Abstract
Introduction: Recent studies have established that concurrent MYC and BCL2 protein expression by immunohistochemistry (IHC) identifies a subgroup of patients with diffuse large B-cell lymphoma (DLBCL) with a poor outcome. Classic dual translocation MYC/ BCL2, so called double hit' disease, is associated with a high risk of central nervous system (CNS) relapse; however the impact of concurrent MYC and BCL2 protein expression on the risk of CNS relapse remains unknown. Further, robust biological markers that accurately predict the risk of CNS relapse in DLBCL would also be of value in clinical practice.
Methods: Cases of pre-treatment formalin fixed paraffin embedded DLBCL in two tissue microarrays were independently scored by two expert hematopathologist (GWS and KLT or PF and AM) for expression of MYC (Epitomics Y69), BCL2 (Dako 124), CD10, BCL6 and MUM1 by IHC. MYC and BCL2 positivity were defined as ≥ 40% and ≥ 50% cells with staining, respectively, in accordance with previously established cutoffs (Johnson, JCO 2012; 30). Cases with discordant scores were reviewed by a third hematopathologist (RDG) to reach a consensus. Cell of origin (COO) was assigned according to the Hans IHC algorithm (Hans, Blood 103: 2004) as well as by the recently described gene expression profiling Lymph2Cx 20 gene assay based on NanoString technology (Scott, Blood 2014; 123) in the subset of patients with ≥ 40% tumor content. Patients treated with at least one cycle of R-CHOP chemotherapy with curative intent were included and those with established CNS disease at diagnosis were excluded.
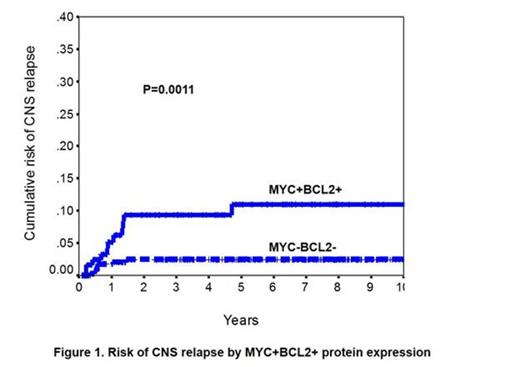
Results: 447 patients were identified with the following baseline clinical characteristics: Median age 65 y (16-92y); males n=280, 63%; performance status ≥ 2, n= 147, 33%; stage 3 or 4 disease n=242, 54%; elevated LDH n=219, 47%; EN > 1 n= 80, 17%. With a median follow-up of 6.75 years for living patients, the 3 year time to progression, progression-free and overall survival for all patients were 68%, 66%, and 73%, respectively. In total, 131 (29%) were MYC+BCL2+ and 316 (71%) were non-MYC+BCL2+. By COO assignment using the Hans algorithm (n=444), 192 were non-GCB (43%) and 252 were GCB (57%) and by the Lymph2Cx (n=308); 103 were ABC (33%), 172 were GCB (56%) and 33 (11%) were unclassifiable. The 2 year cumulative risk of CNS relapse for the whole cohort was 4.3%. The cumulative risk of CNS relapse was higher in cases that were MYC+BCL2+ (2 year risk 9.4% vs 2.4%, P=0.001) with similar results obtained if classic MYC+BCL2+ double hit cases are excluded. There were no cases of CNS relapse in cases MYC+ alone by IHC. By COO, patients with a non-GCB phenotype by the Hans algorithm had an increased risk of CNS relapse (2 year risk 6.9% vs 2.6%, P=0.03) and similarly, cases assigned as ABC DLBCL by the Lymph2Cx assay also identified a group with a higher risk of CNS relapse compared to GCB cases (9.5% vs 2.5%, P=0.03) (Figure 1). In Cox regression multivariate analysis including the COO (Hans), IPI group (0/1 vs 2/3 vs 4/5) and MYC/BCL2 IHC, only the IPI (HR 2.18, P=0.02) and MYC+BCL2+ IHC (HR=3.76, P=0.007) were associated with an increased risk of CNS relapse. Similar results were obtained using the Lymph2Cx COO designation. Within the IPI risk groups, MYC+BCL2+ status further stratified patients in the intermediate risk group (IPI 2 or 3, n=206) into a higher risk group (2 year CNS relapse 12.6%) and a low risk group (2 year CNS relapse 2.9%) (P=0.01). A similar trend was observed in the high IPI risk group (IPI 4 or 5, n=86, 2 year CNS relapse MYC+BCL2+ 17.2% vs 4.7%, P=.0.18) but it was not useful in the low IPI risk group (IP1 0 or 1 (n=155), 2 year CNS relapse 4% vs 1%, P=0.39) where the overall risk was low. Within the COO subgroups, MYC+BCL2+ status also defined a group at high cumulative risk of CNS relapse within the non-GCB subtype (12.9% vs 3%, P=0.001) and by the Lymph2Cx defined ABC subtype (16.9% vs 2.2%, P= 0.03) and a trend was observed for GCB defined by Lymph2Cx (6.6% vs 1.5%. P=.08) but not by Hans criteria (P=0.40).
Conclusion: Concurrent expression of MYC and BCL2 protein in DLBCL defines a group of patients at high risk of CNS relapse, independent of the IPI and COO. MYC+BCL2+ status may help to further risk stratify patients in the intermediate and high IPI risk groups and within the ABC subtype to identify patients who should undergo additional diagnostic testing and in whom to explore the effectiveness of prophylactic CNS strategies.
Savage:F Hoffmann-La Roche: Other. Sehn:Roche: Research Funding. Connors:Seattle Genetics, Inc.: Research Funding; Roche: Research Funding. Gascoyne:Hoffman La-Roche: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.