Abstract
Introduction: Accurate and rapid diagnosis is essential in acute venous thromboembolism (VTE) to help prevent significant morbidity and mortality. Soluble P-selectin (sP-sel) is a cell surface ligand that aids in cell adhesion. It is released from activated platelets and damaged endothelial cells resulting in release of procoagulant molecules from leukocytes and aiding in thrombus generation. Our lab has previously shown elevated sP-sel is highly predictive of VTE in combination with clinical probability (Wells score). Current standards for ruling out VTE include combining Wells Score and plasma D-dimer; however, D-dimer increases with age and is less useful in the elderly. Age adjusted D-dimer, defined as 10*age in patients ≥50 years old, has been described as being more sensitive, which could rule out more clots in the elderly, sparing them from other diagnostic tests.
Methods: We performed a prospective cohort study of patients ≥18 years old who presented with symptoms of deep venous thrombosis (DVT) in upper or lower extremities from December 2008 to July 2013. Exclusion criteria included isolated calf DVT, superficial thrombosis, indeterminate duplex scans, pregnancy or nursing mothers, therapeutic anticoagulation, and symptoms of simultaneous upper and lower extremity (LE) clot. After informed consent was obtained, biomarkers were drawn and duplex ultrasound was used to confirm or deny presence of acute clot. Our objective was to examine the accuracy of biomarker combinations and clinical probability score to rule in or rule out acute venous thrombus.
Results: We recruited 461 patients to the study. Patients with positive lower extremity DVT were significantly more likely to be male, have a prior history of DVT, have active cancer or history of cancer, and be inpatient.
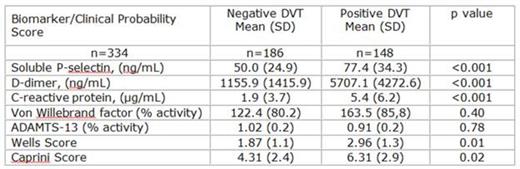
Biomarkers and Clinical Probability Score of Patients Presenting with Symptoms of LE DVT
Biomarkers and Clinical Probability Score of Patients Presenting with Symptoms of LE DVT
There were no significant differences in biomarkers between upper and lower extremity VTE aside from non-significance of sP-sel in upper extremity clots.
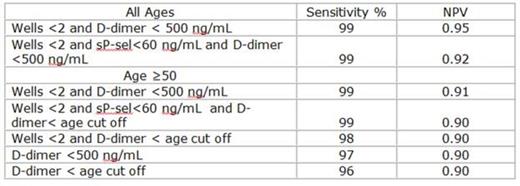
We calculated the specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) of several combinations of biomarkers and clinical probability assessment.
Specificity and PPV
Sensitivity and NPV
Using the age adjusted D-dimer did not improve the overall sensitivity when compared to the traditional cut off. However, sub-analysis demonstrated using D-dimer <500 ng/mL in those ≥ 50 ruled out 35 patients while the age adjusted D-dimer ruled out an additional 17 patients (12% increase). An additional 10% of patients ≥60 years were ruled out using the age adjusted D-dimer alone; this benefit rose to 15% in patients ≥70 years old. Use of the age adjusted D-dimer did not increase false negative results.
Conclusions: We found Wells ≥ 2 and sP-sel ≥ 90 ng/mL had the highest specificity of any combination of biomarkers, highlighting its clinical utility as a predictive biomarker of thrombosis. Using this combination would allow clinicians to accurately rule in venous thrombus without need for further imaging. In this study, we would have successfully identified 48 (25%) patients with acute thrombus without duplex ultrasound. Compared to the traditional cut off value, age adjusted D-dimer did not increase sensitivity in those >age 50, but its utility increased with age, making it a promising biomarker to safely rule out thrombosis in the elderly.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.