Abstract
Fibrinogen is a critical protein for hemostasis and clot formation. However, transfusion guidelines have variable recommendations for maintaining fibrinogen levels in bleeding patients. An increasing number of studies support the practice of fibrinogen replacement therapy for acquired coagulopathies, and additional studies are underway. Fibrinogen therapy can be administered with cryoprecipitate or fibrinogen concentrates, and clinical practice varies according to their availability and licensing status. Fibrinogen concentrate therapy has been studied in animal models and clinical trials and supports the critical role of fibrinogen repletion in bleeding patients. Point-of-care testing will have an important role in guiding fibrinogen replacement for hemostatic therapy in clinical settings such as cardiovascular surgery, postpartum hemorrhage, and trauma. Fibrinogen therapy is an important component of a multimodal strategy for the treatment of coagulopathic bleeding.
Introduction
Fibrinogen is a critical protein for clot formation, providing a matrix and mesh network essential for clot strength. Maintaining fibrinogen levels is an important therapeutic target in bleeding patients, particularly in perioperative settings.1-3 Early studies demonstrated that fibrinogen repletion corrected clot strength, based on viscoelastic blood testing using thromboelastography/thromboelastometry.4 Normal fibrinogen levels are elevated during pregnancy,5 and cases studies indicate that fibrinogen repletion may be effective in the treatment of postpartum hemorrhage.6,7 Additionally, studies have been published, or are underway, that provide supporting evidence for the role of fibrinogen repletion for treating acquired coagulopathy.1,8-10 Although precise levels for fibrinogen repletion remain to be defined as a therapeutic trigger or target, we review the current evidence and provide therapeutic perspectives in clinical settings.
The role of fibrinogen and related proteins in clot formation
A 62-year-old 110-kg man underwent first-time cardiac surgery with a valve sparing aortic root replacement. Preoperative medications included a statin and beta-blocker. Intraoperatively, 52 000 units of heparin were administered and reversed with 250 mg of protamine. He was empirically transfused plasma (4 units) and pheresed platelets (2 units) for bleeding. In the intensive care unit (ICU) he was warm, hemodynamically stable, but bleeding ∼150 mL/h. Coagulation tests obtained on ICU arrival included activated clotting time, 120 seconds; platelet count, 115 000; international normalized ratio, 1.3; partial thromboplastin time (PTT), 37 seconds; and fibrinogen, 120 mg/dL (1.2 g/L).
Question: What therapy should be considered to treat the bleeding?
Fibrinogen is a hepatically synthesized 340-kDa plasma glycoprotein that is the substrate for thrombin, plasmin, and factor XIIIa, with a half-life of 3 to 5 days.11 Following tissue injury, fibrinogen is cleaved by thrombin and generates soluble fibrin monomers that create a net that entraps red blood cells (RBCs) to form a clot. The fibrin polymers are cross-linked by factor XIIIa, improving clot strength and preventing fibrinolysis. Fibrinogen also binds to platelet glycoprotein IIb/IIIa receptors to promote platelet aggregation, further facilitating cross-linking and clot stabilization. Thus, fibrinogen is a critical component and substrate for clot formation, amplification, and strength.
Fibrinogen circulates at the highest concentration of the plasma coagulation factors. Following substantial blood loss and hemorrhage, hypofibrinogenemia occurs because of hemodilution from volume replacement and consumption by clot formation or as a result of disseminated intravascular coagulation.12-14 Thus, fibrinogen supplementation to restore plasma levels is an important component for normalizing clot formation in bleeding patients. Other coagulation factor levels are also diminished, resulting in complex coagulopathies in patients with substantial hemorrhage following surgery, trauma, and/or extracorporeal circulation. Factor XIII (FXIII) deficiency because of dilutional changes or consumption may also develop, contributing to bleeding perioperatively.15-17 Studies using thromboelastography to measure clot strength in FXIII-deficient plasma have demonstrated that changes in FXIII activity significantly increase clot strength.18 Therapeutic considerations in coagulopathic bleeding patients should therefore be multimodal, including not only fibrinogen replacement therapy but also addressing related coagulation abnormalities, such as antifibrinolytic therapy, and replenishing other factors.19,20
Target levels of fibrinogen for repletion
Question: What is the target level for increasing fibrinogen in the surgical and postoperative patient?
