Abstract
The allogeneic hematopoietic stem cell transplantation (HSCT) is the only curative treatment in patients with MDS. Indeed, many retrospective studies have shown that the higher risk patients according to IPSS (intermediate-2 and high) have a better overall survival with HSCT if performed at time of diagnosis while HSCT in lower risk patients (low and intermediate-1) should be postponed. Actually, some lower risk patients have poor prognostic features leading to propose the transplantation before they evolve to a higher risk. In this registry study from the CMWP, we analyzed outcome of patients who were diagnosed low risk MDS and who finally were transplanted without evolving to a higher risk. As more and more of these patients are proposed to the transplantation, their survey may give information about their prognostic risks.
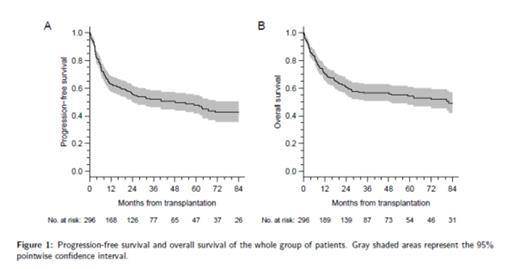
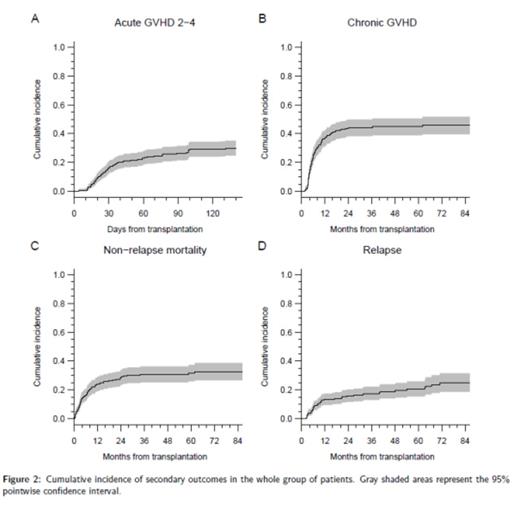
All adult patients transplanted between 2000 and 2011 and registered in the EBMT registry could be included if they have a low risk MDS at time of diagnosis and at time of transplantation. Overall and progression-free survival (OS and PFS) were estimated using Kaplan-Meier product limit estimator. For competing risk, cumulative incidence functions were estimated using usual methodology. Cox proportional hazard model were used to test the potential risk factors (age, gender, CMV recipient/donor, disease, IPSS, transfusion, donor type, conditioning). Missing data were handled through multiple imputations by chained equations methods.
291 patients met the inclusion criteria: 126 women and 165 men. Median age at diagnosis was 53 years and inter-quartile range (IQR) from 44 to 59. The majority of patients have refractory anemia or refractory cytopenia with multilineage dysplasia (66%), while one third of patients have refractory anemia with excess blasts. Most patients were intermediate-1 (80%) and required transfusions before the transplantation (84%). Median age at time of transplantation was 55 years (IQR: 46-60). Median time from diagnosis to transplantation was 11 months (IQR: 7-22). Donor was an HLA matched sibling in 122 (42%) patients and an unrelated donor in the remaining patients. The preferred source of stem cells was peripheral blood stem cells (PB) (78%) followed by bone marrow (19%) and cord blood (3%). Conditioning regimen consisted in a reduced intensity conditioning regimen in the majority of patients (59%) and 58% received an in vivo T depletion.
PFS and OS of the whole patients are shown in Figure 1 A and 1 B. Cumulative incidence of grade II-IV acute GVHD, chronic GVHD, non-relapse mortality and relapse are shown in Figure 2 A-D. Multivariate analysis with original data set (excluding missing data) found the following factors as poor prognostic for PFS: age < 35 years (Hazard ratio (HR): 4.22, p=0.009) or > 45 years (p<0.05), blast count in bone marrow > 5% (HR: 1.67, p=0.05), bone marrow (HR: 2.18, p=0.003) or cord blood (HR: 5.28, p=0.014) as sources of stem cells rather than PB and CMV serostatus positive for the recipient and negative for the donor (HR: 2.50, p=0.002) while transfusion before the transplantation (HR): 0.51, p=0.013) and T-depletion (HR: 0.60, p=0.43) were protective. The second multivariate analysis included all patients with imputed datasets showing similar results.
To conclude, outcome after HSCT in patients with lower risk IPSS are better than those observed in higher risk. In favorable transplant condition (PB, T-depletion), expected OS reaches 70% with a low mortality rate after the second year which could be a valid option in some lower risk patients presenting some high risk factors as poor molecular biology or resistance to agents stimulating erythropoiesis.
Blaise:Sanofi: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal