassemia.
Our finding of an increased risk of severe malaria among Hp2-2 individuals is in apparent contradiction to 2 earlier studies conducted in Sudan and Ghana,15,16 both of which reported a reduced risk of severe malaria among children of the Hp2-2 phenotype. This might be explained by the fact that in these previous studies Hp type was based on phenotyping rather than genotyping, because Hp2-2 is present at lower plasma concentrations and is more likely to be depleted during malaria-related hemolysis and therefore lead to biased misclassification. Similarly, our findings are not in complete agreement with 2 studies conducted by genotyping. In 1 study, conducted in Northern Ghana, the authors found evidence for a marginally increased risk of severe malaria in Hp2-2 individuals,18 whereas in a second study, conducted in The Gambia, the authors found no association between Hp genotype and severe malaria risk.17 It is possible that the clinical characteristics of case patients included in these studies may have differed from those included in our current study. In our study, we did not include children presenting with uncomplicated severe malaria anemia because this condition is not associated with significant mortality.30 Differences in ethnicity and genetic diversity may be another explanation. Finally, the varying observations made in different populations might also be explained by epistasis, which holds that the effect of a genotype at a particular locus depends on the genotype coinherited at a second unrelated locus. Epistasis is likely to be more common than previously thought.38
We looked for possible epistasis between Hp genotype and 2 known malaria-resistance genes: HbAS, which results from a structural abnormality of the β-globin chains of Hb, and α+thalassemia, which results from the underproduction of normal α-globin chains of Hb. The number of children with HbAS and severe malaria were few (n = 22), and our study was underpowered to investigate any potential epistasis between HbAS and Hp genotype. However, we did find evidence for an epistatic interaction between α+thalassemia and Hp genotype (P = .02). Our data suggest that α+thalassemia inherited in combination with Hp2-1 is strongly protective against severe malaria (37% protection, P = .003) but that protection is considerably reduced when inherited in combination with Hp1-1 (13% protection, P = .39) and is lost altogether when inherited in combination with Hp2-2 (Table 4). Similarly, although the Hp genotype inherited in combination with α+thalassemia significantly altered the risk of severe malaria, the Hp genotype in the absence of α+thalassemia did not appear to alter risk in subgroup analyses (Table 4). Although this possible epistasis should be viewed with caution, it seems plausible that varying frequencies of α+thalassemia across Africa might explain apparent differences in the results of previous studies investigating the association between Hp type and severe malaria. For example, the frequency of the α−3.7 allele, the most common cause of α+thalassemia in sub-Saharan Africa, is 0.12 in The Gambia,39 0.33 in Ghana,40 and 0.40 in our population. Varying HP2 allele frequencies could similarly explain differing findings for α+thalassemia association studies.
If epistasis exists between the common Hp variants and α+thalassemia, by what mechanism might it act? Despite high population frequencies of α+thalassemia and the HP2 allele in many malaria-endemic areas, little is known about the pathophysiological consequences of their coinheritance. A number of mechanisms for an epistatic interaction seem plausible, a few of which are summarized here. Individuals with α+thalassemia are under increased oxidative stress,41 a fact that likely relates to an intraerythrocytic excess of unmatched β chains and reactive free thiols.42 Hp2-2, unlike Hp1-1 and Hp2-1, is significantly less able to quench Hb-iron mediated oxidant stress,6-8 which may account for reduced ferroxidase and vitamin C levels in Hp2-2 individuals.43-45 Additionally, methemoglobin, an endothelial cell activator, is increased in thalassemia42,46 and may be further increased in Hp2-2 individuals following hemolysis due to an oxidatively unstable heme moiety in the Hp2-2–Hb complex.6 The Hp2-2 variant is further associated with a shift toward a proinflammatory Th1 cytokine response.10 Thus, it is possible that the protection conferred by α+thalassemia is lost when coinherited with Hp2-2 due to excessive oxidant damage, inflammation, and endothelial cell activation, especially within the brain and deep tissues where the large Hp2-2 protein is less able to penetrate.47 Indeed, subarachnoid hemorrhage in patients with the Hp2-2 genotype results in more severe vasospasm, tissue ischemia, and inflammation.13,14,48 Additionally, the reduced rosetting49-51 and endothelial cell adherence51 observed in α+thalassemia may be countered by the up-regulation of vascular cell adhesion molecules and endothelial cell dysfunction observed in Hp2-2 individuals,11,12 resulting in loss of protection in individuals coinheriting both genotypes.
