Abstract
Introduction: Advances in treatment strategies and supportive care have resulted in a growing number of long-term survivors of hematologic malignancies. In the general U.S. population, CVD (heart failure, stroke, myocardial infarction) is a leading cause of morbidity and mortality, and cardiovascular risk factors (CVRFs: diabetes, hypertension and dyslipidemia) are well-established modifiers of CVD risk. Childhood (Circulation 2013 22;128) and young adult (<40y at diagnosis; JNCI2014 21;106) cancer survivors have a substantially increased risk of CVD when compared to the general population; this is largely attributable to exposure to cardiotoxic therapies (anthracyclines, radiation) at a young age. Less is known regarding the magnitude of risk of CVD in individuals with hematologic malignancies diagnosed at age ≥40y, a population that accounts for the largest proportion of new cancer diagnoses in the U.S. and has a high prevalence of CVRFs. The few studies addressing this issue have been limited by small sample size, short (<1y) follow-up, varying definitions of cardiovascular outcomes, and lack of comparison to non-cancer controls. The current study overcomes these limitations.
Methods: Using a retrospective cohort study design, 2,993 2+y survivors of non-Hodgkin lymphoma (NHL), lymphocytic leukemia (LL), and multiple myeloma (MM) diagnosed at age ≥40y between 2000 to 2007 and treated at Kaiser Permanent Southern California (KPSC) were included in the study. KPSC is the largest integrated managed care organization in Southern California, with documented 10-year insurance retention rates for cancer survivors exceeding 70% (JAYAO 2013 2:59). A non-cancer comparison group (N=6,272) was constructed by selecting individuals enrolled in KPSC and matched to cancer survivors (1:2) on age at diagnosis, sex, and zip-code. Cumulative incidence of CVD (ICD-9 definition: congestive heart failure, stroke, or myocardial infarction) was calculated, taking into consideration the competing risk of death. Definition of CVRFs (hypertension, diabetes, dyslipidemia) was per the National Cholesterol Education Program Adult Treatment Panel III criteria. Cox proportional hazards regression analysis was used to calculate hazard ratio (HR) estimates and 95% confidence intervals (CI), adjusted for relevant covariates.
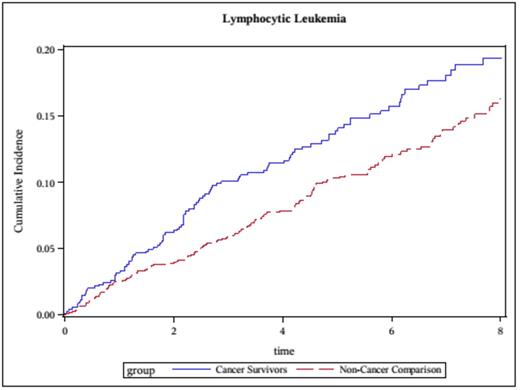
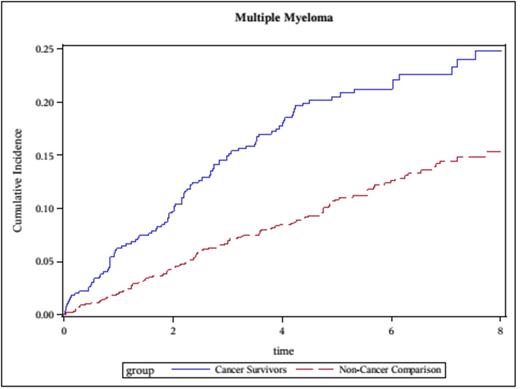
Results: Median age at cancer diagnosis was 63y (range: 40-96); 53.6% were male; 68% were non-Hispanic white; diagnoses: NHL (N=1,787 [59.7%]), LL (N=705 [23.6%], MM (N=501 [16.7%]). In cancer survivors, median time from cancer diagnosis to end of follow-up was 6.2 years (range: 2-10), representing 12,622 person-years of follow-up. Comparison with non-cancer cohort: The 8y cumulative incidence of CVD was significantly higher for NHL survivors (17% vs. 14%, p<0.01), LL (19% vs. 16%, p=0.02), and MM (21% vs. 11%, p<0.01), when compared to non-cancer subjects (Figures). Multivariable analysis adjusted for age, sex, race/ethnicity and CVRFs revealed a significantly increased risk of CVD across all cancer diagnoses (NHL: HR=1.3, 95%CI, 1.1-1.6; LL: HR=1.3, 95%CI, 1.0-1.6, MM=1.9, 95%CI, 1.5-2.5) when compared to non-cancer subjects; younger (<65y at diagnosis) MM survivors were at highest risk (HR=3.5, 95%CI, 2.2-5.6). Modifiers of CVD risk among cancer survivors: Hypertension and diabetes were independent modifiers of CVD risk. Hypertension was associated with a 1.9-fold (95%CI,1.1-3.3) increased risk of developing CVD in NHL survivors and a 3.1-fold (95%CI, 1.4-6.7) increased risk in MM survivors. Diabetes was associated with increased CVD risk across all diagnoses (NHL: HR=1.7, 95%CI, 1.2-2.4; LL: HR=1.6, 95%CI, 1.0-2.6; MM: HR=1.6, 95%CI, 1.0-2.3).
Conclusions: Survivors of adult-onset NHL, LL and MM are at increased risk for developing cardiovascular disease when compared to a matched non-cancer cohort. Cardiovascular risk factors such as hypertension and diabetes are independent modifiers of risk of delayed cardiovascular disease. Taken together these data form the basis for identifying high-risk individuals for targeted surveillance, as well as aggressive management of cardiovascular risk factors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.