Abstract
Background: Acquired chromosome abnormalities, mutations in specific genes, age, comorbidities and prior cancer therapy are some of the factors affecting survival of younger patients with acute myeloid leukemia (AML). Less is known about non-biological factors (NBFs) that may affect the outcome of AML patients.
Methods: We conducted an analysis of AML cases reported to the Surveillance Epidemiology and End Results (SEER-18) program between 2007 (year when insurance information became available) and 2011 (most recent year available). In addition to biological characteristics, we inquired the impact of NBFs: health insurance, marital status, income, level of education and distance from county of residence to the nearest blood and marrow transplant center (a surrogate for access to advanced care) on survival of adult (>18) patients younger than 65 at the time of diagnosis of AML.
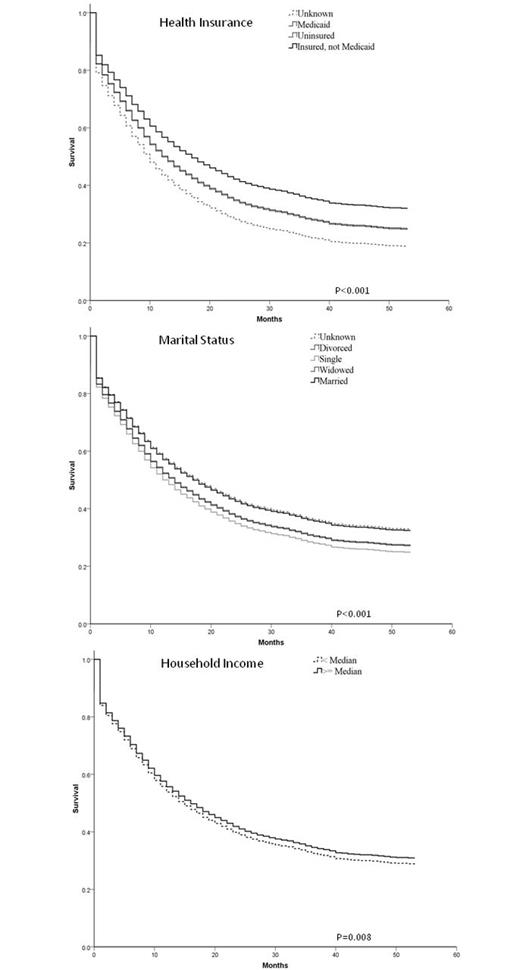
Results: The analysis included 5,904 patients with a median follow up of survivors of 19 months. Median age at diagnosis was 53 (IQR 42-59), 47% were female, 64.3% non-Hispanic Whites (NHW), 10.5% non-Hispanic Blacks (NHB), 14.6% Hispanics, 9.5% Asian or Pacific Islanders (API) and 0.6% American Indian or Alaska Native (AIAN). In terms of AML subtype (as coded by ICD-O-3, comprising a mix of morphology and cytogenetically-defined entities), 51.7% were registered as having simply AML-NOS, 5.0% had t(8;21), t(16;16) or inv (16), 1.3 % had t(6;9) or t(9;11) or inv(3), 11.2% had AML-NOS M0, M1 or M2, 18.5% AML-NOS M4 or M5, 1.9% AML-NOS M6 and 0.6% AML-NOS M7 or t(1;22). Married patients were 57.7%, 24.4% were single, 10.8% divorced, 2.7% widowed. There were 18.1% of patients enrolled in Medicaid, 72.9% with other type of insurance and 6.0% uninsured. Multivariate Cox proportional hazard model confirmed AML subtype to be predictive of survival along with age and sex. NBFs independently associated with survival were insurance status, marital status and income (Figure 1 - adjusted survival curves). Patients with Insurance other than Medicaid had the best outcome while uninsured patients and patients covered by Medicaid had similarly poor survival. Married patients (and patients with unknown marital status) had better survival than patients divorced, widowed or single. Education and distance to transplant center did not predict survival (Table 1).
Conclusion: NBFs play a substantial role in determining outcomes of younger adult patients with AML and need to be considered in efforts to improve outcomes in this disease.