Conversely, Hp2-1 coinherited with α+thalassemia appeared to confer significant protection from severe malaria indicating heterozygote advantage. In addition to reduced rosetting, infected α+thalassemia cell membranes bind significantly more malaria immune globin and are more susceptible to phagocytosis compared with control cells,52,53 a process likely mediated by oxidative damage to the red cell membrane from unbound β chains and accelerated acquisition of aggregated band 3 proteins.53,54 It is possible that the Hp2-1 variant optimizes the protective effect of α+thalassemia by providing a balanced plasma environment with optimal oxidant/antioxidant levels and Th1 vs Th2 cytokines compared with Hp1-1 and Hp2-2. Hp2-1 has a distinct molecular structure compared with the other variants; for example, Vibrio vulnificus is unable to acquire iron from Hp2-1–Hb complexes, despite iron acquisition from Hp1-1–Hb and Hp2-2–Hb complexes.55 Heterozygote advantage from Hp2-1 is further observed with protection from Kaposi’s sarcoma56 and reduced mortality in HIV patients.57 A similar trend toward protection was seen in individuals coinheriting Hp1-1 and α+thalassemia, although this did not reach statistical significance. Epistasis may provide valuable insights into the mechanisms by which malaria resistance genes provide protection.
We did not find an interaction between the common Hp variants and the −61C allele or any influence of the −61C allele on the risk of severe malaria. It might be expected that low Hp concentrations associated with the −61C allele25,26 would expose children to the deleterious effects of cell-free Hb and therefore predispose such children to severe malaria.2 However, in our previous study of children with uncomplicated malaria, although the −61C allele was associated with reduced Hp concentrations during convalescence when malaria parasites had been cleared, it had no influence on Hp concentration at the time of a malaria episode.21 Hp is up-regulated during the acute phase response, and this may counter the reduced transcription that might result from the −61C allele outside the acute phase response. Alternatively, it is also possible that the structure or function of the common Hp variants may be more clinically relevant than their concentrations. Our finding differs from that made in our earlier study conducted in The Gambia, in which a reduced incidence of uncomplicated malaria was found only in children >3 years of age carrying the −61C allele.21 Because this protection was only seen in older children, we proposed that an immune mediated mechanism, possibly mediated by low Hp concentration, oxidative damage to the red cell membrane, and accelerated acquisition of aggregated band 3 proteins or by other immune modulation, might have been involved.21 In the current study, the majority of children were <3 years of age and as such will have had less time to acquire immunity. The patient mix was also different between the studies. Children in the current study had severe life-threatening malaria requiring high dependency care in hospital, whereas the previous study involved children in the community with a mild febrile episode associated with malaria parasites on blood film. Moreover, although Hp concentration at convalescence might influence acquisition of immunity following uncomplicated malaria, Hp concentration at the time of malaria may be more critically important in severe malaria. It also seems possible that the apparently conflicting findings between these 2 studies could be explained by a range of other genetic, ethnic, or environmental differences between the children involved. We also previously reported a lower incidence of uncomplicated clinical malaria in older children (>3 years) carrying the Hp2-2 genotype, postulating that this might be mediated by oxidative damage to the red cell membrane and accelerated acquisition of antibodies to aggregated band 3 proteins.20 Similarly, in the current study, the majority of children were <3 years old and thus would have had less time to acquire immunity.
In summary, this large case control study and meta-analysis suggest that the common Hp 2-2 genotype confers an increased risk of severe malaria and that the Hp2-1 genotype is protective. Moreover, our data are compatible with an epistatic interaction with regard to susceptibility to severe malaria between Hp and α+thalassemia. It seems plausible that heterozygote advantage, balancing selection pressure, and epistasis might explain the varying gene frequencies of the HP2 allele and α+thalassemia in different populations and explain why the relationship between malaria and HP2 has proved difficult to confirm. Further studies investigating these associations in other malaria-endemic populations are indicated.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the study participants, their families, and the nurses and fieldworkers who participated in this study and Kevin Marsh, Kathryn Maitland, and Charles Newton for their contribution to the study. The authors also thank David Weatherall and Andrew Prentice for helpful discussions relating to α+thalassemia and Hp. The authors thank the staff of the human genetics laboratory at the KEMRI-Wellcome Trust Programme including Herbert Opi, Metrine Tendwa, Johnstone Makale, Adan Mohamed, Kenneth Magua, and Ruth Mwarabu for their help with sample processing, genotyping and database support.
T.N.W. is funded by a fellowship from the Wellcome Trust (091758) and by funds from the European Union FP7 EVIMalR Consortium. S.H.A. was supported by a Career Support Award from Oxford University Clinical Academic Graduate School and by awards from the European Society of Pediatric Infectious Disease, The Academy of Medical Sciences, The Wellcome Trust, The British Heart Foundation, and Arthritis Research United Kingdom.
This paper is published with permission from the Director of KEMRI.
Authorship
Contribution: S.H.A. conceived the study, performed experiments, analyzed data, and wrote the manuscript; S.M.U. performed experiments, analyzed data, and contributed to writing the manuscript; E.N. and A.W.M. performed experiments and contributed to data analysis; G.N. and C.N. managed databases and analyzed data; D.P.K. conceived the study and performed experiments; K.A.R. performed experiments, contributed to data analysis, and wrote the manuscript; and T.N.W. conceived the study, obtained funding, contributed to data analysis, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sarah H. Atkinson, KEMRI/Wellcome Trust Research Programme, Centre for Geographic Medicine Research-Coast, PO Box 230, Kilifi, Kenya; e-mail: satkinson@kemri-wellcome.org.
References
Author notes
S.H.A. and S.M.U. contributed equally to this study.