Abstract
Allogeneic hematopoietic cell transplantation (HCT) is a curative treatment option when indicated for myeloid malignancies such as acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS). The Disease Risk Index (DRI, Armand et al, 2012) has been developed to predict overall survival and progression-free survival on the basis of differences in relapse risk. The purpose of this single-center study was to retrospectively investigate the prognostic value of the DRI on the outcome of 470 patients that underwent HCT for AML and MDS between 2000 and 2013.
AML patients (n=381) underwent HCT in first and second complete remission and MDS patients (n=89) underwent HCT untreated or in remission. Median age at HCT was 51 (range 18-71), 219 (47%) patients were female. Myeloablative conditioning (MAC) was used in 304 (65%) patients, reduced-intensity (RIC) in 166 (35%) patients. Donors were related for 287 (61%) patients, unrelated for 183 (39%) patients. Grafts were peripheral blood stem cells (PBSC) in 377 (80%) patients and bone marrow in 93 (20%) patients. Median follow-up of patients alive was 44 months (range 1-134). In accordance with the DRI criteria, all 470 patients were in the low risk group concerning disease stage. Concerning disease biology characterized by cytogenetic risk, 11 patients were low risk, 396 patients were intermediate risk and 63 patients high risk. Based on the DRI overall risk stratification, 11, 396 and 63 patients were low, intermediate and high risk respectively.
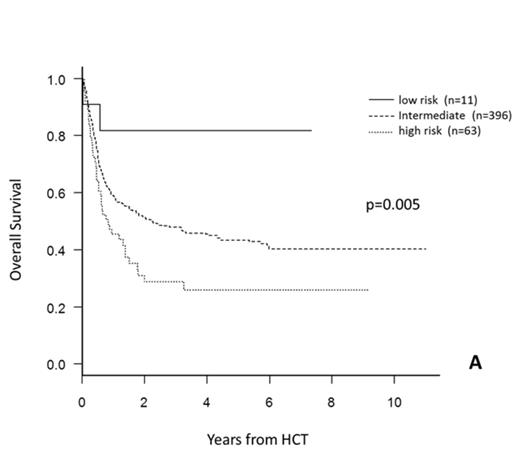
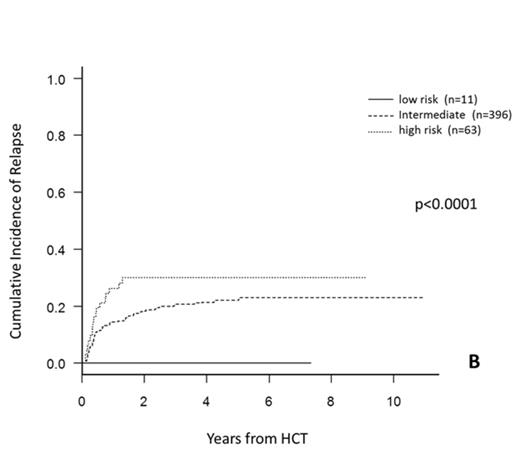
Univariate analysis demonstrated that the DRI was significantly prognostic for overall survival (OS) with a 3-year OS of 82%, 48% and 29% for low, intermediate and high risk patients respectively (p=0.005, Figure A). For cumulative incidence of relapse (CIR), DRI was again prognostic with 3-year CIR 0%, 21% and 30% for low, intermediate and high risk patients respectively (p<0.0001, Figure B). For non-relapse mortality (NRM), DRI did not demonstrate significant prognostic relevance with 3-year NRM 18%, 32% and 43% for low, intermediate and high risk patients respectively (p=0.14).
Multivariable analysis for OS confirmed the prognostic significance of the DRI with hazard ratio (HR) 3.3 and 4.9 for intermediate and high risk respectively compared to low risk (p=0.01). For CIR, DRI was highly significant (p<0.0001) while for NRM, the DRI was not predictive (p=0.22). This study confirms the prognostic relevance of the DRI for OS and CIR in our cohort of patients undergoing HCT for AML and MDS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.