Abstract
Background: Bone marrow transplant (BMT) remains the preferred frontline curative modality for patients with aplastic anemia in the presence of a matched sibling donor (MSD). In the absence of MSD the general consensus is frontline immunosuppressive therapy (IST) followed by BMT from a matched unrelated donor (MUD) in case of failure or relapse. No randomized controlled studies have been performed to compare earlier MUD transplant to 2nd cycle IST in case of failure of response to 1st IST cycle. In the pediatric population a higher percentage of congenital marrow failure syndromes is encountered than in adult world; the diagnosis of many of those is challenging clinically and from the molecular and genetic standpoints.
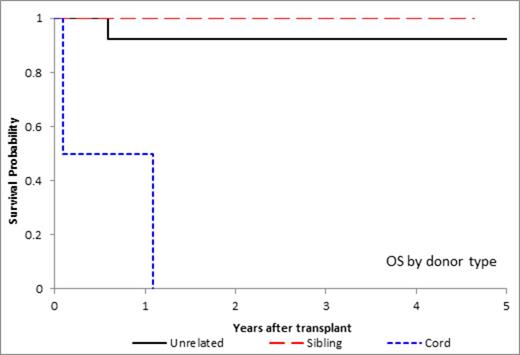
Objectives: Review the outcome of 25 patients younger than 20 years diagnosed with aplastic anemia and recently transplanted at our institution. Compare outcomes of MSD versus MUD versus umbilical cord (UC) BMT in this patient population.
Methods: A retrospective analysis was performed on 25 patients diagnosed with aplastic anemia who underwent BMT at St Jude Children’s Research Hospital between 9/1/2009 through 8/31/2013. Initial diagnosis and treatment, patients’ characteristics, transplant data, overall survival, and complications were analyzed.
Results: Of the 25 patients reviewed, 15 patients were diagnosed with acquired aplastic anemia and 10 with congenital marrow failure, including 7 with dyskeratosis congenita (DKC), 1 with Shwachman Diamond syndrome (SDS), and 2 with congenital marrow failure not otherwise specified (negative genetic testing, but age, family history, and presentation consistent with congenital marrow failure). All 7 DKC patients had telomere lengths less than first percentile, and 2 had documented genetic mutations; of the 7 patients 2 received MSD, 3 received MUD and 2 received UC transplants.
Most donors were MUD (13/25), 2 were UC donors as there were no other available donors, and 10 were MSD. All MSD recipients are alive, engrafted and disease free. There were 3 deaths. One MUD recipient with acquired aplastic anemia died of uncontrolled sepsis. Both UC recipients died; one had failure of engraftment and later died of acute myeloid leukemia that had developed on day +224 of transplant while on Danazol and G-CSF, and the other died of pulmonary and hepatic failure. The latter was the only patient who received TBI (2 Gy) as part of his conditioning regimen, engrafted on day +27 and died on day +33. There was no statistical difference in overall survival (OS) between MSD and MUD transplant (100% vs 92.3% at 3 years, respectively, p value = 0.38).
Acute graft versus host disease (aGVHD) developed in 5 patients; 3 had received MUD transplant and 2 had received MSD. Two of these 5 patients also developed chronic graft versus host disease (cGVHD), which was limited in both cases. There was no statistically significant difference in engraftment or GVHD occurrence between the MSD and MUD patients.
Conclusions: In our recent experience aplastic anemia in children,outcomes from MUD BMT were comparable to MSD BMT, especially with improved supportive care and GVHD prevention and treatment. Cord blood as an alternative donor source remains very challenging in this patient population from the engraftment and toxicity standpoints especially in certain congenital marrow failure syndromes. These data suggest that BMT should be considered earlier when there is MUD availability for patients with aplastic anemia.
P unrelated vs cord = 0.0007
P sibling vs cord = 0.0002
P unrelated vs sibling = 0.38
Reiss:Alexion Pharm: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.