Abstract
Transforming growth factor β (TGF-β) is a key regulator of cell growth and survival. We have previously reported the pro-survival role of TGF-β1 and the anti-leukemic efficacy of TGF-β neutralizing antibody in the bone marrow (BM) microenvironment (Xu et al., Br J Haematol.2008, Tabe et al. PLoS One. 2013). FLI-1 is a transcription factor that plays a pivotal role in the regulation of extracellular matrix genes under negative regulation by TGF-β1–dependent acetylation. We reported that patients with acute myeloid leukemia (AML) expressing a low level of FLI-1 achieved high rates of remission, but their remission duration and survival were curtailed (Kornblau et al., Blood, 2011). Moreover, treatment with rhTGF-β1 induced expression of matrix metalloproteinase-1 (MMP-1) mRNA in AML cells, which inversely correlated with FLI-1 expression (Tabe et al. ASH 2012), concordant with a previous report that FLI-1 downregulates the expression of MMP-1 promoter activity.
In this study, we investigated the molecular mechanisms by which TGF-β induces AML cell survival. In AML cell lines NB4, U937, and OCI-AML3, rhTGF-β1 (2ng/mL) induced the TGF-β downstream targets plasminogen activator inhibitor-1 (PAI-1, mRNA) and Smad2 phosphorylation (p-Smad2). These effects were reversed by anti–TGF-β neutralizing antibody 1D11 but not by the isotype control antibody 13C4. Treatment with rhTGF-β1 significantly inhibited serum starvation–induced apoptosis and promoted G0/G1 cell cycle arrest in NB4 and U937 cells but not in OCI-AML3 cells (subG1% vs controls at 72 h: NB4, 18.9 ± 1.7 vs 12.8 ± 1.3; U937, 51.9 ± 2.8 vs 29.1 ± 2.4; OCI-AML3, 8.8 ± 0.5 vs 7.7 ± 0.5; G0/G1 % vs controls at 72 h:,NB4, 39.2 ± 3.5 vs 55.6 ± 5.6; U937, 16.0 ± 1.8 vs 37.6 ± 2.1; OCI-AML3, 68.0 ± 4.2 vs 55.1 ± 9.9). These changes were effectively reversed by 1D11, indicating that rhTGF-β1 facilitated pro-survival effects along with transition into a quiescent G0 state in NB4 and U937 cells but not in OCI-AML3 cells.
To investigate the differences in TGF-β downstream signaling activation in these cells, we focused on ERK phosphorylation and FLI-1 expression. TGF-β is known to activate ERK downstream of the Ras pathway, which cross-talks with Smad signaling and associates with FLI-1 activation. In U937 and NB4 cells, after rhTGF-β1 treatment, ERK phosphorylation was upregulated in the early phase (0.5-3 h) and then downregulated (24 h), and FLI-1 expression was downregulated (mRNA and protein, 24 h). Protein phosphatase 2A (PP2A), a modulator of TGF-β and a negative regulator of p-ERK, was downregulated by rhTGF-β1. ERK is known to participate in multiple feedback loops that include its upstream regulator Ras, which is important for the reduction of ERK activity at a late stage after stimulation. Indeed, p-Raf, a direct upstream regulator of p-ERK, demonstrated concordant expression changes with p-ERK after rhTGF-β1 treatment. No changes in p-ERK and FLI-1 expression were detected in OCI-AML3 cells. rhTGF-β1 induced significant upregulation of anti-apoptotic Bcl-2 in NB4 and U937 but not in OCI-AML3 cells.
We next investigated the rhTGF-β1–induced expression of CD44 and its variant CD44v. CD44 is recognized as a marker of cancer stem cells, and CD44v regulates redox status in stem-like cancer cells. In several types of cancer cells, CD44 is known to mediate cell migration via interaction with TGF-β type I receptor and close association with ERK signaling. Treatment with rhTGF-β1 increased both total and variant CD44 mRNA in NB4 cells but caused no change in OCI-AML cells (fold change of CD44/CD44v mRNA compared to controls: NB4, 3.0/3.7; OCI-AML3, 1.2/0.9). These changes were inversely correlated with FLI-1 expression in NB4 cells.
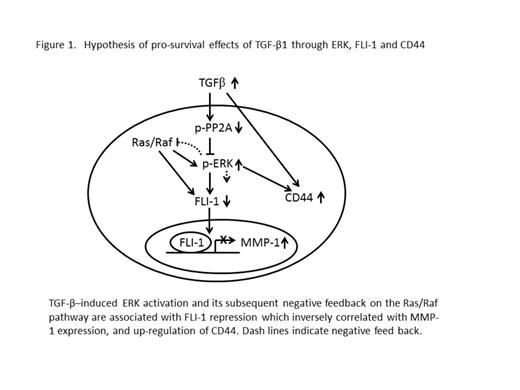
Taken together, these results show that TGF-β–induced ERK activation and its subsequent negative feedback on the Ras/Raf pathway are associated with FLI-1 downregulation and other responses, including CD44 upregulation, in AML in a cell-dependent manner (Figure 1). These molecular changes might contribute to maintenance of the stem cell–like properties, support survival of AML cells, and play pathologic roles in the TGF-β–abundant BM microenvironment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.