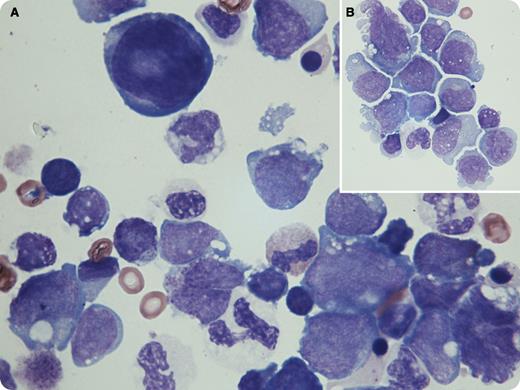
A 64-year-old female presented with poorly differentiated acute myeloid leukemia (AML) following a history of essential thrombocythemia. Bone marrow showed hypercellularity and 21% blasts, which were CD13+, CD33+, CD34+, CD45dim, MPO+, CD117+, and HLADR+. Cytogenetic testing revealed a complex karyotype; del(5q) and del(7q) were identified by fluorescence in situ hybridization. Blasts were seen on peripheral smear review. After failed induction with arabinosylcytosine and daunorubicin, treatment was replaced with decitabine and ruxolitinib. Complications included (presumed) fungal pneumonia, pleural and pericardial effusions, Staphylococcus bacteremia, pathological fracture of right coracoid process, and widespread osteolytic lesions. The patient reported fevers, night sweats, mild cough, and exertional dyspnea. Thoracentesis was performed, and the following cell counts were obtained: white blood cells, 1450/μL; red blood cells, 330/μL; and differential, 64% blasts with immunophenotype consistent with the initial diagnosis. As shown in panels A and B, blasts were pleomorphic with medium to giant/irregular forms, variable N:C ratio, basophilic cytoplasm, conspicuous nucleoli, smooth chromatin (moderate clumping in some), and occasional multinucleated form. Few blasts had sparse azurophilic granules, and a large atypical hyperchromatic mesothelial cell was also noted on the slide (panel A, top center).
Cytospin-induced changes in blast morphology include irregular nuclear contours, more pronounced nucleoli, increased cytoplasm, and abnormal concentration of cytoplasmic granules. Cytospin smears should be evaluated with caution in light of these in vitro preparation–induced changes.
A 64-year-old female presented with poorly differentiated acute myeloid leukemia (AML) following a history of essential thrombocythemia. Bone marrow showed hypercellularity and 21% blasts, which were CD13+, CD33+, CD34+, CD45dim, MPO+, CD117+, and HLADR+. Cytogenetic testing revealed a complex karyotype; del(5q) and del(7q) were identified by fluorescence in situ hybridization. Blasts were seen on peripheral smear review. After failed induction with arabinosylcytosine and daunorubicin, treatment was replaced with decitabine and ruxolitinib. Complications included (presumed) fungal pneumonia, pleural and pericardial effusions, Staphylococcus bacteremia, pathological fracture of right coracoid process, and widespread osteolytic lesions. The patient reported fevers, night sweats, mild cough, and exertional dyspnea. Thoracentesis was performed, and the following cell counts were obtained: white blood cells, 1450/μL; red blood cells, 330/μL; and differential, 64% blasts with immunophenotype consistent with the initial diagnosis. As shown in panels A and B, blasts were pleomorphic with medium to giant/irregular forms, variable N:C ratio, basophilic cytoplasm, conspicuous nucleoli, smooth chromatin (moderate clumping in some), and occasional multinucleated form. Few blasts had sparse azurophilic granules, and a large atypical hyperchromatic mesothelial cell was also noted on the slide (panel A, top center).
Cytospin-induced changes in blast morphology include irregular nuclear contours, more pronounced nucleoli, increased cytoplasm, and abnormal concentration of cytoplasmic granules. Cytospin smears should be evaluated with caution in light of these in vitro preparation–induced changes.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.