– Multivariate analysis of biological and non-biological factors associated with survival in AML
| Factor . | Reference . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| AML category | <0.001 | |||
| t(8;21) or t(16;16) or inv(16) | AML-NOS | 0.47 | 038-0.58 | <0.001 |
| t(6;9) or t(9;11) or inv(3) | AML-NOS | 1.12 | 0.83-1.52 | 0.47 |
| NOS- M0,M1 or M2 | AML-NOS | 0.81 | 0.72-0.91 | <0.001 |
| NOS – M4 or M5 | AML-NOS | 0.96 | 0.87-1.05 | 0.34 |
| NOS-M6 | AML-NOS | 1.02 | 0.80-1.31 | 0.85 |
| NOS-M7, t(1;22) | AML-NOS | 2.04 | 1.41-2.95 | <0.001 |
| AML with myelodysplasia-related changes | AML-NOS | 1.07 | 0.93-1.23 | 0.31 |
| Therapy-related AML | AML-NOS | 1.09 | 0.90-1.33 | 0.38 |
| Age | Per 1 year | 1.02 | 1.02-1.03 | <0.001 |
| Female | Male | 0.89 | 0.83-0.95 | 0.001 |
| Marital status | <0.001 | |||
| Single | Married | 1.23 | 1.12-1.35 | <0.001 |
| Divorced | Married | 1.15 | 1.03-1.29 | 0.01 |
| Widowed | Married | 1.16 | 0.94-1.42 | 0.18 |
| Unknown | Married | 0.99 | 0.82-1.19 | 0.89 |
| Insurance status | <0.001 | |||
| Medicaid | Insured | 1.21 | 1.11-1.34 | <0.001 |
| Uninsured | Insured | 1.23 | 1.06-1.43 | 0.006 |
| Unknown | Insured | 1.46 | 1.19-1.80 | <0.001 |
| Household income > median | 0.91 | 0.85-0.98 | 0.008 | |
| Race-ethnicity | 0.009 | |||
| AIAN | NHW | 0.80 | 0.48-1.34 | 0.40 |
| API | NHW | 1.01 | 0.89-1.14 | 0.86 |
| Hispanic | NHW | 1.08 | 0.97-1.20 | 0.15 |
| NHB | NHW | 1.22 | 1.10-1.37 | <0.001 |
| Unknown | NHW | 0.73 | 0.39-1.37 | 0.33 |
| Factor . | Reference . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| AML category | <0.001 | |||
| t(8;21) or t(16;16) or inv(16) | AML-NOS | 0.47 | 038-0.58 | <0.001 |
| t(6;9) or t(9;11) or inv(3) | AML-NOS | 1.12 | 0.83-1.52 | 0.47 |
| NOS- M0,M1 or M2 | AML-NOS | 0.81 | 0.72-0.91 | <0.001 |
| NOS – M4 or M5 | AML-NOS | 0.96 | 0.87-1.05 | 0.34 |
| NOS-M6 | AML-NOS | 1.02 | 0.80-1.31 | 0.85 |
| NOS-M7, t(1;22) | AML-NOS | 2.04 | 1.41-2.95 | <0.001 |
| AML with myelodysplasia-related changes | AML-NOS | 1.07 | 0.93-1.23 | 0.31 |
| Therapy-related AML | AML-NOS | 1.09 | 0.90-1.33 | 0.38 |
| Age | Per 1 year | 1.02 | 1.02-1.03 | <0.001 |
| Female | Male | 0.89 | 0.83-0.95 | 0.001 |
| Marital status | <0.001 | |||
| Single | Married | 1.23 | 1.12-1.35 | <0.001 |
| Divorced | Married | 1.15 | 1.03-1.29 | 0.01 |
| Widowed | Married | 1.16 | 0.94-1.42 | 0.18 |
| Unknown | Married | 0.99 | 0.82-1.19 | 0.89 |
| Insurance status | <0.001 | |||
| Medicaid | Insured | 1.21 | 1.11-1.34 | <0.001 |
| Uninsured | Insured | 1.23 | 1.06-1.43 | 0.006 |
| Unknown | Insured | 1.46 | 1.19-1.80 | <0.001 |
| Household income > median | 0.91 | 0.85-0.98 | 0.008 | |
| Race-ethnicity | 0.009 | |||
| AIAN | NHW | 0.80 | 0.48-1.34 | 0.40 |
| API | NHW | 1.01 | 0.89-1.14 | 0.86 |
| Hispanic | NHW | 1.08 | 0.97-1.20 | 0.15 |
| NHB | NHW | 1.22 | 1.10-1.37 | <0.001 |
| Unknown | NHW | 0.73 | 0.39-1.37 | 0.33 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.