Normal reported fibrinogen levels vary but are generally considered to range from 2.0 to 4.5 g/L (200 to 450 mg/dL) and are increased in certain clinical settings such as pregnancy.5,21-23 Hypofibrinogenemia is reported to be a risk factor for hemorrhage in clinical scenarios including cardiovascular surgery,1,24 obstetrics,25-27 and trauma.28,29 The critical level of fibrinogen depends on multiple factors and clinical situations, and clinical studies are underway to better define target levels.30 The first report, from 1987, included 36 patients with massive hemorrhage and suggested that problems in hemostasis occurred when fibrinogen was <1.0 g/L.31 Clinicians still believe this is the threshold; however, increasing studies and consensus recommendations have revised target levels to at least 1.5 to 2.0 g/L with additional prospective, randomized studies underway.19,20,32-34
Many clinicians do not monitor fibrinogen levels with active bleeding or may believe the critical level to treat is 1.0 g/L, derived from nonbleeding patients with congenital fibrinogen deficiency. Additionally, fibrinogen concentrations <1.0 g/L affect clot-based laboratory tests, including prothrombin time (PT) or activated PTT.35 Previous guidelines following trauma or for surgery recommend a target of ∼1.0 g/L.36,37 Current studies and consensus guidelines suggest higher target levels in certain perioperative settings, including cardiovascular surgery, trauma, and other scenarios.19,20,25,32,33,38
Point-of-care coagulation testing using viscoelastic measurements of clot strength (maximal amplitude/maximum clot firmness [MCF]) is dependent on fibrinogen concentration.35,39 In vitro, a threshold of 2.0 g/L is required to optimize clot formation.9 However, studies report fibrinogen supplementation in surgical patients at higher levels.1,34,40,41 More recent European trauma guidelines from 2013 recommend fibrinogen administration at levels <1.5 to 2.0 g/L.20 In other settings, such as pregnancy, different therapeutic thresholds may need to be considered. In peripartum patients, fibrinogen levels increase to 500 to 600 mg/dL (5-6 g/L), and levels <2.0 g/L are considered to be highly predictive for risk of postpartum hemorrhage (PPH).5,25
Measuring fibrinogen levels
Question: What are the different ways to measure fibrinogen in the surgical bleeding patient?
Most assays used to measure plasma fibrinogen concentrations are functional assays that determine clot formation using either spectroscopic or viscoelastic clot detection. The Clauss assay uses citrated plasma to which thrombin is added, and the clot formation time is recorded via spectroscopic analysis.42 Thromboelastometry (ROTEM; TEM International, Munich, Germany) and thromboelastography (TEG; Haemonetics Corp., Braintree, MA) are increasingly used as point-of-care devices in perioperative settings and trauma that are modified to determine a functional fibrinogen levels using platelet activation inhibitors (cytochalasin or abciximab). Fibrinogen concentration based on Clauss measurements may be falsely decreased with direct thrombin inhibitors,43 falsely elevated with starch solutions,44 and optical or turbidometric detection methods can be affected more than the mechanical detection methods.45
Fibrinogen repletion
Question: What products can be used to replete fibrinogen levels in a bleeding patient?
Fibrinogen supplementation is based on the availability of cryoprecipitate and/or fibrinogen concentrates in individual countries. In many European countries (except the United Kingdom), lyophilized fibrinogen concentrates are used primarily, whereas cryoprecipitate and plasma are used in North America, the United Kingdom, and some European countries. Fibrinogen therapy using plasma, cryoprecipitate, and fibrinogen concentrates as a source of supplementation has been recently reviewed.30
Plasma
Plasma is transfused extensively in trauma and surgical patients.46 However, recent systematic reviews suggest there is no benefit for most clinical indications, except in trauma,46-49 and some studies report increased morbidity associated with its use.50,51 Different plasma preparations are available and used including single-donor fresh frozen plasma (FFP), plasma frozen within 24 hours of collection, and thawed plasma (used within 5 days of initial thaw); however, these products are not ideal sources for repletion, as fibrinogen concentrations can vary from 1 to 3 g/L.30 Transfusing plasma for fibrinogen repletion also requires large volumes that may be helpful for patients with trauma-induced coagulopathy who are bleeding and require volume replacement. A dose of 12.2 mL/kg increases plasma fibrinogen levels only 0.4 g/L, whereas 33.5 mL/kg increases levels by 1.0 g/L.52
Despite this information, clinicians continue to use plasma therapy for fibrinogen supplementation. A recent analysis evaluated the evidence for plasma use compared with fibrinogen concentrates from studies reporting bleeding, transfusion requirements, and fibrinogen levels in patients given plasma or fibrinogen concentrates in trauma or surgical settings.53 The authors found 70 plasma and 21 fibrinogen concentrate studies, mostly derived from observational data. The benefits or efficacy of plasma were inconsistent, with improved outcomes in 28% of the studies compared with worse outcomes in 22% of the studies. The authors noted a reduction of mortality in 50% of the massive bleeding or trauma patient studies, and increased mortality in 20% of nonmassive bleeding and surgical patients. The fibrinogen concentrate data included only 5 studies in which fibrinogen concentrate was assessed vs a comparator, of which 70% had improved outcomes. Overall, the risk of transfusion-associated circulatory overload and inability to replete fibrinogen levels precludes plasma as an effective therapy. Fibrinogen concentrates or cryoprecipitate are more effective at fibrinogen repletion.34,41
Cryoprecipitate
Cryoprecipitate, discovered by Judith Graham Pool, was used for treating patients with hemophilia A before the availability of lyophilized clotting factor concentrates.54 Cryoprecipitate is obtained by thawing FFP at 1°C to 6°C, centrifugation, and resuspending the precipitated proteins in plasma and refreezing.55 Cryoprecipitate also contains fibrinogen, von Willebrand factor, and FXIII and is used extensively as a fibrinogen source. Each unit of cryoprecipitate contains ∼200 to 250 mg of fibrinogen, and a standard dose is 8 to 10 units for adults, although fibrinogen concentration can vary among units.56 Cryoprecipitate repletes fibrinogen but is also used for deficiencies in von Willebrand factor and FXIII.
Because cryoprecipitate therapy is a multidonor product with no antiviral processing, it is not available in some countries because of safety concerns.57 However, alternatives to cryoprecipitate may not be available in all countries. Cryoprecipitate needs to be inventoried according to blood group compatibility and requires time for thawing and pooling before transfusion. Although widely used, studies and/or evidence for its use are limited.58 Guidelines suggest that cryoprecipitate should not be used to control bleeding related to low fibrinogen levels if specific factor concentrates are available.59
Fibrinogen concentrates
Commercial fibrinogen concentrates are available as pasteurized, lyophilized products from pooled donors that undergo purification, viral inactivation, and removal processes and do not require cross-matching.30,60 Four fibrinogen concentrates are currently approved and have been reviewed by both Levy et al30 and Franchini and Lippi.61 Haemocomplettan/RiaSTAP (CSL Behring) is the only fibrinogen concentrate globally available and is licensed in some countries for multiple indications including treating acute bleeding episodes with hypofibrinogenemia.
Fibrinogen dosing
Question: What dosing strategies and/or testing should be considered in a bleeding patient?
Fibrinogen can be dosed based on the level of bleeding and initial fibrinogen concentration. Where licensed for use perioperatively, 1 to 2 g should be administered initially if bleeding is accompanied by suspected low fibrinogen concentrations or function.19,30 However, dosing should depend on bleeding status and laboratory or point-of-care test results. The increasing use of point-of-care testing in trauma and surgery with ROTEM/TEG facilitates targeted coagulation factor repletion.62,63 The FIBTEM test (ROTEM device) has been used extensively to determine fibrinogen levels and calculate dosing as reported in clinical trials.1,34,64 Maximal amplitude, an equivalent parameter to MCF, can be measured using a functional fibrinogen assay on the TEG device. The fibrinogen dose can be calculated as follows: Fibrinogen concentrate dose (g) = [target FIBTEM MCF (mm) – actual FIBTEM MCF (mm)] × [body weight (kg)/70] × 0.5 g/mm.
Normal MCF values are 9 to 25 mm that correlate with normal fibrinogen levels65 ; however, a target MCF of 22 mm has been used in aortic surgery patients (achieved using mean fibrinogen doses of 5.7 g).40 In the algorithm by Weber, 25 mg/kg fibrinogen concentrate is recommended if EXTEM A10 and FIBTEM A10 are below 40 mm and 8 mm, respectively.66 If FIBTEM A10 is <6 mm and EXTEM A10 is <40 mm, the recommended dose increases to 50 mg/kg.66 Dosing strategies are reviewed in Table 1. Of interest is a publication by Collins, who developed a model that evaluates increasing fibrinogen levels by either plasma, cryoprecipitate, or fibrinogen concentrate.67
There is a perceived risk of triggering a thromboembolic event associated with fibrinogen supplementation, and that administering excessive fibrinogen, particularly with high thrombin generation, may increase the risk of systemic microthrombogenicity. However, post hoc analysis of a randomized clinical trial of fibrinogen concentrate reported fibrinogen supplementation was not associated with significant alterations of hemostatic parameters.68 In a porcine model, there were no reports of hypercoagulability or thromboembolism following treatment with fibrinogen levels up to 600 mg/kg.10
Clinical studies evaluating the role of fibrinogen therapy
Question: What is the data supporting fibrinogen repletion in surgical, trauma, and postoperative patients?
Fibrinogen repletion, primarily with the use of fibrinogen concentrates for acquired bleeding, has been reported in clinical settings including surgery, trauma, and obstetrics (reviewed by Levy et al30 ).
Trauma
Fibrinogen levels are decreased in trauma patients on admission and are associated with poor outcomes.69 Fibrinogen repletion is increasingly used as hemostatic treatment of trauma-induced coagulopathy, especially with concentrates.62,70 However, hypovolemic patients are initially resuscitated with plasma following a massive transfusion protocol. Additional therapy includes measuring fibrinogen levels and specific repletion as part of a subsequent multimodal therapy that includes antifibrinolytic therapy with tranexamic acid, surgical correction, and other therapies.
Fibrinogen and other factor concentrates are increasingly being studied and reported in surgical and trauma algorithms as a management protocol for treating hemorrhage. Goal-directed coagulation management using fibrinogen concentrates and PCCs improved survival rates as compared with those predicted by the Trauma Injury Severity Score in a retrospective report of 131 patients.63 Another retrospective report included 601 patients receiving FFP without factor concentrates and noted greater transfusion requirements with RBCs or platelet concentrates compared with 80 trauma patients who received fibrinogen concentrate and/or PCC.71 A prospective evaluation of 144 patients with major blunt trauma also reported coagulation factor concentrates corrected coagulopathy and reduced RBC and platelet transfusion compared with those receiving FFP, and fewer patients developed multiorgan failure.72 However, overall mortality was not reduced with fibrinogen concentrates in another retrospective study of 294 trauma patients.73
Current European guidelines for managing bleeding in trauma patients with fibrinogen levels <1.5 to 2.0 g/L recommend an initial fibrinogen concentrate dose of 3 to 4 g, with further dosing guided by laboratory testing.20 There are additional studies underway, including prospective management protocols (Schöchl et al74 ) and 2 ongoing European trials of fibrinogen concentrates in trauma. However, multimodal approaches are important to consider, including the use of antifibrinolytic agents.
Cardiovascular surgery
Cardiovascular surgical patients bleed because of multiple coagulation defects associated with cardiopulmonary bypass (CPB), tissue injury, and dilutional changes.75 Multiple risk factors significantly influence bleeding including reoperation, type of surgical procedure (aortic root replacement, multiple valve replacements), CPB time, renal dysfunction, and factors unique to this patient population.76 Additionally, cardiac surgery patients have hemostatic changes consistent with disseminated intravascular coagulation, including elevated d-dimers, low fibrinogen, increased PT and PTT, thrombocytopenia, and low antithrombin levels. However, preoperative fibrinogen levels are reported to be an independent predictor of postoperative bleeding and transfusion requirement after coronary artery bypass grafting surgery.77 Preoperative fibrinogen concentrations <3 g/L are reported to increase perioperative blood loss and transfusion requirements after coronary artery bypass grafting.77
In a prospective, observational study of 1956 patients undergoing cardiac surgery, fibrinogen levels on ICU admission were lower in bleeding patients (2.5 ± 0.8 g/L and 2.1 ± 0.8 g/L in the control and excessive bleeding groups, respectively) and were a predictor of bleeding.78 Studies also suggest fibrinogen repletion will reduce bleeding and the need for allogeneic blood products.79 A prospective study of fibrinogen concentrates in 61 patients with bleeding post-CPB noted fibrinogen reduced transfusions compared with placebo (2 U vs 13 U, respectively), and transfusion avoidance was achieved in half of the patients.1 Other prospective and retrospective cardiac surgical studies, including high-risk ascending aortic replacement surgery, report that fibrinogen repletion with concentrates reduces postoperative bleeding and allogeneic blood product administration.34,40,64,79,80 Placebo controlled, randomized studies are currently underway to evaluate the role of fibrinogen repletion in major aortic surgery, and the results are eagerly awaited from a recently completed study (http://clinicaltrials.gov/show/NCT01475669). There is also a need to further evaluate several recent studies demonstrating significant reductions in bleeding and allogeneic transfusion using fibrinogen concentrates.
Obstetric hemorrhage
PPH is an important cause of maternal mortality and a growing focus for clinical trials.81,82 Following a comprehensive literature review, an expert panel defined severe persistent (ongoing) PPH as “active bleeding >1000 mL within the 24 hours following birth that continues despite the use of initial measures including first-line uterotonic agents and uterine massage.”83 Multiple studies report fibrinogen as an important predictor of PPH and of progression to severe PPH.25,26 Reduced levels of fibrinogen were associated with the progression of PPH in a cohort study of 356 women.27 Lower fibrinogen and FIBTEM A5 values were associated with more prolonged bleeds, need for invasive procedures, longer time in high dependency unit, and earlier transfusion, especially when FIBTEM was <10 mm or fibrinogen <2 g/L. In a study of 128 women with PPH requiring uterotonic prostaglandin infusion, 50/128 women had severe PPH defined by a hemoglobin drop of >4 g/dL, 4 or more RBC transfusions, need for surgical or arterial embolization procedure, or mortality.25 Patients with severe PPH had significantly lower fibrinogen and prolonged PT. Fibrinogen was the only laboratory value associated with severe PPH, and the risk was 2.63-fold higher for each 1-g/L decrease.25 The negative predictive value of fibrinogen >4 g/L was 79%, and the positive predictive value of ≤2 g/L was 100%. A case control study including 3 groups of women after a first pregnancy (severe PPH, nonsevere PPH, and asymptomatic controls; 317 in each group) observed that fibrinogen levels <2 g/L were independently associated with a significant risk of severe PPH.26 An additional report evaluating the specificity of fibrinogen levels <2 g/L for predicting severe PPH was ∼99%, and the odds ratio was ∼12.84 A prospective analysis for the need for embolization or surgical interventions for severe PPH on ICU admission reported that a fibrinogen level <2 g/L was an independent predicator.85 Additional analysis of 456 patients with PPH >1500 mL reported fibrinogen levels correlated with blood loss.86
Further studies in PPH report that fibrinogen concentrate therapy is important in patients with hypofibrinogenemia.6 Initial fibrinogen levels below 2 g/L in women with PPH are associated with more severe hemorrhage. In these emergency settings, fibrinogen concentrate allows rapid therapy without blood type matching; however, there are limited data and no published randomized clinical trials in this setting. The FIB-PPH trial investigated if early fibrinogen concentrate treatment reduced transfusions in PPH.87 This randomized, placebo-controlled, double-blind trial included patients after vaginal delivery with acute blood losses, as follows: ≥500 mL following manual removal of placenta; ≥1000 mL following manual exploration of the uterus postpartum; or a perioperative blood loss ≥1000 mL following Cesarean section. Patients received 2 g of fibrinogen concentrate or placebo and were monitored using standard coagulation tests. A reduction of allogeneic blood product administration was the primary end point. This study was completed in July 2013, and the results are eagerly awaited. A separate and ongoing trial (Fib2; EudraCT: 2012-005511-11) aims to establish whether giving fibrinogen concentrate reduces blood loss and the amount of allogeneic blood product administration compared with placebo.
