Abstract

Background: Retrospective analyses have demonstrated significantly improved survival for AYA ALL patients (pts) aged 16-21 years (yrs) when treated on pediatric versus adult U.S. NCI Cooperative group regimens where 2-yr event-free survivals (EFS) have been only 35-40%. The purpose of C10403, a large prospective US intergroup trial, was to evaluate the feasibility and effectiveness [with EFS as a primary endpoint), of treating AYA ALL pts (ages 16-39 yrs) using the standard arm of the successful Children's Oncology Group regimen (COG AALL0232) .
Methods: Newly diagnosed AYA patients with B-precursor (B-ALL) or T-precursor (T-ALL) ALL were eligible to enroll on C10403. Burkitt type and Ph+ ALL were excluded. The regimen was identical to the Capizzi methotrexate arm of COG AALL0232 (Larsen E. JCO 2011; 29 suppl:3) and consisted of four intensive courses: remission induction, remission consolidation, interim maintenance, delayed intensification, and prolonged maintenance therapy. Pts with M2 marrow response (>5% but < 25% lymphoblasts) after remission induction received an extended remission induction course of therapy. Events were defined as induction failure (M3 [³25% blasts] day 29 of induction or M2 day 43 of extended induction), death, relapse, or second malignancy. Key correlative science studies in a subset of the total accrued population included assessment of Minimal Residual Disease (MRD) using quantitative real-time PCR of clonal IgH or TCR gene rearrangements as well as Low Density Microarray (LDA) assays designed to detect a previously validated gene expression profile (Harvey, R; ASH 2013, abstract 826) which can prospectively identify ALL pts with Ph-like (BCR-ABL1-like) ALL.
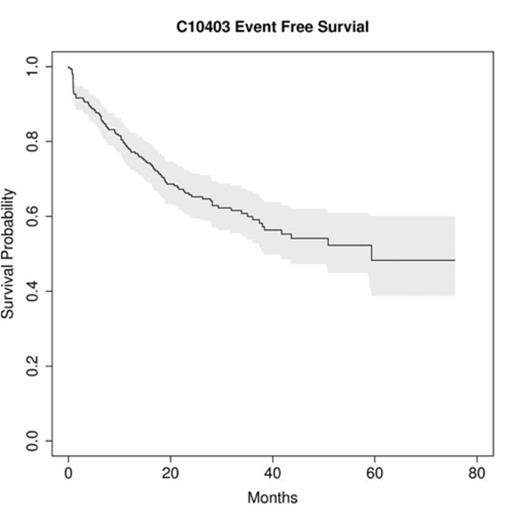
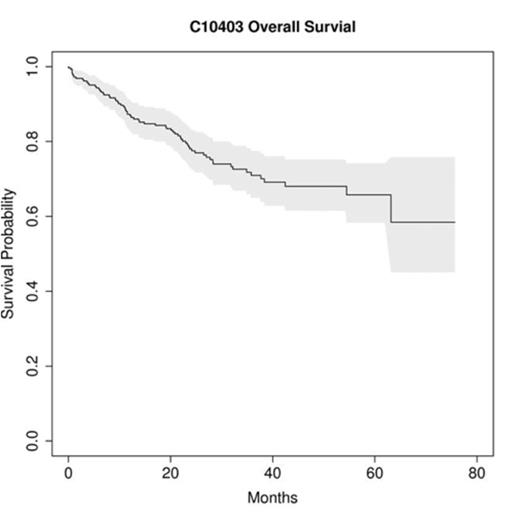
Results: 318 pts were enrolled on C10403 from 11/2007 to 8/2012; 22 withdrew prior to therapy. Of 296 evaluable pts, the median age at diagnosis was 24 yrs (range: 17 to 39): 25% were 17-20 yrs, 53% were 21-29 yrs, and 22% were 30-39 yrs. The majority had B-ALL (76%) and were male ( 61%). Approximately 25% were non-Caucasian and 15% were Hispanic or Latino. 32% of pts were obese (BMI³30). There were 5 (2%) treatment-related deaths during protocol therapy: liver failure (n=2, both during induction), infection (1 in induction, 1 in consolidation), and ventricular arrhythmia (1 in induction). Overall, treatment toxicities were similar to those reported in the standard arm of COG AALL0232, with an increased thrombosis and early hyperbilirubinemia for C10403 pts, as reported previously (Advani A, ASH 2013, abstract 303). To date, 70 deaths have been reported and 87 pts remain on protocol therapy. With a median follow-up of 28 months for surviving pts, 105 events have been observed. The median EFS overall is 59.4 months (95% CI: 38.4 to NR) and the 2-yr EFS rate overall is 66% (95% CI: 60 – 72%) [Fig 1a] with similar 2-yr EFS rates for B and T- ALL pts (65%, and 68%). The 2-yr OS rate is 78% (95% CI: 72 – 83%)[Fig 1b], which is similar for B (78%, 95% CI: 72 – 84%) and T-ALL, (80%, 95% CI: 70 – 91%). These results allow rejection of the null hypothesis of this Phase II trial that the true median EFS is, at most, 32 months. In multivariable analysis of presenting clinical features, age > 20 years and initial WBC count ³ 30k/microliter were significantly associated with worse EFS and OS. Presence of MRD at day 28 following initiation of induction therapy and presence of a Ph-like gene expression signature were significantly associated with both worse EFS and OS. Notably, absence of detectable MRD noted in 22/58 [38%] evaluable pts at day 28 of induction was associated with 100% EFS (p=0.0006). The Ph-like like signature was detected in 28% of pts tested on C10403 and the 2 yr EFS for these patients was only 52%, compared to 81% for those without Ph-like disease (p = 0.04).
Conclusions: This large prospective US adult intergroup trial (C10403) for pts 16-39 years old employing an intensive pediatric regimen demonstrates a significant improvement (compared to historical controls) in AYA EFS and OS and validates this approach for treatment of AYA with ALL by adult hematologists. The improved clinical outcomes and the predictive value of the correlative studies in this trial lay the foundation for the design of future trials, where incorporation of novel agents to eradicate MRD, and/or use of tyrosine kinase inhibitors to target the frequently detected Ph-like ALL in AYA pts may further improve survival for young adults with ALL.
Stock:Sigma-Tau: Membership on an entity's Board of Directors or advisory committees, Research Funding. Advani:Sigma Tau: Membership on an entity's Board of Directors or advisory committees; Jazz: Membership on an entity's Board of Directors or advisory committees. Liedtke:Onyx: Membership on an entity's Board of Directors or advisory committees. Larson:Novartis: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract