Abstract

Background: Currently, among HLA-8/8, or 7/8 allele-matched unrelated donor (UD) and umbilical CBT (UCBT), HLA-8/8 allele-matched UD transplantation (UDT) showed superior overall survival (OS) to 7/8 allele-matched UDT and UCBT, while a similar OS has been demonstrated between the HLA-7/8 allele-matched UDT and the UCBT. It has been observed that recipients of CB had higher earlier mortality including graft-failure or severe infections. However, less graft-versus-host disease (GVHD) and associated complications brought less long-term mortality, which compensate the early deaths. Thus we hypothesized that UCBT may demonstrate comparable outcomes with 8/8 allele-matched UDT in updated long-term analyses.
Methods: The purpose of the current study is to compare the transplant outcomes of 8/8 and 7/8 allele-matched BMT with those of CBT, and redefine the role of CBT. Because the most of UDT in Japan is still BM transplantation, we analyzed the transplant outcomes in younger adult patients (age, 16-50) receiving UCBT in comparison with those receiving 8/8, 7/8 and 6/8 allele-matched unrelated BMT (UBMT) for acute lymphocytic leukemia (ALL) and acute myeloid leukemia (AML) using a Japanese registry database (TRUMP data). Also we included 6 out of 6 HLA-allele data available UCBT so that we could analyze each allele-mismatch effect within UCBT group.
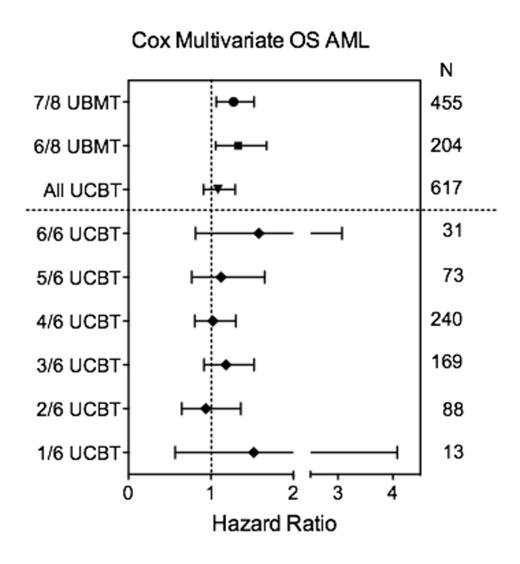
Results: A total of 3,062 first transplants between 2001 and 2010 were included. [AML: 8/8 UBMT, 676; 7/8 UBMT, 455; 6/8 UBMT, 204; CB; 617][ALL: 8/8 UBMT, 418; 7/8 UBMT, 267; 6/8 UBMT, 120; CB, 305] For AML, CR1 and CR2 are defined as standard risk and others are as advanced risk. For ALL, CR1 is defined as standard risk and others are as advanced risk disease. Advanced risk patients were significantly more in the UCBT group. With adjusted analyses for AML, UCBT and 8/8 UBMT showed similar OS, while 7/8 and 6/8 UBMT showed inferior OS [8/8 UBMT as reference: CB; Hazard ratio (HR) =1.08 (95% confidence interval (95%CI), 0.91-1.29), p=0.37: 7/8 UBMT; HR = 1.27 (95%CI, 1.06-1.52), p=0.009: 6/8 UBMT; HR =1.33 (95%CI, 1.06-1.67), p=0.015]. The 4-year unadjusted OS was 65.9% (95% CI, 60.6-70.7) for 8/8 UBMT and 61.8% (95%CI, 55.0-67.9) for UCBT in standard risk patients, while 28.1% (95%CI, 21.6-34.9) for 8/8 UBMT and 30.3% (95%CI, 25.0-35.8) for UCBT in advanced risk patients. For ALL, there is no significant difference in OS among 4 groups in adjusted analyses. The 4-year unadjusted OS was 64.3% (95%CI, 57.3-70.5) for 8/8 UBMT and 65.7% (95%CI, 56.1-73.7) for UCBT in standard risk patients, while 28.5% (95%CI, 20.2-37.3) for 8/8 UBMT and 30.2% (95%CI, 21.6-39.2) for UCBT in advanced risk patients. There is no significant difference in the risk of relapse among 4 groups for both AML and ALL. Non-relapse mortality (NRM) in AML after UCBT was comparable with 8/8 UBMT, while 7/8 and 6/8 UBMT had higher NRM [CB; HR =1.12 (95%CI, 0.85-1.47), p=0.43: 7/8 UBMT; HR = 1.51 (95%CI, 1.16-1.96), p=0.002: 6/8 UBMT; HR =1.55 (95%CI, 1.12-2.16), p=0.009]. The 2-year unadjusted NRM of AML for 8/8, 7/8, 6/8 UBMT and UCBT was 16.5% (95%CI, 13.0-20.5), 24.2% (95%CI, 19.1-29.7), 26.0% (95%CI, 18.3-34.4) and 20.0% (95%CI, 15.2-25.3) in the standard risk group, respectively, while 21.4% (95%CI, 15.9-27.4), 30.7% (95%CI, 23.3-38.4), 26.7% (95%CI, 16.8-37.6) and 19.0% (95%CI, 15.0-23.5) in the advanced risk group respectively. For ALL, the adjusted NRM is not significantly different between 8/8, 7/8 UBMT and UCBT, although 6/8 UBMT alone demonstrated higher risk of NRM. To examine the allele-mismatch effect in UCBT group, we further compared OS/NRM of each allele-mismatch UCBT with UBMT in the cox's multivariate analysis [8/8-, 7/8-, 6/8-UBMT, 6/6-, 5/6-, 4/6-, 3/6-, 2/6- and 1/6-UCBT]. Each allele-mismatch UCBT group showed comparable HR with 8/8 UBMT group (Figure). There was no significant difference among each allele-mismatch group.
Conclusion: These data suggest that CB may be the first choice alternative to 8/8 UBM for AML. For ALL, 8/8 UBM is the first choice, however, CBT will convey comparable outcomes with 7/8 UBMT. The survival after UCBT is approaching to that after 8/8 UBMT in recent years.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract