Abstract
Background: Primary mediastinal (PMBL), GCB and non-GCB B-cell lymphoma are three major subtypes of DLBCL with distinct clinical outcomes. PMBL and DLBCL of GCB immunophenotype have a higher chance of cure than patients with non-GCB DLBCL when treated with conventional chemotherapy. In the relapsed/refractory setting, there is paucity of data regarding the impact of histological classification of DLBCL on survival following alloSCT in patients who were not eligible for or who have failed a prior autologous SCT (ASCT). Herein, we compare outcomes of alloSCT in these patients.
Methods and Patients: We identified 101 de novo DLBCL patients who were treated at our center from January 1, 1998 to December 31, 2011. Seventeen (17%) tumors were PMBL. We determined the cell-of-origin in the remaining patients, based upon the Visco/Young and Choi immunohistochemical algorithms, and classified 62 (61%) as GCB and 22 (22%) as non-GCB tumors. GCB patients were older than non-GCB [median (range): 54 (21-70) vs 48(24-58) years, p=0.003)] and PMBL [26(19-48), P <0.001)]. Patients with PMBL, however, were more likely to have bulky disease at study entry (SE) than other subtypes [24% (PMBL) vs 5% (GCB) and 5% (non-GCB); P= 0.04]. Stage III-IV at SE in GCB, non-GCB and PMBL was present in 42%, 45% (P=0.8) and 35% (P=0.6), respectively; the number of prior chemotherapies received was 4 in both GCB and non-GCB and 5 in PMBL (P=0.3). The proportion of patients who have failed a prior ASCT was comparable in all three groups (32%, 32% and 47%, P=0.2). Refractory disease was present in 35% of GCB and PMBL patients at SE compared to 14% in non-GCB patients (P=0.03). Distribution of IPI, LDH, and proportion of PET+ patients (47%, 45% and 47%) were not statistically different in all 3 groups. A larger proportion of GCB patients (44%, reference) received non-myeloablative conditioning than non-GCB (23%, P=0.07), or PMBL (12%, P=0.3); the remaining patients received reduced-intensity conditioning (RIC). The proportion of patients who received a matched sibling donor in GCB, non-GCB and PML were 69% (reference), 64% (P=0.6) and 41% (P=0.03), respectively. The remaining patients received matched unrelated donors. More GCB patients received peripheral blood as stem cell source than non-GCB (89% vs 73%, P=0.08) or PMBL (47%, P=0.001) patients. Median year of transplant was 2006 in both GCB and non-GCB and 2004 in PMBL.
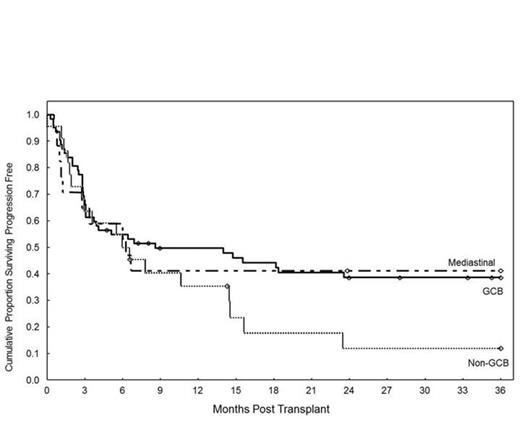
Results: Median (range) follow-up months in surviving GCB, non-GCB and PML patients were 63 (5-157), 29 (7-117) and 52 (10-133) months respectively. The 3-year cumulative OS were 52% (reference), 18% (P=0.09) and 46% (P=0.6). The 3-year cumulative PFS were 39%, 12% (P=0.1) and 41% (P=0.9) (Figure). When we restricted the comparison to patients who had chemosensitive disease and received RIC, the 3-year OS rates for GCB, non-GCB and PMBL were 47%, 25% (HR=0.6, P=0.3) and 44% (HR=0.9, P=0.9), respectively. The 3-year PFS rates were 37%, 10% (HR=0.6, P=0.2) and 44% (HR=0.7, P=0.8). Non-relapse mortality at 3-years was 29% (reference), 47% (P=0.1), and 35% (P=0.6). The incidence of acute II-IV GVHD was 24%, 27% and 29%. The incidence of extensive chronic GVHD was 34%, 54% (P=0.07) and 41% (P=0.5). The major cause of death in all 3 subgroups was disease progression (38%, 38%, and 33%), followed by acute GVHD 14%, 13%, and 33%.
Conclusions: Our results suggest a tendency for inferior survival after alloSCT in non-GCB when compared to GCB and PMBL subtypes of DLBCL. This occurred despite the younger age in the non-GCB versus GCB group. Innovative approaches are needed to improve outcomes in non-GCB patients after alloSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.