Orthopedic surgery
Orthopedic surgery is associated with blood loss and risk of dilutional coagulopathy and impaired fibrin polymerization.88 In a prospective study of 66 patients, repletion with fibrinogen concentrate maintained clot firmness.89 In another study of children undergoing surgical craniosynostosis repair, repeated fibrinogen doses restored hemostasis without additional need for transfusions.90 In a similar study, using a ROTEM-assisted algorithm, factor concentrates reduced intraoperative transfusion requirements.91
Summary
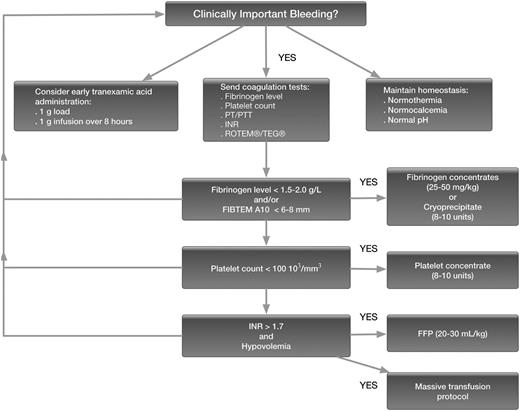
Fibrinogen is a critical hemostatic protein required for both prevention and treatment of bleeding. Fibrinogen levels can best be repleted with either cryoprecipitate (containing fibrinogen, factor VIII, von Willebrand factor, and FXIII) or a commercial fibrinogen concentrate. An increasing number of studies have examined the role of fibrinogen as a therapeutic target, for its use in acquired coagulopathies. Therapy in the bleeding patient should be multimodal to include repletion of other coagulation proteins, antifibrinolytic agents, and blood products including platelets and RBCs as needed.93-100 Fibrinogen concentrate represents an important option for treating coagulopathic bleeding, allowing reduction of allogeneic blood product transfusion. Further multicenter studies in a variety of clinical settings are needed to determine optimal dosing strategies and target thresholds for fibrinogen therapy. An algorithm with suggested management strategies for the bleeding patient with a focus on fibrinogen measurement and repletion strategies is included in Figure 1.
Fibrinogen algorithm. Suggested management strategy for the bleeding patient with a focus on fibrinogen measurement and repletion strategies.
Fibrinogen algorithm. Suggested management strategy for the bleeding patient with a focus on fibrinogen measurement and repletion strategies.
Authorship
Contribution: J.H.L. wrote and edited the manuscript; and L.T.G. reviewed and edited the manuscript.
Conflict-of-interest disclosure: J.H.L. serves on steering committees for CSL Behring, Boehringer-Ingelheim, and Grifols. L.T.G. is a consultant for CSL Behring and Octapharma.
Correspondence: Jerrold H. Levy, Duke University Medical Center, 2301 Erwin Rd, 5691H HAFS, Box 3094, Durham, NC 27710; e-mail: jerrold.levy@duke.edu.